INTRODUCTION
Burns during pregnancy require greater care due to associated physiological
changes. The incidence of burns during pregnancy is not well established in the
literature, but is estimated to range between 3% and 7%, and primarily reflects
the incidence in developing countries1,2. The management
of burns in pregnancy represents a great challenge, with significant impact on
maternal-fetal prognosis. We report two cases treated in the burn unit of the
Paulista School of Medicine, Federal University of São Paulo (EPM/UNIFESP), in
São Paulo, SP.
CASE REPORTS
Clinical case 1
A 36-year-old, previously healthy woman sustained accidental burns caused by
a flaming alcoholic liquid. She was injured in the 10th week of gestation,
with body surface area involvement of 29%. She had 2nd and 3rd degree burns
on the face, chest, abdomen, arms, hands, and legs bilaterally. She
underwent tracheal intubation on admission for respiratory insufficiency
secondary to likely inhalation injury, which was later confirmed with
bronchoscopy.
During hospitalization, she underwent debridement and grafting of burned
areas with success. The obstetrics team was involved in her care and
ultrasound confirmed the gestational age. The patient was discharged from
the hospital after completion of burn treatment and was referred for
outpatient obstetric follow-up until full-term birth (Figures 1, 2,
3, and 4).
Figure 1 - Case 1 - Appearance of burns on admission. Most are
2nd degree, but areas of 3rd degree
burns are present on the breasts and right arm.
Figure 1 - Case 1 - Appearance of burns on admission. Most are
2nd degree, but areas of 3rd degree
burns are present on the breasts and right arm.
Figure 2 - Case 1 - 2nd degree burns in the lower limbs on
admission.
Figure 2 - Case 1 - 2nd degree burns in the lower limbs on
admission.
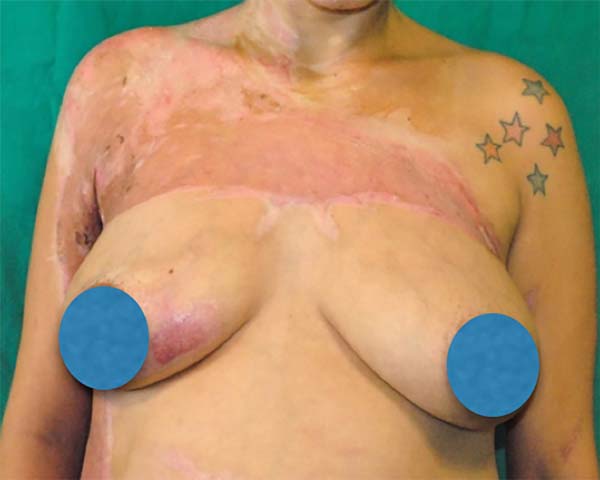
Figure 3 - Late postoperative Case 1 - Areas of partial skin grafting on
the breasts, axillae, and right arm.
Figure 3 - Late postoperative Case 1 - Areas of partial skin grafting on
the breasts, axillae, and right arm.
Figure 4 - Late postoperative Case 1 - Patient with healing
2nd degree burns and partial skin graft donor
area on the left side of the healed left thigh.
Figure 4 - Late postoperative Case 1 - Patient with healing
2nd degree burns and partial skin graft donor
area on the left side of the healed left thigh.
Clinical case 2
A 29-year-old woman was the victim of aggression by her partner at 31 weeks
of gestation, with burns caused by a flaming alcoholic liquid. She had 2nd
and 3rd degree burns on 15% of the body surface, involving the face, neck,
anterior trunk, and right upper limb.
During hospitalization, she underwent debridement and grafting of burned
areas with success. Cardiotocography was performed by the obstetrics team to
monitor fetal viability. She was discharged from the burn unit and
transferred to the obstetrics unit, where she remained hospitalized until
full-term birth (Figures 5, 6, 7, and 8).
Figure 5 - Case 2 - Appearance of 3rd degree burns on the
chest on admission.
Figure 5 - Case 2 - Appearance of 3rd degree burns on the
chest on admission.
Figure 6 - Case 2 - 2nd degree burns on the right hand, with
deep area in the thenar region.
