INTRODUCTION
Cutaneous and soft tissue reconstruction in the region around the knee is often
challenging for the plastic surgeon and aimed at providing an acceptable
aesthetic appearance associated with good knee joint function1. A well-vascularized tissue is necessary
to ensure good wound healing, with local and free flaps among the surgical
options.
Local flaps are usually in or near the lesion and have limitations regarding the
size and length of the vascular pedicle, which is relatively small2. As for the free flaps, besides being a
more complex procedure in the reconstructive ladder of plastic surgery,
microvascular anastomosis technical difficulty due to the depth of the recipient
vessels3,4.
Surgery planning requires the simplest technique that will lead to wound closure,
with the minimum morbidity in the donor area5. The fasciocutaneous reverse anterolateral thigh (ALT) flap, which
was described first in 1990 by Zhang et al., seems to be an effective and
lasting option for the reconstruction of defects around the knee. It has a long
vascular pedicle and a large cutaneous portion1,4,5. Since then,
some studies have been published in the literature with success on the use of
the reverse ALT flap in the treatment of injuries around the knee; however, only
few reports have described its use in defects located in the popliteal
fossa6.
In this work, a series of cases of patients who underwent reconstruction with
fasciocutaneous reverse ALT flap for defects in the popliteal fossa, proximal
region, and leg is presented.
OBJECTIVE
To demonstrate the experience of the Reconstructive Plastic Surgery Service of
the Workers’ Hospital in Curitiba, Paraná, with lower limb reconstruction using
the reverse ALT thigh flap. This study aimed to verify the safety, versatility,
and reproducibility of this flap for the reconstruction of large wounds in the
regions of the lower thigh, knee, popliteal fossa, and proximal third of the
leg.
METHODS
All cases were selected from among reverse ALT thigh flap reconstructions
performed in the last 18 months in the plastic and reconstructive surgery
service. Of the 4 cases selected, 3 were for reconstruction of the popliteal
fossa and 1 was for reconstruction of the upper third of the leg. Follow-up for
2 to 18 months was conducted for the patients, and questions were asked about
the member function, aesthetics, and overall satisfaction with the procedure. In
addition, all surgical complications inherent to the procedure and other
interventions needed were discussed.
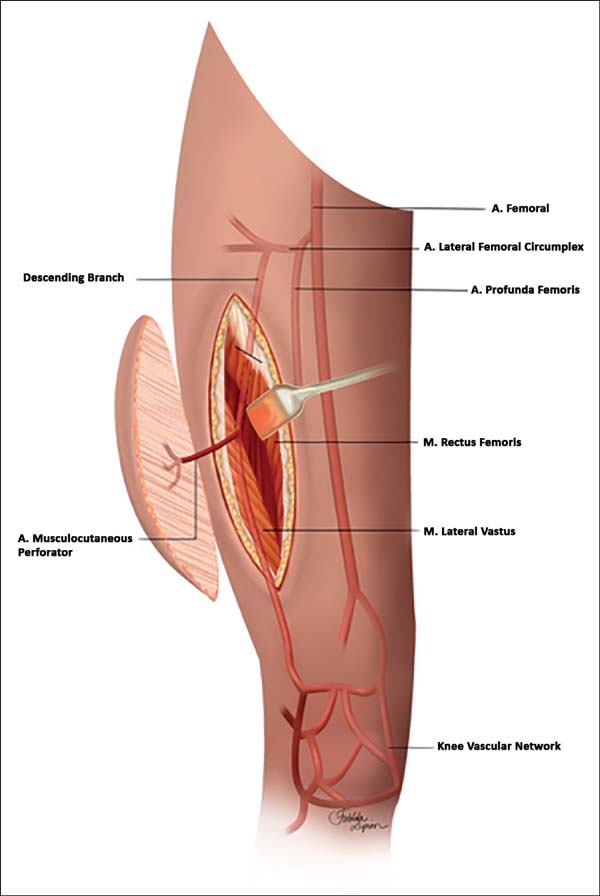
The technique of lifting the anterolateral flap of the reverse thigh was
performed as described in the following steps: 1. Marking of the donor area was
comprised of an ellipse of the previously debrided wound size in which the
center was comprised of the midpoint of a traced line between the anterior
superior iliac crest and the lateral border of the patella (Figure 1). 2. Incision of the medial portion of the
marking. 3. Medial-to-lateral subfascial dissection, locating the perforator of
the descending branch of the lateral femoral circumflex artery (LFCA). 4.
Incision of the lateral portion of the flap and detachment of the
fasciocutaneous flap. 5. Dissection of the perforator artery from the LFCA trunk
to the lateral superior genicular artery (LSGA). 6. Clamping and sectioning of
the proximal portion of the LFCA, with the flap fed by the LSGA. 7. Elaboration
of the subcutaneous tunnel in the knee region.
