INTRODUCTION
In 1955, Sir Harold Gillies, father of modern plastic surgery, stated that
photography was among the major advances in the field at the time1. Since then, the importance of
photographic standardization has been the target of numerous publications in
the
international2-5 and Brazilian6-11
literature. However, the teaching and learning of the photodocumentation process
during residency has not been standardized in national peer-reviewed
literature.
OBJECTIVE
The present study aims to outline a formal training program in 2-dimensional
standardized photographic (“photo”) documentation adopted by a residency in
Plastic Surgery.
METHODS
This is a descriptive study about the components of the training program in
photodocumentation adopted by the Brazilian Society of Plastic Surgery (SBCP)
Accredited Service. The structure (active participation in resident training)
and topics covered during training included: design of a photo studio (equipment
types and distribution of equipment), differences among different cameras and
lenses, photographic principles (exposure [aperture, speed and ISO] and depth
of
field), lighting, photo situations in plastic surgery (preoperative,
intraoperative, postoperative, and pediatric documentation), standardized photo
views, photo database management, types of images, computerized photogrammetry,
and ethical and medical-legal issues (including consent for photos).
This study followed the ethical standards of the 1964 Declaration of Helsinki and
its respective amendments and was approved by the local Ethics Committee
(003/2017).
RESULTS
Photographic documentation training program
In 2007, when the institutional photographic protocol was modified, a formal
training program in standard 2-dimensional photodocumentation was
implemented to formalize and stimulate this component of the training
process in Plastic Surgery. The photographic protocol was standardized with
the purpose of maintaining a complete medical image database for
longitudinal documentation (pre- and post-operative periods, early and late)
of all patients (diagnostic process, evolutionary and therapeutic results),
preoperative planning, intraoperative visual reference, ethical and
medical-legal issues, medical education (including training of new plastic
surgeons) and scientific research (presentations and scientific
articles).
As the patient must be the only (or principal) modifiable variable in photos
taken at different times, we have focused our efforts on the careful
standardization of photodocumentation; the goal is to present the patient
accurately (including satisfactory and unsatisfactory results), rather than
producing a favorable view, as is done, for example, in advertising
photography. Thus, all patients have been systematically photographed in the
preoperative, intraoperative, and postoperative periods by a team composed
of a professional photographer contracted by the Institution, plastic
surgeons/preceptors, and residents in Plastic Surgery.
In addition to standard photodocumentation (preoperative and postoperative
[1st and 2nd weeks, 1st, 3rd, 6th, 9th, 12th postoperative months, and then
every 3/6 months]), all additional complications were systematically
photographed. The date was correctly stated (time, day, month, and year) on
each patient’s photograph and records to follow the documentation and
facilitate the active search for specific photos.
Regardless of professional documentation, plastic surgeons/preceptors also
routinely take photos themselves; such a stance serves as an additional
stimulus for training residents. Residents actively participate in all
institutional photo systematization and acquire skills related to
photodocumentation through the training program. Training has been
distributed over the 3 years of the program, with a natural transition of
tasks according to the year of training/acquisition of photo skills:
First-year residents (R1s): the institutional
professional photographer is responsible for the initial teaching-learning
process of the theoretical and practical principles of photography (detailed
below) for residents who have just started training. As the skills are
acquired and properly certified, the R1s begin to photograph outpatients
under the supervision of the “most experienced residents” and
surgeons/preceptors. In all particular situations requiring removal of
clothing or exposure of sexual organs, the professional photographer does
not participate in the photodocumentation, and the R1s are systematically
guided by the more seasoned residents and surgeons/preceptors.
Second-year residents (R2s): participate in the
photodocumentation of patients until the R1s acquire the necessary
skills.
Third-year residents (R3s): perform
photodocumentation in the surgical center (preoperative, intraoperative, and
postoperative).
During and after all photo shoots, the professional photographer,
surgeons/preceptors, and “more experienced” residents are responsible for
reviewing the photos taken by “less experienced” residents in order to
provide constructive feedback and maintain quality of the photos.
Moreover, during this process, all residents are encouraged to practice
knowledge and skills related to photodocumentation (e.g., photographing
outside the hospital setting) in order to expand and refine
photodocumentation as well as strengthen the constructive feedback process
(residents are encouraged to take their questions to the professional
photographer, surgeons/preceptors, and more “experienced” residents).
Components of the training program
During the training process, topics/themes (detailed, from now on) were
presented in theory classes (presentation of concepts) and practicums
(exercises where the concepts were applied). The training resident was
encouraged to learn all nuances of photodocumentation, seeking total control
over the final quality of the photo.
Photo studio2,4,5,12,13
Residents are trained in a white-walled room with curtained windows, equipped
with a rotating chair (360°) for the patient, placed 30-90 cm from a blue
background with carefully marked points to facilitate different photo views;
digital cameras (Nikon® D50), lenses (AF Nikkor® 105 mm), flash units
(Nikon® SB-21/AS-14 and Nikon® SB-26), and digital flash kits (Atek® 160
Plus) were provided. In addition to learning how to use all equipment,
residents gain knowledge about the differences between supplied and
commercially available equipment.
