INTRODUCTION
The surgical flap consists of a tissue mobilized from one part of the body to
another with a vascular peduncle and can be kept intact or sectioned, to perform
vascular anastomosis and maintain the blood supply of that tissue. These can
be
classified according to the composition of the tissue found in it (cutaneous,
musculocutaneous, fasciocutaneous, osteocutaneous and sensory), and according
to
the movement of the skin towards the receptor area (advance, rotation,
transposition, and interpolation)1,2.
They are a choice to reconstruct a defect on vital structures, tissues devoid of
a perivascular membrane, or implants.
To improve their surgical skills, medical students seek to expand their
theoretical knowledge through observation and practice in operating rooms3,4.
However, this learning vehicle has become a restricted alternative due to the
increased demand to surgeons for greater effectiveness, seeking to reduce
surgical time and, consequently, the time available for teaching; in addition
to
ethical conflicts that may arise by allowing the student to practice them in
the
patient, because of the concept of non-maleficence3.
Given these difficulties, practical models were elaborated to allow their use
outside the operating room and resemble human tissue. According to the material
used for its manufacture and its purpose, these are classified as high,
intermediate, and low fidelity. However, many of these have high costs,
difficult access, and ethical complications, making them unfeasible for
practice5,6.
Thus, low-cost and synthetic models for the training of surgical techniques, such
as the skin flap, are a relevant tool and can present positive results regarding
the facilitation of the teaching and learning process of a complex theme, such
as surgery. Allowing not only a more effective fixation of theoretical content
but improving practical skills so that ethical principles are preserved.
OBJECTIVE
The present work aims to present a synthetic model that is unpublished and
practical for the training of skin flap techniques.
METHODS
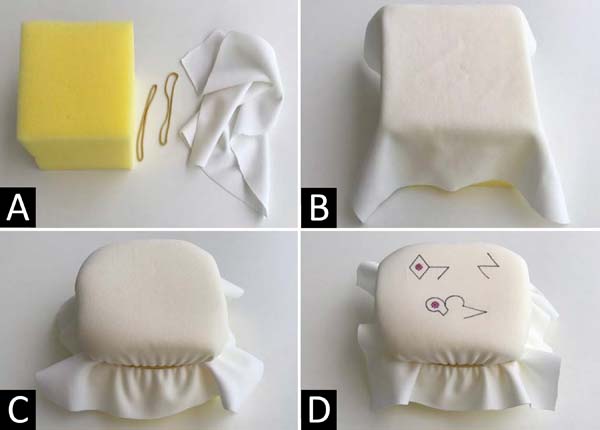
Its construction is made from the following components (Figure 1): 1) 24cm2 of mesh fabric (96%
polyester, 4% elastane); 2) car wash sponge (11x13x6cm); 3) latex rubber bands;
4) fine-tipped permanent brush; 5) scalpel (handle # 3, blade # 15); 6) 3-0
nylon threads; 7) surgical suture instruments (needle holder, mouse-tooth
forceps and scissors).
Figure 1 - Demonstration of the material needed to construct the
model.
Figure 1 - Demonstration of the material needed to construct the
model.
The assembly consists of covering one of the sponge surfaces with fabric to
simulate the skin and the subcutaneous sponge. Besides, in order to have the
fabric fixed on the sponge, latex elastics are used for this fixation, remaining
immobile and slightly stretched (Figures 2A, 2B, and 2C).
Figure 2 - Demonstration of the model construction steps. A.
Sponge block, rubber bands and mesh fabric; B.
Positioning the fabric on the sponge; C. Fixing the
fabric to the sponge with the latex elastic; D. Model
duly ready and with the flap markings to be made.
Figure 2 - Demonstration of the model construction steps. A.
Sponge block, rubber bands and mesh fabric; B.
Positioning the fabric on the sponge; C. Fixing the
fabric to the sponge with the latex elastic; D. Model
duly ready and with the flap markings to be made.
After assembly, the fine-tipped brush is used to draw on the fabric’s surface the
type of flap to be made. Finally, the model can already be used to train the
various techniques described using the appropriate surgical instruments (Figure 2D).
Thus, the model mentioned above was made with a maximum cost of 10 reais and
simulates this procedure’s technique. It is worth mentioning that the fabric
is
the only component that cannot be reused after use, and that needs
replacement.
The model was made at the University of Fortaleza (UNIFOR) by the university’s
academic league of plastic surgery in January 2019. Moreover, the study
mentioned above did not specify the involvement of humans and animals, so there
was no need for approval by the Ethics Committee to prepare the skin flap model,
which is obtained through synthetic materials.
The model was used in extracurricular activities elaborated by the academic
league of plastic surgery of the university; the activities took place in a
4-hour shift under the supervision of academic members of the academic league
who had teaching guidance.