Figure 1 - Reverse anterolateral thigh flap. Schematic drawing.
Figure 1 - Reverse anterolateral thigh flap. Schematic drawing.
This study was approved by the ethics and research committee of the Worker’s
Hospital, with registration No. 69703617.9.0000.5225.
RESULTS
Case 1
A 24-year-old man fell from a 2-m height and incurred a tibial plateau
fracture, which was surgically treated with placement of two plates through
the posterior access, which evolved with infection and dehiscence of the
surgical wound. After 8 months of conservative treatment, use of an
anterolateral reverse thigh flap was proposed.
Physical examination revealed an unstable wound of 3 × 3 cm in size in the
popliteal fossa region with adjacent tissue contraction (Figure 2).
Figure 2 - Initial lesion of case 1.
Figure 2 - Initial lesion of case 1.
The surgery started with wound excision and debridement of the scar tissue
around it. The flap was released in accordance with the technique described
in our methodology. The flap was then transposed to the defect in the
popliteal fossa, passing through the subcutaneous tunnel created in the
medial knee region (Figure 3). The
donor area was closed primarily and a cast-splint was placed, keeping the
knee in extension to prevent bending of the vascular pedicle. In the
immediate and 10-month postoperative periods, the area had a good appearance
(Figures 4 and 5).
Figure 3 - Mobilization of the flap in case 1.
Figure 3 - Mobilization of the flap in case 1.
Figure 4 - Final result of case 1.
Figure 4 - Final result of case 1.
Figure 5 - Appearance of case 1 10 months after operation.
Figure 5 - Appearance of case 1 10 months after operation.
Case 2
A 30-year-old woman with a history of exposed fracture of the proximal tibia
was treated with Ilizarov external fixation, which resulted in a large scar
retraction and unstable wound that limited the complete flexion of the left
leg.
The physical examination revealed an unstable wound of 2.5 × 2.5 cm in size
in the anterolateral proximal leg region (Figure 6). Thus, reconstruction of the region was planned with a
reverse ALT flap.
Figure 6 - Anterior view of the initial lesion of case 2.
Figure 6 - Anterior view of the initial lesion of case 2.
Surgery was started with the dissection and location of the LSGA once the
patient had retraction in the anatomical region of the LSGA, which was then
followed by wound excision and debridement of the surrounding scar tissue.
The next steps were as described in the methodology, with only one
difference. In this case, elaboration of tunnel was not necessary for the
pedicle, as the incision was in communication with wound resection. At the
end of the procedure, a suction drain was placed in the donor and recipient
areas. The final appearance was good (Figure 7).
Figure 7 - Final result of case 2.
Figure 7 - Final result of case 2.
Case 3
A 40-year-old woman had a history of resection of a liposarcoma in the right
popliteal region, complemented by post-resection radiotherapy, which evolved
with a large chronic wound and local radiodermatitis for a period of 3
years.
Physical examination revealed an unstable 7 × 4cm wound in the right
popliteal fossa (Figure 8). Hence,
reconstruction of the region was planned with a reverse anterolateral thigh
flap (Figure 9).
Figure 8 - Posterior view of the initial lesion in case 3.
Figure 8 - Posterior view of the initial lesion in case 3.
Figure 9 - Marking of the flap in case 3.
Figure 9 - Marking of the flap in case 3.
Marking of the donor area and flap release followed the steps described in
the methodology. In this case, the anatomical variation made the artery
dissection difficult because the LFCA perforator that nourished the flap had
a proximal origin. Thus, the level of ligature was almost at the emergence
of the deep femoral artery. After confirmation of adequate retrograde flux
of the LSGA, the proximal ligation of the LFCA was safely conducted. Next,
excision of the chronic wound with the radiodermatitis area (Figure 10) was performed, and the flap
transposed to the defect of the popliteal fossa, passing through a
subcutaneous tunnel created in the lateral region of the knee (Figures 11 and 12). The wound and donor areas had a pleasing final
appearance (Figures 12 and 13) at 3 months after operation (Figure 14).
Figure 10 - Marking of the initial lesion and posterior view of case
3.
Figure 10 - Marking of the initial lesion and posterior view of case
3.
Figure 11 - Release of the flap in case 3.
Figure 11 - Release of the flap in case 3.
Figure 12 - Final appearance of the lesion in case 3.
Figure 12 - Final appearance of the lesion in case 3.
Figure 13 - Final appearance of the donor area in case 3.
Figure 13 - Final appearance of the donor area in case 3.
Figure 14 - Appearance 3 months after operation in case 3.
Figure 14 - Appearance 3 months after operation in case 3.
Case 4
A 35-year-old male patient presented a large fibrosarcoma on the right
popliteal fossa, with infiltration of noble structures.