Photo cameras2,4,12,13
All current cameras operate as “dark cameras”: instead of a hole, they have a
lens and diaphragm through which light passes and a light-sensitive
material, i.e., the digital sensor, on the opposite side. The difference
between the cameras lies in the sophistication and efficiency with which
they perform (allowing controlled light to reach the sensor and produce an
image). Some cameras have a direct viewfinder, and reflex cameras (single-
or dual-lens), large format cameras (“studio cameras”), and monitor cameras
(“compact digital cameras”) are also used.
Any shortcomings in the understanding and application of photographic
concepts or the use of automatic controls in the photo process will allow
the system to dictate the results, rather than residents having total
control over their own standardized photos. Thus, digital single-lens reflex
(DSLR) cameras are at the core of training, as they allow greater control
over photo results including lens changes. In these DSLR cameras, the image
shown on the liquid crystal display (LCD) is identical to the image that
will appear on the photo (or computer monitor); the LCD allows immediate
confirmation of the image quality: low-quality images can be retaken. It is
important that residents know the camera’s main components/functions:
shutter, shutter speed control, viewfinder, shutter release, slots for the
lenses, flash, and cables.
Lenses2-5,12,13-15
The lens is the key component of photography because the definition and
sharpness of the image projected are the determining factors of photo
quality. The lenses function as a kind of “funnel” for the light beams,
directing them in a convergent way. Lenses have 2 adjustments: focus
(controlled by a focus ring; the resident must master the use of manual
focus) and diaphragm aperture.
The brightness of an object depends on certain factors: the lens diameter,
lens quality, and quantity, and lens focal length (the distance [in
millimeters]) between the optical center of the lens and the focal plane
when the subject [patient] is in focus). The sensor will receive more light
with a lens of larger diameter and will receive less light with greater
focal length and number of lenses.
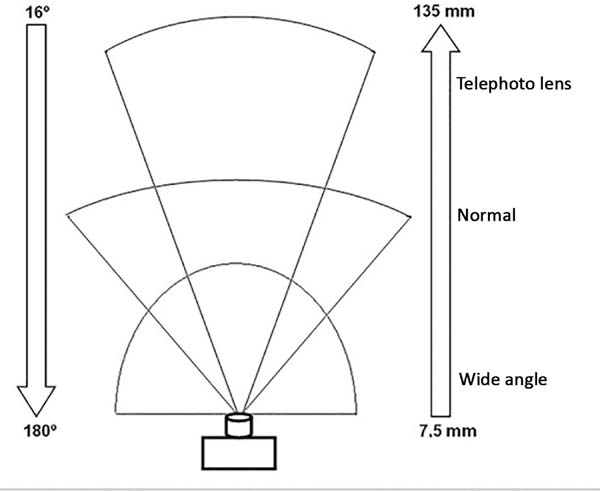
Different types of lenses are defined according to focal length: normal,
wide-angle, and telephoto (Figure 1).
Like human eyes, normal lenses cover a 45°-50° angle of the scene (for
example, the 50 mm lens covers approximately 46° of the scene). Wide-angle
lenses have a smaller focal length and a larger coverage angle compared to
normal lenses; with these wide-angle lenses, patients closer or farther seem
respectively larger or smaller than in reality.
Figure 1 - Simplified schematic representation of the relationship
between (Left) viewing angle (°) and (Right) focal length (space
between the sensor and optical center of the lens focused to
infinity) of wide angle, normal, and telephoto lenses shown in
millimeters (mm). As the lens size increases, the focal length
increases and the range angle decreases. Fixed lenses have a
single focal length (e.g., 105 mm), while zoom lenses show focal
length variation (e.g., 18-55 mm). Because the normal focal
length of the human eye is approximately 50 mm, normal 50-mm
lenses provide a natural, undistorted image. Focal distances of
less than 50 mm can produce images with radial distortion and
therefore are not recommended for photographing faces. Note: The
proportions of distances and sizes in the sketch are not
true-to-life.
Figure 1 - Simplified schematic representation of the relationship
between (Left) viewing angle (°) and (Right) focal length (space
between the sensor and optical center of the lens focused to
infinity) of wide angle, normal, and telephoto lenses shown in
millimeters (mm). As the lens size increases, the focal length
increases and the range angle decreases. Fixed lenses have a
single focal length (e.g., 105 mm), while zoom lenses show focal
length variation (e.g., 18-55 mm). Because the normal focal
length of the human eye is approximately 50 mm, normal 50-mm
lenses provide a natural, undistorted image. Focal distances of
less than 50 mm can produce images with radial distortion and
therefore are not recommended for photographing faces. Note: The
proportions of distances and sizes in the sketch are not
true-to-life.
Telephoto lenses have a greater focal length and lower coverage angle when
compared to normal lenses; hence, distant patients seem to be close to the
camera. Zoom lenses have variable focal length. Residents should primarily
master optical zoom, not digital zoom. However, the use of zoom lenses is
not recommended for preoperative and postoperative documentation, as
potential variation may compromise photo standardization.
Fixed lenses have been the most used, and must be chosen according to the
need, to allow better photo standardization. For example, focal length
lenses between 90 and 105 mm are recommended to capture pertinent facial
anatomy as they provide greater depth of field, ensuring that the entire
face is in focus. On the other hand, macro lenses are convenient for
intraoperative photographs and documentation of skin lesions or scars as
they enlarge the subject that is close to the camera.