Figure 6 - Case 2 - 2nd degree burns on the right hand, with
deep area in the thenar region.
Figure 7 - Late postoperative Case 2 - Postoperative appearance of
partial skin graft on the chest.
Figure 7 - Late postoperative Case 2 - Postoperative appearance of
partial skin graft on the chest.
Figure 8 - Late postoperative Case 2 - Right hand after partial skin
grafting in the thenar region in order to preserve grip
function.
Figure 8 - Late postoperative Case 2 - Right hand after partial skin
grafting in the thenar region in order to preserve grip
function.
DISCUSSION
The percentage of body surface area (BSA) involvement is the main prognostic
factor for maternal and fetal mortality, with 50% mortality when involved BSA is
>40%1. Inhalation injury is another
important prognostic factor related to maternal and fetal mortality3-5. The most common complication is fetal distress, followed by
spontaneous abortion and preterm labor3,4.
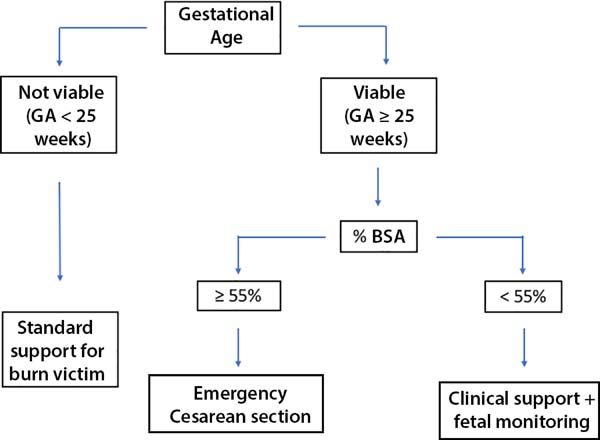
Proper treatment is essential for success and survival of the fetus. On initial
assessment, the maternal BSA and gestational age (GA) of the fetus should be
calculated, preferably by ultrasound, to confirm fetal viability. In 2015,
Parikh et al.1 published
an algorithm designed to assist in the management of pregnant burn victims
(Figure 9).
Figure 9 - Algorithm for the treatment of burns in pregnancy. Adapted from
Parikh et al.
1.
Figure 9 - Algorithm for the treatment of burns in pregnancy. Adapted from
Parikh et al.
1.
Pregnant patients with more than 55% BSA involvement should undergo urgent
cesarean section if the fetus is viable, as this significantly improves maternal
and fetal prognosis. In cases with less than 55% BSA involvement, resuscitation
and support measures should continue, with continuous fetal monitoring and use
of corticosteroids to induce fetal lung maturation if needed1.
Hypovolemia is a major challenge in the treatment of burns in general. There is
no guideline for fluid resuscitation in pregnant burn patients, but in general,
the Parkland formula is used; the formula recommends an increase in fluid
replacement by 30%, due to the physiological increase in intravascular volume
during gestation1,2. In pregnancy, hypovolemia may have direct
implications for the progress of gestation6. Fluid loss after a burn can trigger premature labor2.
Another source of vulnerability in pregnant burn victims is the upper airway1,6. Physiological edema that is already present in the upper airways
during pregnancy can accelerate airway obstruction in cases of inhalation injury
and can interfere with intubation1,5.
The first clinical case describes treatment in the first trimester of pregnancy,
in which the medications used most influenced decision-making. The medications
commonly used for the treatment of burns were evaluated for safe use in the
first trimester. In the second clinical case, the risk of premature labor due to
the stress of trauma and surgery was the main determinant in management.
Chemical prophylaxis of deep venous thrombosis is strongly recommended because of
the hypercoagulable state of pregnancy. Low-molecular-weight heparin was used in
the first case, and unfractionated heparin in the second, both of which are
considered safe for use in pregnancy1. The
use of proton-pump inhibitors or H2 inhibitors is also considered safe and
recommended for pregnant women due to the risk of gastric peptic ulcer.
In both cases, ranitidine1 was chosen. Of
the antimicrobials usually used in the treatment of burns, amikacin is known to
be teratogenic and its use should be avoided in the treatment of pregnant women,
even in topical form1.