Physical examination revealed a large tumor in the right popliteal fossa of
10 × 10 cm in size, fixed to the depth. Magnetic resonance imaging of the
right knee detected an invasion of the common fibular nerve, posterior joint
knee capsule, and medial and lateral heads of the gastrocnemius muscle of
the right lower limb. No invasion of the popliteal artery or lateral
genicular arteries was identified. Therefore, tumor resection with
reconstruction of the region with reverse anterolateral thigh flap was
planned.
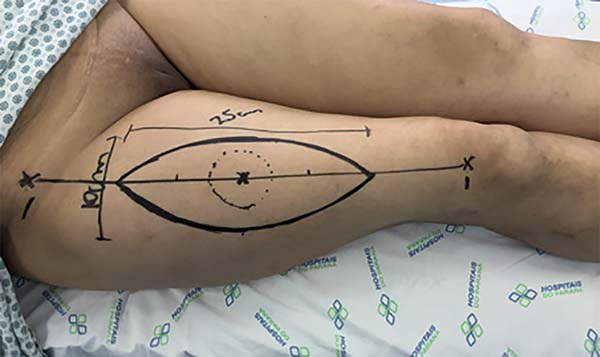
The marking of the donor area was comprised of a spindle-shaped area to be
resected (Figure 15). The oncological
surgeon began surgery with a wide resection with safety and tumor-free
margins. The resection went deep into the posterior joint capsule of the
knee, encompassing 15 cm of the common fibular nerve and insertion of the
medial and lateral heads of the gastrocnemius muscle (Figure 16).
Figure 15 - Marking of the flap in case 4.
Figure 15 - Marking of the flap in case 4.
Figure 16 - Lesion after debridement and posterior view of case
4.
Figure 16 - Lesion after debridement and posterior view of case
4.
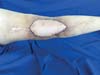
Next, the popliteal fossa reconstruction was started, with dissection of the
sural nerve for microsurgical graft and nerve reanastomosis with
interposition of the common fibular nerve graft. The nerve suture performed
was epineural with the use of fibrin glue. Once the nerve graft was
performed, dissection of the reverse ALT flap was started, following the
technique described in the methodology (Figure 17).
Figure 17 - 14 days post-operative of case 4.
Figure 17 - 14 days post-operative of case 4.
Patients 1 to 4 were followed up for 18, 11, 4, and 2 months. The only
complication occurred in case 2, which had a postoperative hematoma in 15%
of the flap area. The debrided flap was subsequently grafted successfully.
In case 1, thinning of the flap with liposuction was performed. In cases 3
and 4, no other interventions were needed.
Regarding limb function and resolution of the baseline problem, all the cases
showed good results. From the aesthetic point of view, the only case that
required reconsideration was case 2, which led to the patient’s complaint of
an aesthetic impairment. Finally, the patients were questioned on the
overall outcome of their procedures, all of whom were satisfied.
DISCUSSION
The knee and fossa popliteal region have inherent characteristics that can make
even a small wound a challenge. Defects of the soft parts of this region may be
accompanied by exposed bone or tendon, in addition to limitation in the range of
joint knee movement1.
The cutaneous aspect of the anterolateral thigh region has an excellent vascular
communication network, which allows the elevation of large ALT flaps with only
one good-caliber perforator7.
Consequently, the reverse ALT flap is a well-established option for defects in
the knee region and has grown in popularity8.
The vascular base of this flap is the anastomosis between the descending branch
of the LFCA and LSGA, which is located approximately 3 to 10 cm above the
lateral border of the patella. This connection maintains a constant cutaneous
perfusion through a retrograde blood flow, which was clearly described by Pan et
al.6, which is enough for flap
survival (Figure 1).
The reverse ALT flap has many advantages as follows: 1. long pedicle, large
caliber, and enough blood supply; 2. large size and range of arc rotation; 3.
The thickness of the flap is thinner than that of the muscle cutaneous flap; and
4. small morbidity of the donor area.4,9
Among the inconveniences described in this procedure are the risk of venous
congestion due to long retrograde flow and arterial impairment due to
compression or kinking of the pedicle4,
which occurred in only one case (case 2) due to hematoma under the flap. In all
the other cases, no complications occurred.
As it is a fasciocutaneous flap and allows primary closure of the donor area, the
reverse ALT flap generates a purely aesthetic sequela. Another flap option to be
used in the reconstruction of lesions of this region is the gastrocnemius muscle
flap, which ends up generating a functional sequela of the limb.
Free flaps are also another option for reconstruction of this region, but to
create these flaps, a highly specialized professional is needed, as well as
specific materials such as a surgical microscope, which is often an unfeasible
option in economically disadvantaged regions. Although the technique of
detachment of the reverse ALT flap is laborious, no special material is needed
to make this flap. Hence, it can be created even in regions with few resources,
sparing the need for a microsurgery.