Photographic principles2,4,12,14
Exposure: the relationships between the
aperture (“amount of light”), shutter speed (“how much light will reach the
digital sensor”), and ISO (sensitivity) are considered the “photo exposure
triangle.” In contrast with automatic exposure, the 3 functions must be
controlled/modified according to each particular situation via a
selector/button on the camera body or on the lens itself (speed).
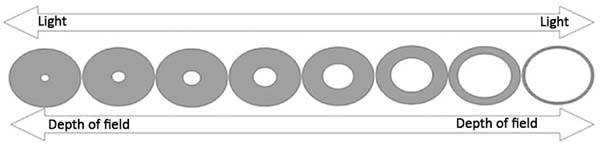
Aperture is defined by the diaphragm
(“opening”) that controls the amount of light entering the lens. The
diaphragm has several aperture values, symbolized by “f.” Increasing the “f”
value reduces the orifice size (Figure 1). The aperture also affects the depth of field.
Speed indicates the time the shutter (located
between the lens and the sensor, to control the time [speed with] light can
enter the camera) is open, when the sensor will receive light. Speed values
are defined in fractions (for example, 125 means that the sensor is exposed
to light for 1/125 s). The smaller the number, the lower the speed at which
the light will reach the sensor; speeds below 60-30 may require use of a
tripod to prevent loss of photo quality (Figure 2).
Figure 2 - Simplified diagrammatic representation of the diaphragm (set
of superimposed blades— “leaf shutter”—inside the lens that
allows control of the amount of light entering the camera). The
diaphragm aperture values are indicated by “f” (in the diagram,
from left to right: f/16, f/11, f/8, f/5.6, f/4, f/2.8 and
f/1.4). The larger the number, the more closed the diaphragm,
and therefore less light will pass through the hole. The
aperture of the diaphragm also controls the depth of field
(extension of the sharp region [in focus] when taking a
picture); the greater the aperture of the diaphragm (i.e., the
smaller the number), the smaller the depth of field. In medical
photos, maximum clarity of the subject/patient is sought so that
details are not lost; this is achieved by adopting small
diaphragm apertures, preferably > f8. Note: The proportions
of distances and sizes in the sketch are not
true-to-life.
Figure 2 - Simplified diagrammatic representation of the diaphragm (set
of superimposed blades— “leaf shutter”—inside the lens that
allows control of the amount of light entering the camera). The
diaphragm aperture values are indicated by “f” (in the diagram,
from left to right: f/16, f/11, f/8, f/5.6, f/4, f/2.8 and
f/1.4). The larger the number, the more closed the diaphragm,
and therefore less light will pass through the hole. The
aperture of the diaphragm also controls the depth of field
(extension of the sharp region [in focus] when taking a
picture); the greater the aperture of the diaphragm (i.e., the
smaller the number), the smaller the depth of field. In medical
photos, maximum clarity of the subject/patient is sought so that
details are not lost; this is achieved by adopting small
diaphragm apertures, preferably > f8. Note: The proportions
of distances and sizes in the sketch are not
true-to-life.
ISO is the measure of sensitivity of the sensor
to light. The higher the ISO number, the greater the sensitivity of the
sensor and the greater the light pickup; however, the image may be affected
by “noise,” with reduced photo quality.
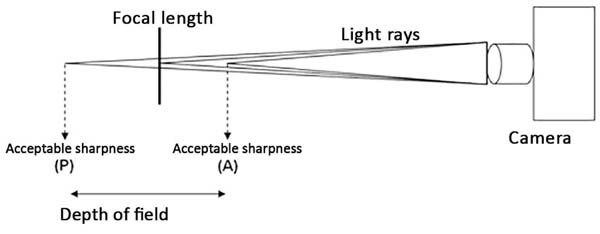
Depth of field is defined by the area before
(anterior, front) and after (posterior, back) the patient/subject, in which
the sharpness is acceptable (Figure 3). This is dependent on the aperture (Figure 2), and focal length of the lenses (telephoto lenses
[e.g., 300 mm] have smaller field depths than normal lenses [e.g., 50 mm]
with the same aperture).
Figure 3 - Simplified schematic representation of the depth of field. A
specific anatomical structure (e.g., eyes, ear, or lips) should
be standardized as a focal point for each photo view (or pose).
Thus, the depth of field is defined by the anterior (A) and
posterior (P) areas of the focal plane in which sharpness is
acceptable.
Figure 3 - Simplified schematic representation of the depth of field. A
specific anatomical structure (e.g., eyes, ear, or lips) should
be standardized as a focal point for each photo view (or pose).
Thus, the depth of field is defined by the anterior (A) and
posterior (P) areas of the focal plane in which sharpness is
acceptable.
