INTRODUCTION
Tissue expansion is the technique that allows the reconstruction of defects by
the gradual distension of a flexible skin area, preparing it for use in solving
any defect such as breast reconstruction, burns, and giant nevi1. This reconstructive method has advantages
such as the use of tissues of color and texture similar to the defect, less
damage to the donor area, and aesthetic improvement.
In burns, tissue expansion is indicated when the wounds have completely healed,
and the resulting scars need to be treated. Patients with burn sequelae may have
limited tissue availability for flaps. Specific areas such as the scalp benefit
from tissue expansion by allowing the treatment of sequelae with similar
tissue2 (Figure 1), as well as the head and neck region. The expansion can be
done in tissues surrounding the wound, or donor areas of free flaps in
situations that nearby regions are not available3.
Figure 1 - Patient with an area of alopecia on the scalp due to the burn
submitted to treatment with tissue expander. A.
Preoperative period; B. Final result after three-stage
treatment with round type expanders.
Figure 1 - Patient with an area of alopecia on the scalp due to the burn
submitted to treatment with tissue expander. A.
Preoperative period; B. Final result after three-stage
treatment with round type expanders.
Giant congenital nevus can be defined as an ectopic concentration of melanocytes
of neuroectodermal origin with a diameter greater than 20 cm and affecting about
1 in every 20,000 live births4. Besides
the aesthetic implications, patients with this type of anomaly need to deal with
5 to 12% associated risk of malignancy. Therefore, prophylactic excision is
recommended4. The use of tissue
expanders is frequent in this treatments5.
The number of procedures involving skin expanders for breast reconstruction has
also been increasing. Statistics from the American Society of Plastic Surgeons,
in 20166, show that approximately 90% of
breast reconstructions with prostheses are performed in two stages, the first
of
which is tissue expansion (Figure 2). The
use of expanders may also be required in breast agenesis. In Poland’s syndrome,
there is a partial or total absence of the pectoralis major, pectoralis minor,
serratus and breast muscles, and the nipple-areola complex; therefore, expansion
is one of the techniques used in its treatment7
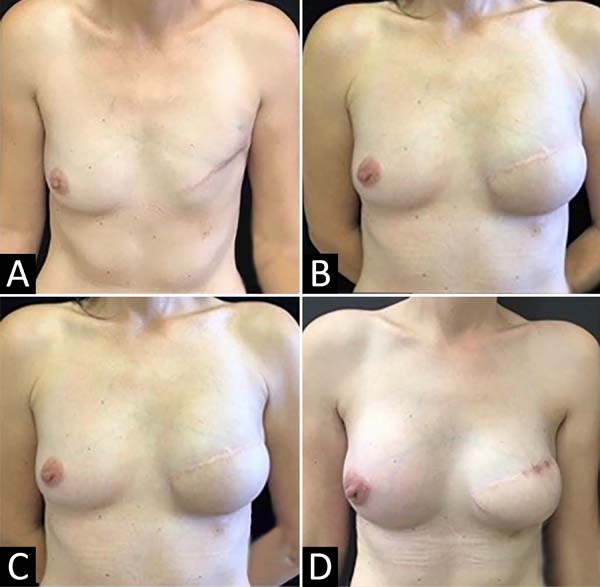
Figure 2 - Patient undergoing treatment for left breast for ductal carcinoma
in situ. Late breast reconstruction was performed with a large
dorsal flap and a round, smooth expander with a remote valve. After
six months, and after the expansion was completed, she was replaced
with an expander for prosthesis and symmetrization with a zigzag
periareolar augmentation mammoplasty. A. Preoperative
period; B. Result after placing the expander;
C. Result after replacing the expander with the
prosthesis; D. Final result.
Figure 2 - Patient undergoing treatment for left breast for ductal carcinoma
in situ. Late breast reconstruction was performed with a large
dorsal flap and a round, smooth expander with a remote valve. After
six months, and after the expansion was completed, she was replaced
with an expander for prosthesis and symmetrization with a zigzag
periareolar augmentation mammoplasty. A. Preoperative
period; B. Result after placing the expander;
C. Result after replacing the expander with the
prosthesis; D. Final result.
OBJECTIVE
This article has as main objective to report the experience of the plastic
surgery service at the Hospital de Clínicas of the Federal University of Paraná
(UFPR) with the use of expanders, emphasizing the complications found, their
possible causes and management.
METHODS
This is a retrospective, descriptive, and analytical study of patients who
underwent tissue expansion for reconstructive surgery at Hospital de Clínicas
da
UFPR. This study was submitted and approved by the Ethics and Research Committee
of the Hospital de Clínicas da UFPR (approval number: 68550217.4.0000.0096).