RESULTS
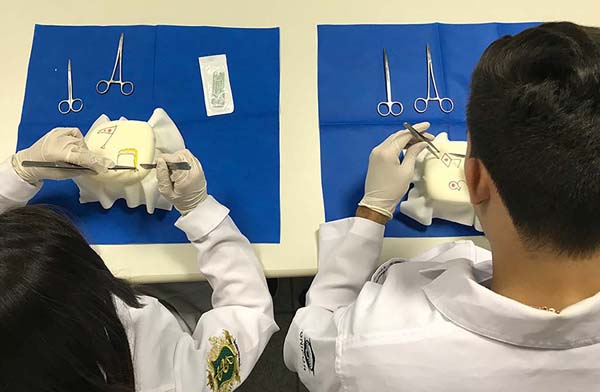
The model was used in the event of the academic surgical leagues of a Private
University of Fortaleza/CE, in which students from various school periods,
approximately 50 students, had contact with the proposed model (Figure 3).
Figure 3 - Practice of performing the skin flap using the proposed
model.
Figure 3 - Practice of performing the skin flap using the proposed
model.
The model presented satisfactory results in the simulation of the skin flap
technique. The fabric, although limited in the simulation of human skin
consistency, demonstrated good elasticity and tensile strength, allowing the
improvement of surgical instrumentation manipulation and knowledge of principles
and practice of procedure. Besides, it allowed the development of skills also
by
the instructor students, such as interpersonal communication.
It is added that the presence of students more experienced and trained by the
teacher, contributed to the elaboration of a less hostile environment for
learning, facilitating the clarification of doubts in a simple and accessible
language.
DISCUSSION
During the medical career, most surgical practices are restricted to the hours
destined to general surgery and are often insufficient for academics interested
in the surgical field. Regarding plastic surgery, there is a lack of treatment
for essential themes in this area, such as the cutaneous flap7.
Microsurgery is an area of paramount importance in the plastic surgeon
curriculum. Many models that allow the practice of this flap have already been
developed and tested, demonstrating efficacy in the development of skills in
microsurgery. According to the systematic review of non-biological models by
Abi-Rafeh et al., in 20198, simulation
models should play an even more significant role in developing a microsurgery
training curriculum. The model developed in this article was planned for the
technique of cutaneous flap; unfortunately, it does not meet the specificities
and characteristics of a model that allows the practice of free flap.
The model described was presented to a plastic surgeon, a professor of medicine
at the University of Fortaleza. The professor evaluated the simulator and
admitted the possibility of applying this model to teaching the procedure since
the designs and geometries of some flaps are relatively complex to understand.
Moreover, due to its high relevance, being one of the pillars of skin surgery,
it is essential to the academic interested in the specialty, the knowledge of
its execution through training in practical models of low cost and easy
maintenance9, since, for better
learning, the training repeated several times, with a low-cost material, is
something that proves indispensable.
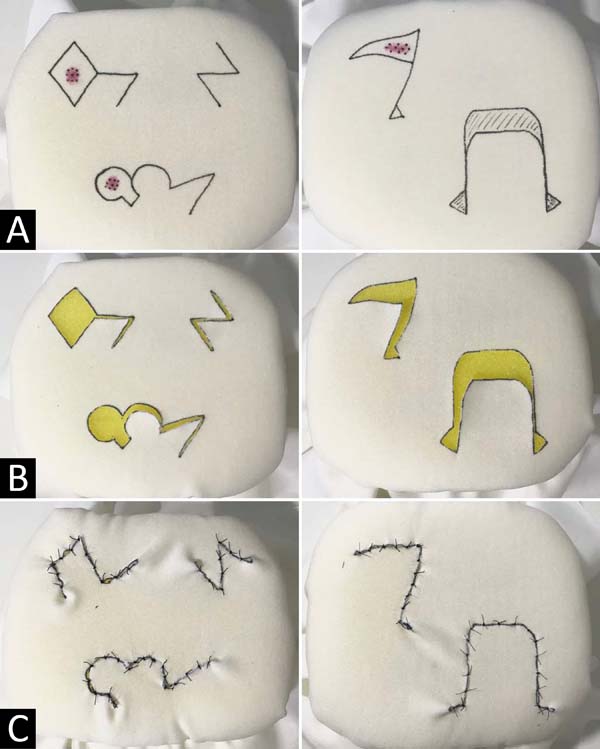
The model also allows the execution of rotation, transposition, interpolation,
and simple advancement flaps, as shown in Figure 4, and can be used to train various types of flaps.
Figure 4 - Demonstration of the flap techniques performed on the model.
A. Markings of the Limberg flaps, Z-plasty,
bilobed, triangular and simple advancement; B.
Incisions and removal of injuries; C. Suture and
completion of flap techniques.
Figure 4 - Demonstration of the flap techniques performed on the model.
A. Markings of the Limberg flaps, Z-plasty,
bilobed, triangular and simple advancement; B.
Incisions and removal of injuries; C. Suture and
completion of flap techniques.