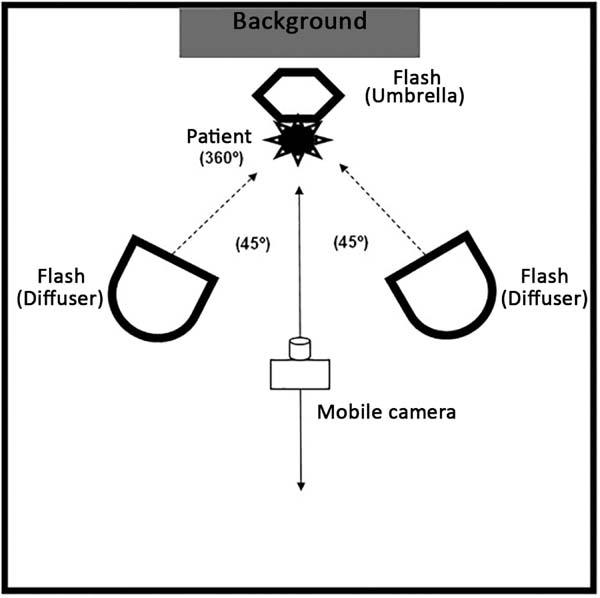
Lighting2-5,12,14,15
Mastering natural and artificial lighting is essential to take good quality
photos. In a studio, lighting can be fully controlled (Figure 4). The flash is routinely used due to its
power. The shutter (speed) must be synchronized with the flash, and only the
aperture may be modified. Flashes are used with diffusers and reflectors
(soft fabrics) to soften the shadows (balance the illumination). A circular
flash used with a macro lens should be applied, especially when recording
small subjects (e.g., scars and skin lesions) and cavities (e.g., oral
cavity and tissue tunnels formed by dissection) to eliminate shadows and
improve the photo result.
Figure 4 - Artificial lighting: Three flashes are carefully arranged to
reflect and diffuse light: 2 floodlights attached to diffusers
are positioned at 1-1.5 m from the patient at a 45° angle of the
patient camera axis and a floodlight attached to a reflector
(umbrella) is positioned above and posteriorly to the patient,
with incidence of light facing the ceiling. The flashes should
be synchronized with the camera shutter. A 30-60-cm distance
should be maintained between the patient and the blue background
(blue provides sufficient contrast, is complementary to all skin
colors, allows greater depth of field, and moderates shadows
without overcasting the patient) to avoid shadows. Since the
quality and quantity of lighting are constant, configurations
with large openings (f>16) and low speeds (<1/125) can be
easily achieved. Note 1: Professional support is recommended for
initial setup. Note 2: distances/sizes are not
true-to-life.
Figure 4 - Artificial lighting: Three flashes are carefully arranged to
reflect and diffuse light: 2 floodlights attached to diffusers
are positioned at 1-1.5 m from the patient at a 45° angle of the
patient camera axis and a floodlight attached to a reflector
(umbrella) is positioned above and posteriorly to the patient,
with incidence of light facing the ceiling. The flashes should
be synchronized with the camera shutter. A 30-60-cm distance
should be maintained between the patient and the blue background
(blue provides sufficient contrast, is complementary to all skin
colors, allows greater depth of field, and moderates shadows
without overcasting the patient) to avoid shadows. Since the
quality and quantity of lighting are constant, configurations
with large openings (f>16) and low speeds (<1/125) can be
easily achieved. Note 1: Professional support is recommended for
initial setup. Note 2: distances/sizes are not
true-to-life.
Preparation of patients3,5,14,15
All objects that may cause visual distraction should be systematically
removed from the visual field prior to photodocumentation. The frontal
region and ears should not be covered by hair. Glasses, jewelry, hearing
aids, and makeup should be removed. All clothing that interferes with the
visibility of target areas should be removed. As many patients may feel
uncomfortable without clothing, and underwear can produce inconsistent
photographs, disposable photo clothing can be used; it is important to
maintain consistency of use when different photos are taken, for example, in
the preoperative and postoperative periods.
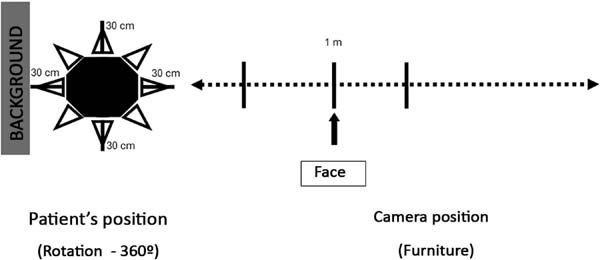
Positioning of patients and the camera2-5,12,14-16
Proper positioning of the patient and the camera should be standardized
according to the target anatomical region, to allow reproducibility with
steady quality. For example, in the sitting position, the patient should be
erect on a swivel seat, and the head should be flexed or extended up to the
desired plane (e.g., Frankfurt horizontal plane, interpupillary plane, or
vertical midline). Pre-placed markings on the walls and floor can guide
proper positioning and assist precise rotation of the patient.
The axis formed between the camera lens and a specific anatomical point, and
the distance between the camera and the patient, should also be
standardized, and may vary according to the location in the photo. The lens
axis should be at the same height as the center of the area to be
photographed (Figure 5).
Figure 5 - Simplified schematic representation of patient and camera
positions (photographer). The patient should be positioned in
the center of an octagon with a radius of 30-60 cm, allowing
360° rotation. To determine the ideal focal length for specific
anatomical regions, experimental shots should be taken at
different distances. Once the desired photo results have been
achieved, the position should be marked on the floor and photos
of the same anatomical region should always be based on that
mark. In the sketch, in our studio, the distance of 1 m between
the patient and camera was standardized to document the complete
face (constant illumination, 105 mm lens, ISO 100, speed 1/125,
variable aperture). Note 1: The marks on the floor must be made
according to the conditions of each studio to maintain photo
quality. Note 2: The proportions of the distances and sizes in
the sketch are not true-to-life.