Medical records of patients who underwent expansion between January 2010 and
December 2016 were analyzed. All patients who underwent surgery for tissue
expansion during this period were included. Exclusion criteria included the
abandonment of treatment and the death of the patient during this period. The
data obtained were age, gender, pathology indicative of the procedure, type of
expander, insertion site, evolution, and complications.
From the data obtained, a descriptive statistical analysis was carried out,
emphasizing the relationship between the complications found and parameters,
such as the cause of treatment, the format of the expander, and the insertion
site.
RESULTS
Sixty-one patients and 80 surgeries, including reexpansion procedures, were
analyzed. The majority of patients were female (83.6%). The age at the first
surgical stage of the patients analyzed was between 2 and 73 years (mean 31),
with the majority in the age group above 40 years (41%), followed by young
people between 11 and 20 years (27.9%). The main indication for surgery was
breast reconstruction after mastectomy (36%), followed by a burn scar correction
(31.1%) and giant nevi correction (14.7%). Other causes include post-trauma scar
correction (6.6%), vascular malformation correction (4.9%), breast agenesis due
to Poland’s syndrome (3.3%), microtia (1.6%), and resection of dermofibrosarcoma
(1.6%).
Concerning the complications most seen in the procedures performed, signs of
infection (14.7%) stand out. Other complications observed were: suture
dehiscence (3.2%), seroma (3.2%), expander defect (3.2%), expander exposure
(3.2%), necrosis (1.6%) and signs of hypoperfusion (1.6%).
Patients undergoing breast reconstruction had the highest number of
complications. Considering the 22 patients who received treatment, four
presented, in the first stage, infectious signs in the breast where the expander
was placed, and another four presented the following complications each:
exposure of the expander, dehiscence of the suture, seroma and signs of
hypoperfusion. In five cases, it was necessary to remove the expander. Patients
suffering from seroma, and exposure only needed to relocate the expanders. One
of the patients died due to cancer complications.
Among patients undergoing expansion to correct burns, two showed signs of
infection after surgery. Two others presented complications due to suture
dehiscence and one due to defect in the expander. They all required the removal
of the expander. Forty percent of the complications in patients with burn
sequelae were in the lower limbs. The other correlations between the cause of
treatment and the percentage of complications are shown in Table 1.
Table 1 - Indications for expansion surgery and number of complications *.
| Etiology |
Number of patients |
% Total |
Number of complications |
% Complications |
| Breast reconstruction |
22 |
36 |
9 |
40.1 |
| Burn sequel |
19 |
31.1 |
5 |
26.3 |
| Giant Nevus |
9 |
14.7 |
3 |
33.3 |
| Post-trauma scar sequel |
4 |
6.6 |
1 |
25.0 |
| Vascular malformation |
3 |
4.9 |
1 |
33.3 |
| Poland syndrome |
2 |
3.3 |
1 |
50.0 |
| Dermatofibrosarcoma resection |
1 |
1.6 |
1 |
100.0 |
| Microtia |
1 |
1.6 |
0 |
0 |
Table 1 - Indications for expansion surgery and number of complications *.
The chest region was associated with a higher number of complications than other
parts of the body: 11 of the 28 patients who underwent the procedure in this
region had some type of complication. The other correlations between the
anatomical region submitted to expansion and complications are shown in Table 2.
Table 2 - Anatomical region submitted to expansion and number of complications
*.
| Anatomical region |
Number of patients |
% Total number of patients |
Number of complications |
% |
| Complications |
|
|
|
|
| Chest |
28 |
45.9 |
11 |
39.3 |
| Lower limbs |
9 |
14.8 |
3 |
33.3 |
| Scalp |
9 |
14.8 |
2 |
22.2 |
| Face |
8 |
13.1 |
2 |
25.0 |
| Back |
7 |
11.5 |
1 |
14.3 |
| Abdomen |
2 |
3.3 |
0 |
0 |
| Upper limbs |
1 |
1.6 |
0 |
0 |
| Neck |
1 |
1.6 |
1 |
100.0 |
Table 2 - Anatomical region submitted to expansion and number of complications
*.
Regarding age, the greatest number of complications occurred in patients over 40
years of age. In this group, 36% had some type of complication (Table 3).
Table 3 - Distribution of patients by age and number of complications.
| Age (years) |
Number of patients |
% Total |
Number of complications |
% of Complications |
| 0-10 |
9 |
14.8 |
3 |
33.3 |
| 11-20 |
17 |
27.9 |
5 |
29.4 |
| 21-30 |
6 |
9.8 |
0 |
0 |
| 31-40 |
4 |
6.6 |
1 |
25.0 |
| >40 |
25 |
41.0 |
9 |
36.0 |
Table 3 - Distribution of patients by age and number of complications.