The model proposed by Denadai et al., In 20125, made from chicken skin, proved to be a complementary alternative
to the arsenal of existing simulation models due to its similarity, in texture
and consistency, to human tissue10.
However, when it comes to its continuous use in teaching programs, the animal
model can be expensive, since it needs a collection and storage service so that
it does not bring biological risk to the students of the institutions. Besides,
its preparation is time-consuming and delicate, since it is necessary to defrost
the parts in advance, a process that, when not done well, can leave the material
hardened, causing the loss of needle threads during training and further
increasing it cost.
The use of animal material also presents several ethical and bureaucratic
complications, since besides being questionable, they conflict with modern
concepts of animal welfare. With this, the current diversity and complexity of
surgical medical knowledge require a new direction in teaching through
innovative means, seeking to fulfill the educational function without harming
the animals.
The proposed model, which is based on the use of synthetic fabric overlapping a
layer of sponge for car wash, proved to be entirely objective regarding the
execution of the technique, as the chosen fabric has good resistance to suture,
reducing the probability of dehiscence, doing the practice aimed at improving
the skin flap technique viable and safe. Besides, the model is easy to prepare
and store, as it does not need to be conserved, and its assembly is simple,
practical, and fast.
The proposed model is easy to perform and assembled to facilitate the
understanding of the skin flap technique.
CONCLUSION
It is believed that the use of this synthetic model becomes relevant in the
training of medical students and residents in plastic surgery, because it allows
the practice of this medical skill, with minimal ethical conflicts and without
the need to train in animals or the patient himself.
Besides, the surgical simulation of the cutaneous flap, using the proposed
synthetic model, is a suggestion for the exercise of this technique because it
presents logistical and instructive benefits, such as the use of low-cost
materials, easy storage, and preparation.
However, further studies on the effectiveness of training with synthetic models
for undergraduate medical students are needed, with the elaboration of
questionnaires evaluating students’ perception and instructors’ perception.
REFERENCES
1. Galimberti G, Ferrario D, Casabona GR, Molinari L. Usefulness of
rotation and advancement flap for the closure of skin defects in the malar
region. Surg Cosmet Dermatol. 2013;5(1):769.
2. Townsend Junior CM, Beauchamp RD, Evers B, Mattox K. Sabiston
Tratado de cirurgia: a base biológica da prática cirúrgica moderna. 19ª edição.
Rio de Janeiro: Elsevier; 2015.
3. Anastakis DJ, Regehr G, Reznick RK, Cusimano M, Murnaghan J,
Brown M, et al. Assessment of technical skills transfer from the bench training
model to the human model. Am J Surg. 1999 Fev;177(2):167-70.
4. Purim KSM, Santos LDS, Murara GT, Maluf EMCP, Fernandes JW,
Skinovsky J. Avaliação de treinamento cirúrgico na graduação de medicina. Rev
Col Bras Cir. 2013;40(2):152-6.
5. Denadai R, Saad-Hossne R, Oshiiwa M, Bastos EM. Training on
synthetic ethylene-vinyl acetate bench model allows novice medical students to
acquire suture skills. Acta Cir Bras. 2012 Mar;27(3):271-8.
6. Hammoud MM, Nuthalapaty FS, Goepfert AR, Casey PM, Emmons S,
Espey EL, et al. To the point: medical education review of the role of
simulators in surgical training. Am J Obstetr Gynecol. 2008
Out;199(4):338-43.
7. Khatib M, Soukup B, Boughton O, Amin K, Davis CR, Evans DM.
Plastic surgery undergraduate training. How a single local event can inspire
and
educate medical students. Ann Plast Surg. 2014;1-5.
8. Abi-Rafeh J, Zammit D, Jaberi MM, Al-Halabi B, Thibaudeau S.
Nonbiological microsurgery simulators in plastic surgery training: a systematic
review. Plast Reconstr Surg. 2019 Sep;144(3):496e-507e.
9. Friedlich M, Wood T, Regehr G, Hurst C, Shamji F. Structured
assessment of minor surgical skills (SAMSS) for clinical clerks. Acad Med. 2002
Out;77(10 Supl 1):S39-S41.
10. Denadai R, Saad-Hossne R, Souto L. Simulation-based cutaneous
surgical-skill training on a chicken-skin bench model in a medical undergraduate
program. Indian J Dermatol. 2013 Mai;58(3):200-7.
1. University of Fortaleza UNIFOR, Fortaleza,
CE, Brazil.
Corresponding author: Arthur Antunes Coimbra Pinheiro Pacífico
Rua Mariana Furtado Leite, 1250, Apart. 1201, Bairro Eng, Luciano Cavalcante,
Fortaleza, CE, Brazil. Zip Code: 60811-030 E-mail:
arthurh.pacifico@gmail.com
Article received: August 08, 2019.
Article accepted: July 15, 2020.
Conflicts of interest: none