Figure 5 - Simplified schematic representation of patient and camera
positions (photographer). The patient should be positioned in
the center of an octagon with a radius of 30-60 cm, allowing
360° rotation. To determine the ideal focal length for specific
anatomical regions, experimental shots should be taken at
different distances. Once the desired photo results have been
achieved, the position should be marked on the floor and photos
of the same anatomical region should always be based on that
mark. In the sketch, in our studio, the distance of 1 m between
the patient and camera was standardized to document the complete
face (constant illumination, 105 mm lens, ISO 100, speed 1/125,
variable aperture). Note 1: The marks on the floor must be made
according to the conditions of each studio to maintain photo
quality. Note 2: The proportions of the distances and sizes in
the sketch are not true-to-life.
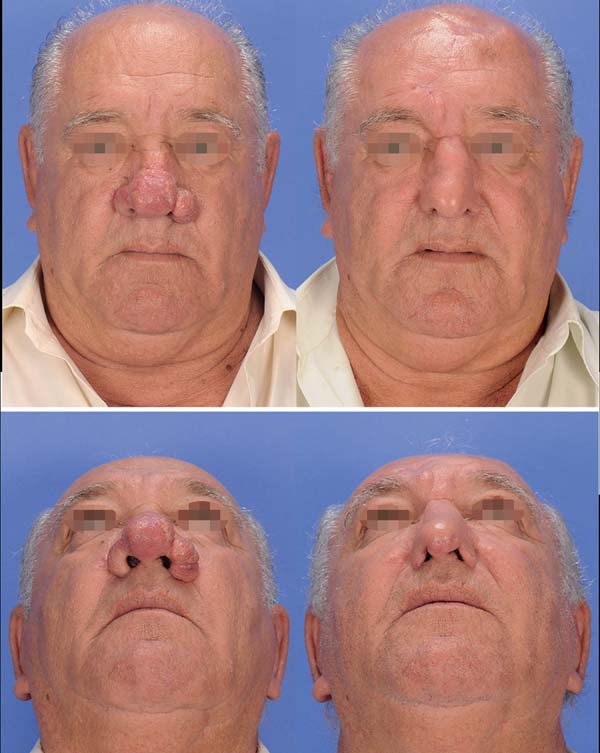
Photoshoot conditions 2-4,16-18
Preoperative and postoperative: In pre- and
postoperative photography, the results are only comparable when the
standardization (detailed, as noted above) is consistently reproduced. The
same equipment with the same settings should be used in pre- and
postoperative photos (Figures 6-8). With standardization, there may be
differences in inter-individual comparisons (mainly children versus adults),
but the intra-individual comparison is entirely feasible.
Figure 6 - Preoperative (Left) and postoperative (Right) standard
2-dimensional photos (Nikon® D50, constant illumination, 105 mm
lens, ISO 100, speed 1/125, aperture 14) of a patient with
rhinophyma subjected to nasal reconstruction with a forehead
flap. Frontal and basal views (Above and Below,
respectively).
Figure 6 - Preoperative (Left) and postoperative (Right) standard
2-dimensional photos (Nikon® D50, constant illumination, 105 mm
lens, ISO 100, speed 1/125, aperture 14) of a patient with
rhinophyma subjected to nasal reconstruction with a forehead
flap. Frontal and basal views (Above and Below,
respectively).
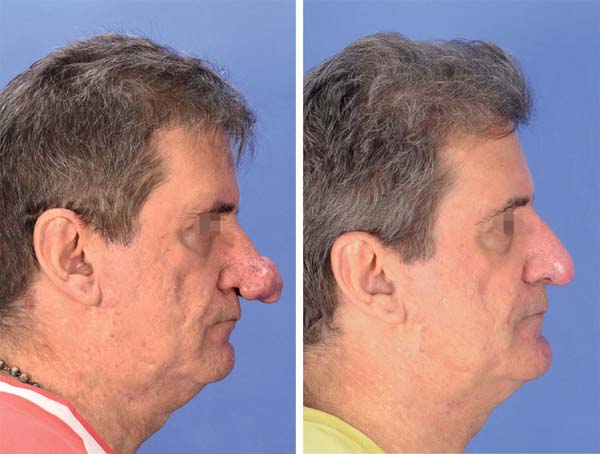
Figure 7 - Standard 2-dimensional photos (Canon® 70D; constant
illumination; objective 50 mm; ISO 100; speed 1/125; aperture
13) of a patient with rhinophyma subjected to tangential
excision with electrocoagulation. Frontal views in the
preoperative (Left) and postoperative period (Right).
Figure 7 - Standard 2-dimensional photos (Canon® 70D; constant
illumination; objective 50 mm; ISO 100; speed 1/125; aperture
13) of a patient with rhinophyma subjected to tangential
excision with electrocoagulation. Frontal views in the
preoperative (Left) and postoperative period (Right).
Figure 8 - Standard 2-dimensional photos of the same patient (
Figure 7). Side views in the
preoperative (Left) and postoperative period (Right).
Figure 8 - Standard 2-dimensional photos of the same patient (
Figure 7). Side views in the
preoperative (Left) and postoperative period (Right).
Intraoperative: It is important that any
unnecessary objects (hands, surgical instruments, compresses, saliva, blood,
etc.) are completely removed from the area being photographed. A blue (or
green) background should be used wherever possible. DSLR cameras with macro,
fixed lens, and circular flash are the most recommended for such
documentation. The surgical light source must be turned off to avoid shadows
that may affect color balance.