Reexpansion was necessary for 37.7% of patients. Of the 19 surgeries performed on
these patients for reexpansion, two had complications. One of the patients who
underwent breast reconstruction showed signs of infection, while the second
surgery of a patient with a giant nevus had the expander’s exposure.
The majority of patients started the expansion during the intraoperative period
(95%), and the time of evolution varied from 0 to 168 months, with an average
of
58.9 months.
Table 4 shows the number of complications
concerning the year.
Table 4 - Distribution of cases concerning the year and the number of
complications *.
| Year of surgery |
Number of surgeries |
Number of complications |
% of complications |
| 2010 |
8 |
3 |
37.5 |
| 2011 |
11 |
2 |
18.2 |
| 2012 |
17 |
4 |
17.6 |
| 2013 |
17 |
4 |
23.5 |
| 2014 |
14 |
3 |
21.4 |
| 2015 |
7 |
2 |
28.6 |
| 2016 |
6 |
3 |
33.3 |
| Total |
80 |
21 |
|
Table 4 - Distribution of cases concerning the year and the number of
complications *.
DISCUSSION
In the mid-1950s, Neumann was the first surgeon to use an expander implant
through a latex balloon to enlarge the periauricular region after an ear
trauma8. Since then, skin expanders
have been used for the most diverse procedures.
In terms of shape, an expander follows three patterns: round, rectangular, and
semi-lunar (croissant). The rectangular is known for allowing additional tissue
expansion, thus increasing the options for flap design. The valve can be
integrated into the expander or attached via a silicone tube.
The content of the expanders available on the market is almost always a saline
solution. Another option found is filling with carbon dioxide, recently approved
by the “US - Food and Drug Administration (FDA)” 9.
In the Plastic Surgery Service of Hospital de Clínicas da UFPR, the three types
of expanders are used, the round one being recommended in breast reconstructions
and the croissant and rectangular types most used in other types of surgery,
such as treating burn sequelae, for example. The contents of these expanders
have always been a saline solution.
A critical point to be defined in the preoperative period is the expansion
design. Attention should be paid to the donor site as infections, trauma, and
unstable scarring can lead to implant failure or extrusion. The incision site
must also be chosen with caution. For example, if the goal is to remove an
injury, it is appropriate to position the incision at the edges of the
injury.
The majority of expansions begin during the intraoperative period, when a volume
is placed making a slight compression to avoid the hematoma formation, since
in
most cases - except for breast reconstruction - a vacuum suction drain is not
used. Although there are many citations in the literature to start the expansion
in one to three weeks after the expander is inserted, in our service, the scar
is expected to mature more, and tissue expansion begins in about four weeks.
If
there are no complications, weekly expansion is performed, until the required
volume is reached. The use of state-of-the-art or osmotic expanders with
self-inflating expansion may eliminate the need for repeated injections,
reducing the number of infections and other complications10. However, there are still no such devices commercially
available in our market11.
The profile of patients, the number of surgeries, and the number of complications
have changed in our department in recent decades if we compare it with a study
by Freitas et al., from 2011. In the period from January 2005 to December 2009,
most of these patients were in their second decade of life and underwent
expansion due to burning sequelae. In the present study, we found a prevalence
of women over the fourth decade of life undergoing breast reconstruction
treatment after radical mastectomy, with the old profile of patients in the
second position. This change in profile is consistent with the worldwide
increase in the number of breast reconstruction procedures with prostheses
performed in two stages, the first of which is tissue expansion6. In proportion to the number of surgeries
performed in the last decades12, the
number of complications has decreased.
In patients undergoing radical mastectomy for cancer treatment, a significant
challenge is a need for post-surgical radiation. Radiation leads to fibrosis,
which compromises the quality of the skin and subcutaneous tissue, resulting
in
higher incidences of complications and possibly impairing the final aesthetic
result13. These complications may
conduct to the need of the radiotherapy treatment interruption, thus
compromising the final result. In other situations, it may be necessary to
deflate the expander to allow adequate access to the chest wall and internal
mammary lymph nodes.
In burns, the most common complications are infection, exposure, and expander
malfunction. According to Bozkurt et al., N 200814, the highest number of complications in these patients occurs in
the head region, and when using larger expansion volumes (400 and 800ml).
However, the results obtained in this research are in line with LoGiudice and
Gosain (2003)15, with more significant
complications in the lower limbs, possibly due to less rich vascularization and
the amount of tissue available region.
The highest incidence of complications with the age group is found in patients
over 40 years old and those between 11 to 20 years old, coinciding with the age
groups with the highest prevalence in patients after radical mastectomy and burn
sequelae.
It is essential to know the types of complications, frequency, and associated
factors to minimize them. Besides, the choice of the best expander option and
the correct surgery technique and expansion are essential for a good result.