CONCLUSION
On the basis of the above-mentioned findings, the reverse ALT flap showed to be a
viable reproducible option, presenting good functional and aesthetic results
that are suitable for cutaneous and soft tissue reconstructions in the popliteal
fossa, knee, and upper leg regions.
COLLABORATIONS
|
GSSJ
|
Author’s contribution: analysis and/or data interpretation;
conception and design study; data curation; final manuscript
approval; methodology; project administration; realization of
operations and/or trials; validation; writing - original draft
preparation; writing - review & editing.
|
|
RSF
|
Author’s contribution: analysis and/or data interpretation;
conception and design study; data curation; final manuscript
approval; methodology; project administration; writing - original
draft preparation; writing - review & editing.
|
|
JRN
|
Author’s contribution: analysis and/or data interpretation;
conception and design study; data curation; final manuscript
approval; methodology; project administration; writing - original
draft preparation; writing - review & editing.
|
|
AGM
|
Author’s contribution: analysis and/or data interpretation;
conception and design study; data curation; final manuscript
approval; formal analysis; methodology; project administration;
writing - original draft preparation.
|
|
DRP
|
Author’s contribution: analysis and/or data interpretation;
conception and design study; data curation; final manuscript
approval; formal analysis; methodology; project administration;
writing - original draft preparation.
|
|
RFRM
|
Author’s contribution: analysis and/or data interpretation;
conception and design study; data curation; final manuscript
approval; formal analysis; methodology; project administration;
writing - original draft preparation.
|
|
VRS
|
Author’s contribution: analysis and/or data interpretation;
conception and design study; data curation; final manuscript
approval; formal analysis; methodology; project administration;
writing - original draft preparation.
|
|
ABP
|
Author’s contribution: analysis and/or data interpretation;
conception and design study; data curation; final manuscript
approval; formal analysis; methodology; project administration;
writing - original draft preparation.
|
REFERENCES
1. Demirseren ME, Efendioglu K, Demiralp CO, Kilicarslan K, Akkaya H.
Clinical experience with a reverse-flow anterolateral thigh perforator flap for
the reconstruction of soft-tissue defects of the knee and proximal lower leg. J
Plast Reconstr Aesthet Surg. 2011;64(12):1613-20.
2. Sahin I, Guzey S, Aykan A, Nisanci M. The Reverse Fasciocutaneous
ALT Flap Harvested From Deeply Wounded and Scarred Area for Reconstruction of
the Knee: A Case Report. Int J Low Extrem Wounds.
2016;15(2):136-8.
3. Wang XC, Lu Q, Li XF, Burd A, Zhao BC, Wang YY, et al. Reversed
anterolateral thigh adipofascial flap for knee and proximal calf defects. Burns.
2008;34(6):868-72.
4. Sadigh PL, Wu CJ, Shih HS, Jeng SF. Reverse Anterolateral Thigh Flap
to Revise a Below-knee Amputation Stump at the Mid-tibial Level. Plast Reconstr
Surg Glob Open. 2014;1(9):e88.
5. Zhang G. Reversed anterolateral thigh island flap and myocutaneous
flap transplantation. Zhonghua Yi Xue Za Zhi.
1990;70(12):676-8.
6. Pan SC, Yu JC, Shieh SJ, Lee JW, Huang BM, Chiu HY. Distally based
anterolateral thigh flap: an anatomic and clinical study. Plast Reconstr Surg.
2004;114(7):1768-75.
7. Saint-Cyr M, Wong C, Schaverien M, Mojallal A, Rohrich RJ. The
perforasome theory: vascular anatomy and clinical implications. Plast Reconstr
Surg. 2009;124(5):1529-44.
8. Liu TY, Jeng SF, Yang JC, Shih HS, Chen CC, Hsieh CH. Reconstruction
of the skin defect of the knee using a reverse anterolateral thigh island flap:
cases report. Ann Plast Surg. 2010;64(2):198-201.
9. Zhou G, Zhang QX, Chen GY. The earlier clinic experience of the
reverse-flow anterolateral thigh island flap. Br J Plast Surg.
2005;58(2):160-4.
1. Hospital do Trabalhador de Curitiba, Curitiba,
PR, Brazil.
2. Universidade Federal do Paraná, Curitiba, PR,
Brazil.
Corresponding author: Guataçara Schenfelder Salles-Junior, Avenida
Republica Argentina, nº 4406 - Novo Mundo, Curitiba, PR, Brazil, Zip Code:
81050-000. E-mail: guatajr@yahoo.com.br
Article received: April 8, 2018.
Article accepted: October 1, 2018.
Conflicts of interest: none.