Pediatric patients: patients who do not yet sit
or stand should preferably be photographed in their parents’ arms, being
careful to wrap parents’ bodies with blue clothing while using a full blue
background. It may be necessary to hold the child’s attention using noises
or movements, to keep the head in designated position.
Movements (muscular action): Functional
deficits and improvements may be documented; images during movement (for
example, facial expression) are extremely useful in evaluating details of
muscular action. For this purpose, numerous photos must be taken from the
same point of view.
Photo views2-5,8,15-17,19-21
A set of standard photographic views (or poses) (frontal [or
anteroposterior], bilateral profile [or lateral], and bilateral semi-
profile [or oblique; 45°]) is used in most documentation, and supplementary
views (including close-ups) should be photographed according to each
specific anatomical region, type of deformity, and surgical intervention
(Table 1). Anatomical points and
limits must be carefully employed to maintain the standardization of photo
views.
Table 1 - General composition of the photo views for anatomical regions,
surgical procedures, and specific deformities
2-5,8,14-17,19-21.
| Anatomical Regions/Surgical Procedures/Specific
Deformities
|
Photographic views |
| Face (full) |
Standard |
| Face (close up)* |
Standard + B |
| Rhytidectomy |
Standard + facial expression |
| Ears |
Standard + PA + P(PA) + SM(PA) |
| Eyelids |
Standard + periorbital expression |
| Mento/cervical ** |
Standard + extension and cervical
flexion
|
| Breasts *** |
Standard |
| Abdomen **** |
Standard |
| Hands/fingers |
Palmar, dorsal, and lateral views |
| Cleft lip and palate |
Standard, AP' + B + intraoral |
| Maxillomandibular/occlusal deformities |
Standard + AP' + P' + intraoral |
| Cranial deformities |
Standard + SC |
Table 1 - General composition of the photo views for anatomical regions,
surgical procedures, and specific deformities
2-5,8,14-17,19-21.
Photo database 4,13,16,19,22-24
Given the nature of patient photos, we should be extremely cautious in the
handling, storage, and use of all medical photodocumentation. It is
important that the entire process involved in photo storage, file renaming
(including the creation of a database that facilitates subsequent searches),
and backup (files regularly recorded to a CD, DVD, or external hard drive)
be executed judiciously and efficiently.
To do this, all photos stored on a digital camera memory card are transferred
to a computer hard disk. The files must then be renamed, ensuring that each
file has a unique name to avoid overwriting; file names should not exceed 31
characters in length to allow compatibility with different operating systems
(PC, Mac, and Unix). The ultimate goal of renaming should be ease and
reliability of access (search and retrieval) of target images. Existing
keywords and practical renaming systems can be applied according to the
need: for example, date (year/month/day) of the photo, medical record
number, follow-up period (e.g., preop, postop 3 months, or postop 1 year),
and file extension (e.g., jpg) - “2018.02.01_00123_preop.jpg” or “2018.02.01
(00123)(preop).jpg”.
Image formats4,13,16,17,19,22-25
Images can be transferred to the computer hard drive in a variety of file
formats, with 2 types of recording systems: lossless and lossy (larger and
smaller file sizes, respectively). In lossless formats such as TIF
(tagged-image format), BMP (bitmap), PSD (Photoshop), and Macintosh PIC, the
images are saved in their entirety, preserving all original information. On
the other hand, in lossy formats (JPEG, Joint Photographic Experts Group),
images are compressed into smaller files, eliminating some of the original
image information each time the file is modified and saved, thus, degrading
their quality.
The JPEG format is commonly used because it can be easily imported into word
processing, presentation, and image manipulation programs. The TIF format
has been the most commonly used in scientific publishing. Converting JPEG to
TIFF in an image editor increases the size of the file but does not improve
the image quality. Another available file format is RAW (known as “digital
negative”). Unlike others, the actual information in the photo is completely
transferred to the hard drive in RAW format. The RAW format contains
detailed information (e.g., white balance, contrast mapping, and so on) and
thus has the potential to produce better image quality due to minimal data
manipulation.
As most current DSLR cameras offer the option of recording images as JPEG
files, RAW files, or both, issues such as storage space (hard disk size) and
willingness to process images should be considered when choosing
formats.
Computerized photogrammetry6,7,14
Residents also learn about standardized, 2-dimensional computerized digital
photogrammetry, a form of indirect anthropometry. In this part of training,
measurements (linear, angular, and area) are performed on 2-dimensional
digital photos using specific software (e.g., ImageJ, Adobe Photoshop,
Mimics, among others). Thus, it is possible to objectively compare linear
measurements between well-established anatomical points in the preoperative
and postoperative periods. Acquiring this particular skill increases the
scientific arsenal for residents who can then participate in scientific
research projects that objectively evaluate surgical outcomes.
Ethical and medical-legal issues2,4,14-16,22,26,27
Medical photodocumentation is completely entangled in multidimensional
ethical and medical-legal dilemmas. While standardized photodocumentation
may assist the surgeon in possible medical-legal implications—if there is
litigation involving a particular surgical treatment, the images may be
applied as evidence—any “improper” use (including loss) of patient photos
may end up having ethical and medical-legal implications. Therefore, all
those involved with medical photodocumentation must meticulously ensure that
patients are fully respected in order to maintain the essence of ethical and
medical-legal principles in which the physician-patient relationship can be
longitudinally structured.