The
future of the skin expansion technique is auspicious. The increase in the number
of studies observed in the last decades on expansion, not only of skin but also
of nerves, bones, and other parts of the body, can be of great value to surgeons
in the future16.
CONCLUSION
The skin expansion technique is indicated for several pathologies’ treatment.
Besides, the patient profile treated at the Hospital de Clínicas da UFPR has
changed in the last decades. Since 2010, there has been an increase in the
number of patients who underwent treatment for breast reconstruction, exceeding
the number of patients due to burning sequelae who underwent the same procedure.
Most of the complications observed in these patients were infections related
to
the insertion of expanders in the chest region to perform the breast
reconstruction procedure.
REFERENCES
1. Di Mascio D, Castagnetti F, Mazzeo F, Caleffi E, Dominici C.
Overexpansion technique in burn scar management. Burns. 2006
Jun;32(4):490-8.
2. Tavares Filho JM, Belerique M, Franco D, Porchat CA, Franco T.
Tissue expansion in burn sequelae repair. Burns. 2007
Abr;33(2):246-51.
3. Barret JP. ABC of burns: burns reconstruction. BMJ.
2004;329(7460):274-6.
4. Paschoal FM. Nevo melanocítico congênito. An Bras Dermatol. 2002
Nov/Dez;77(6):649-58.
5. Viana ACL, Gontijo B, Bittencourt FV. Giant congenital
melanocytic nevus. An Bras Dermatol. 2013 Nov/Dez;88(6):863-78.
6. American Society of Plastic Surgeons (ASPS). Plastic surgery
statistics [Internet]. Arlington Heights, IL: ASPS; 2016; [acesso em 2017 Abr
01]. Disponível em:
https://www.plasticsurgery.org/news/plastic-surgery-statistics?sub=2016+Plastic+Surgery+Statistics
7. Araujo MP, Araujo AJ. Sindrome de Moebiüs-Poland: relato de caso.
Rev Med. 1999;78(3):371-7.
8. Ashley KL, Bruce SB. Tissue expansion. In: Thorne CH, ed. Grabb
and Smith’s Plastic Surgery. Philadelphia, PA: Lippincott Wilians Wilkins; 2013.
p. 512-40.
9. Ascherman JA, Zeidler K, Morrison KA, Appel JZ, Berkowitz RL,
Castle J, et al. Carbon dioxide-based versus saline tissue expansion for breast
reconstruction: results of the XPAND prospective, randomized clinical trial.
Plast Reconstr Surg. 2016 Dez;138(6):1161-70.
10. Chummun S, Addison P, Stewart KJ. The osmotic tissue expander: a
5-year experience. J Plast Reconstr Aesthet Surg. 2010
Dez;63(12):2128-32.
11. Pitanguy I, Radwanski HN, Amorim NFG, Lintz JE, Moraes Neto AEM.
The use of tissue expanders in burn sequelae. Acta Med Misericordia.
2000;2(3):59-64.
12. Freitas RS, Oliveira e Cruz GA, Scomação I, Nasser IJG, Colpo
PG. Tissue expansion at Hospital de Clínicas-UFPR: our experience. Rev Bras Cir
Plást. 2011 Set;26(3):407-10.
13. Nano MT, Gill PG, Kollias J, Bochner MA, Malycha P, Winefield
HR. Psychological impact and cosmetic outcome of surgical breast cancer
strategies. ANZ J Surg. 2005 Nov;75(11):940-7.
14. Bozkurt A, Groger A, O’Dey D, Vogeler F, Piatkowski A, Fuchs
PCH, et al. Retrospective analysis of tissue expansion in reconstructive burn
surgery: evaluation of complication rates. Burns.
2008;34(8):1113-8.
15. LoGiudice J, Gosain AK. Pediatric tissue expansion: indications
and complications. J Craniofac Surg. 2003 Nov;14(6):866-72.
16. Wood RJ, Adson MH, Van Breek AL, Peltier GL, Zubkoff MM, Bubrick
MP. Controlled expansion of peripheral nerves: comparison of nerve grafting and
nerve expansion/repair for canine sciatic nerve defects. J Trauma. 1991
Mai;31(5):686-90.
1. Hospital de Clínicas, Federal University
of Paraná, Curitiba, PR, Brazil.
Corresponding author: Kethelyn Keroline Telinski Rodrigues
Avenida Presidente Getúlio Vargas ,1811, Apart. 41 , Rebouças, Curitiba, PR,
Brazil. Zip Code: 80240-040, E-mail:
kety.rodrigues@gmail.com
Article received: March 03, 2020.
Article accepted: July 15, 2020.
Conflicts of interest: none.