Thus, prior to any photodocumentation, all patients or legal guardians (in
case of being incapable) must systematically provide written photographic
consent. Consent should be specifically provided for identifiable and
non-identifiable photos, making clear all potential uses, including clinical
information as part of the medical record, educational purposes, lectures,
exhibitions, and scientific publications (books and articles). In addition
to this basic information, it is critical that patients and family members
understand other key elements: consent can be withdrawn at any time, and
more importantly, once the photos are published (in periodicals, books,
etc.), they enter the public domain and may be impossible to remove.
Since photos are part of the patient medical record, maximum safety must be
guaranteed; the database must be password-protected and have limited access
in order to prevent unauthorized use. Moreover, patients should be
photographed only according to an institutional protocol, and photographing
patients and archiving photos on personal cameras or cell phones should be
avoided—there is even evidence in literature26 about patients preferring photos taken with hospital cameras.
Although personal cell phones are readily available, their application in
the medical environment has not yet been fully defined and there are
examples in the literature of problems with the “simple” use of a cell phone
camera.
Finally, residents should be trained in the informed consent process and
recognition of patient/family concerns. Residents must master the laws that
regulate medical practice (Code of Medical Ethics) and plastic surgery in
Brazil. For example, patient photos cannot be applied to self-promotion or
medical advertising, even with authorization (Medical Advertising Manual -
CFM Resolution 1974/11).
DISCUSSION
Clinical-surgical experiences should be considered as critical factors in
determining the success of resident education in Plastic Surgery28. Furthermore, mastering good quality
standardized photodocumentation stands out among the many skills and tools that
every plastic surgeon must acquire during training10.
The continuous growth and refinement of digital imagery undoubtedly enable an
increase in use of medical photos in the academic environment, including pre-
and postoperative evaluation, which has become the standard for the
classification of results in plastic surgery29. However, we and other authors4,5,14,19,29,30 continue to
see many photos in scientific publications and presentations that do not meet
the criteria for pre- and postoperative quality or consistency.
These non-standardized photos can misrepresent the patient’s primary complaint,
distort perceptions of surgical outcomes, and divert attention from those
viewing the image2,9,29,30.
In the literature, Dr. Paul Tessier, the father of modern craniofacial surgery,
took care to longitudinally photograph his patients, and is recognized, to this
day for his incredible surgical results. The importance of documentation in
plastic surgery is also reinforced among the principles (“Keep an Accurate
Record”) described by Dr. Ralph Millard, a renowned plastic surgeon. We believe
that acquisition of this skill by residents should be promoted by all those
involved in the training process. Thus, we outlined a formal training program
in
standard 2-dimensional photodocumentation. The present study serves as a guide
for the development of photo skills during training in Plastic Surgery, which
preceptors and residents can apply to expand their understanding of detailed
photo concepts.
The present training program was structured to develop photo skills during
training in Plastic Surgery and therefore does not exhaust the subject.
Additional photographic aspects should be reviewed in specific articles2-10,12-17,20,22.
CONCLUSION
Formal training in standardized 2-dimensional photodocumentation complements the
arsenal of skills required for residents in Plastic Surgery, in order to better
prepare them for future careers.
COLLABORATIONS
|
RF
|
Final approval of the manuscript, conceptualization, design and draft
of the study, methodology, performance of operations and/ or
experiments, writing - preparation of the original, writing - review
and editing.
|
|
AS
|
Final approval of the manuscript, data collection.
|
|
EG
|
Final approval of the manuscript, data collection, writing - review
and editing.
|
|
CLB
|
Final approval of the manuscript, data collection, writing - review
and editing.
|
|
CARA
|
Final approval of the manuscript, data collection, writing - review
and editing.
|
|
CERA
|
Final approval of the manuscript, conceptualization, design and draft
of the study, methodology, performance of operations and/ or
experiments, writing - review and editing.
|
REFERENCES
1. Guy C, Guy RJ, Zook EG. Standards of photography (Discussion). Plast
Reconstr Surg. 1984;74(1):145-6.
2. Archibald DJ, Carlson ML, Friedman O. Pitfalls of nonstandardized
photography. Facial Plast Surg Clin North Am.
2010;18(2):253-66.
3. Persichetti P, Simone P, Langella M, Marangi GF, Carusi C. Digital
photography in plastic surgery: how to achieve reasonable standardization
outside a photographic studio. Aesthetic Plast Surg.
2007;31(2):194-200.
4. Ettorre G, Weber M, Schaaf H, Lowry JC, Mommaerts MY, Howaldt HP.
Standards for digital photography in cranio-maxillo-facial surgery - Part I:
Basic views and guidelines. J Craniomaxillofac Surg.
2006;34(2):65-73.
5. Yavuzer R, Smirnes S, Jackson IT. Guidelines for standard
photography in plastic surgery. Ann Plast Surg.
2001;46(3):293-300.
6. Quieregatto PR, Hochman B, Furtado F, Machado AF, Sabino Neto M,
Ferreira LM. Image analysis software versus direct anthropometry for breast
measurements. Acta Cir Bras. 2014;29(10):688-95.
7. Hochman B, Castilho HT, Ferreira LM. Padronização fotográfica e
morfométrica na fotogrametria computadorizada do nariz. Acta Cir Bras.
2002;17(4):258-66.
8. Hochman B, Nahas FX, Ferreira LM. Photography in medical research.
Acta Cir Bras. 2005;20(Suppl 2):19-25.
9. Paccanaro RC, Gragnani A, Calil JA, Secco LG, Miranda RE, Bersou G,
et al. Padronização e avaliação fotográfica em cirurgia periorbital. Rev Bras
Cir Plást. 2010;25(2):278-84.
10. Scomação IR, Graf RM, Maluf I Jr, Forte AJ, da Silva Freitas R.
Evaluation of Photographic Variables in Patients with Indication for Facial
Rejuvenation. Aesthetic Plast Surg. 2013;37(6):1114-9.
11. Raposo-Amaral CE, Raposo-Amaral CA. Changing face of cleft care:
specialized centers in developing countries. J Craniofac Surg.
2012;23(1):206-9.
12. Soto-Medina CA, Guerrerosantos J, de la Torre-Guerrerosantos Y.
Fotografía digital: una guía sencilla de actualización. Cir Plást Iberolatinoam.
2014;40(1):29-37.
13. Peck JJ, Roofe SB, Kawasaki DK. Camera and lens selection for the
facial plastic surgeon. Facial Plast Surg Clin North Am.
2010;18(2):223-30.
14. Quieregatto PR, Hochman B, Furtado F, Ferrara SF, Machado AF, Sabino
Neto M, et al. Photographs for anthropometric measurements of the breast region.
Are there limitations? Acta Cir Bras. 2015;30(7):509-16.
15. Swamy RS, Most SP. Pre- and postoperative portrait photography:
standardized photos for various procedures. Facial Plast Surg Clin North Am.
2010;18(2):245-52.
16. Schaaf H, Streckbein P, Ettorre G, Lowry JC, Mommaerts MY, Howaldt
HP. Standards for digital photography in cranio-maxillo-facial surgery--Part
II:
Additional picture sets and avoiding common mistakes. J Craniomaxillofac Surg.
2006;34(7):444-55.
17. Santo PRQE, Sabino Neto M, Furtado F, Trigo Junior TW, Santo AAQE,
Nonato FL, et al. Conhecendo os tipos de arquivo de fotografia JPEG e RAW
utilizados em pesquisa. Rev Bras Cir Plást. 2018;33(1):89-95.
18. Humphrey CD, Kriet JD. Intraoperative photography. Facial Plast Surg
Clin North Am. 2010;18(2):329-34.
19. Solesio Pilarte F, Lorda Barraguer E, Lorda Barraguer A, Laredo
Ortiz C, Rubio Verdú R. Estandarización fotográfica en Cirugía Plástica y
Estética. Cir Plást Iberolatinoam. 2009;35(2):79-90.
20. Henderson JL, Larrabee WF Jr, Krieger BD. Photographic standards for
facial plastic surgery. Arch Facial Plast Surg.
2005;7(5):331-3.
21. Gherardini G, Matarasso A, Serure AS, Toledo LS, DiBernardo BE.
Standardization in photography for body contour surgery and suction-assisted
lipectomy. Plast Reconstr Surg. 1997;100(1):227-37.
22. Segal J, Sacopulos MJ. Photography consent and related legal issues.
Facial Plast Surg Clin North Am. 2010;18(2):237-44.
23. Humphrey CD, Tollefson TT, Kriet JD. Digital asset management.
Facial Plast Surg Clin North Am. 2010;18(2):335-40.
24. Hamilton GS 3rd. Photoshop tips and tricks every facial plastic
surgeon should know. Facial Plast Surg Clin North Am.
2010;18(2):283-328.
25. Pham AM, Tollefson TT. Objective facial photograph analysis using
imaging software. Facial Plast Surg Clin North Am.
2010;18(2):341-9.
26. Lau CK, Schumacher HH, Irwin MS. Patients' perception of medical
photography. J Plast Reconstr Aesthet Surg. 2010;63(6):e507-11.
27. Carreiro PR. Ethics in the digital age. Rev Col Bras Cir.
2014;41(4):234-5.
28. Denadai R, Muraro CAS, Raposo-do-Amaral CE. Cirurgiões plásticos
como cirurgiões de mão: a visão dos residentes. Rev Bras Cir Plást.
2014;29(3):422-31.
29. Parker WL, Czerwinski M, Sinno H, Loizides P, Lee C. Objective
interpretation of surgical outcomes: is there a need for standardizing digital
images in the plastic surgery literature? Plast Reconstr Surg.
2007;120(5):1419-23.
30. Riml S, Piontke AT, Larcher L, Kompatscher P. Widespread disregard
of photographic documentation standards in plastic surgery: a brief survey.
Plast Reconstr Surg. 2010;126(5):274e-6e.
1. Hospital SOBRAPAR, Instituto de Cirurgia
Plástica Craniofacial, Campinas, SP, Brazil.
2. Faculdade de Ciências Médicas, Universidade
Estadual de Campinas, Campinas, SP, Brazil.
Corresponding author: Rafael Denadai, Av. Adolpho Lutz, 100 -
Cidade Universitária - Campinas, SP, Brazil, Zip Code 13083-880. E-mail:
denadai.rafael@hotmail.com
Article received: May 23, 2018.
Article accepted: October 4, 2018.
Conflicts of interest: none.