Early grafting, preferably before 48 hours, has been shown to reduce maternal
mortality, without negatively impact on survival of the fetus7. For this reason, when the conditions of
the pregnant patient and fetus allow, we should not delay surgical procedures,
and both intraoperative and postoperative care require special attention7.
Fetal heart rate monitoring using ultrasound is recommended in the intraoperative
and immediate postoperative period, starting at 16 weeks, with continuous
cardiotocography starting at 25 weeks8.
Fetal Doppler ultrasound on admission and 2 weeks after the injury is
recommended, due to the risk of late fetal death6,9.
CONCLUSION
The reported cases illustrate the treatment of burns during two distinct phases
of pregnancy, i.e., at the beginning of pregnancy and approaching term. In the
first trimester, special attention should be given to the medications that will
be used during treatment, due to the risk of teratogenicity.
In the third trimester, fetal monitoring with cardiotocography is more important
due to the risk of fetal distress, abortion, and premature delivery. Given the
unique features of pregnancy, the complexity of burn treatment is apparent.
Although burns are best managed by prevention, greater knowledge of the
physiology of gestation allows us to properly manage burns in pregnancy.
COLLABORATIONS
|
JRNLF
|
Analysis and/or interpretation of data; statistical analyses; final
approval of the manuscript; conception and design of the study;
writing the manuscript or critical review of its contents; special
supplement (article submitter).
|
|
ELF
|
Analysis and/or interpretation of data; completion of surgeries
and/or experiments; writing the manuscript or critical review of its
contents.
|
|
GFT
|
Analysis and/or interpretation of data; final approval of the
manuscript; conception and design of the study; writing the
manuscript or critical review of its contents.
|
|
AFO
|
Analysis and/or interpretation of data; final approval of the
manuscript; conception and design of the study; writing the
manuscript or critical review of its contents.
|
|
LMF
|
Analysis and/or interpretation of data; statistical analyses; final
approval of the manuscript; conception and design of the study;
completion of surgeries and/or experiments; writing the manuscript
or critical review of its contents.
|
REFERENCES
1. Parikh P, Sunesara I, Lutz E, Kolb J, Sawardecker S, Martin JN Jr.
Burns During Pregnancy: Implications for Maternal-Perinatal Providers and
Guidelines for Practice. Obstet Ginecol Surv. 2015;70(10):633-43. DOI: http://dx.doi.org/10.1097/OGX.0000000000000219
2. Akhtar MA, Mulawkar PM, Kulkarni HR. Burns in pregnancy: effect on
maternal and fetal outcomes. Burns. 1994;20(4):351-5. DOI: http://dx.doi.org/10.1016/0305-4179(94)90066-3
3. Karimi H, Momeni M, Momeni M, Rahbar H. Burn injuries during
pregnancy in Iran. Int J Gynaecol Obstet. 2009;104:132-4. PMID: 19022440 DOI:
http://dx.doi.org/10.1016/j.ijgo.2008.10.003
4. Maghsoudi H, Smnia R, Garadaghi A, Kianvar H. Burns in Pregnancy.
Burns. 2006;32(2):246-50. DOI: http://dx.doi.org/10.1016/j.burns.2005.10.003
5. Roderique EJ, Gebre-Giorgis AA, Stewart DH, Feldman MJ, Pozez AL.
Smoke inhalation injury in a pregnant patient: a literature review of the
evidence and current best practices in the setting of a classic case. J Burn
Care Res. 2012;33(5):624-33. DOI: http://dx.doi.org/10.1097/BCR.0b013e31824799d2
6. Jain V, Chari R, Maslovitz S, Farine D; Maternal Fetal Medicine
Committee, Bujold E, et al. Guidelines for the Management of a Pregnant Trauma
Patient. J Obstet Gynaecol Can. 2015;37(6):553-74. DOI: http://dx.doi.org/10.1016/S1701-2163(15)30232-2
7. Prasanna M, Singh K. Early burn wound excision in major burns with
pregnancy: a preliminary report. Burns. 1996;22(3):234-7. PMID: 8726266 DOI:
http://dx.doi.org/10.1016/0305-4179(95)00113-1
8. Vilas Boas WW, Lucena MR, Ribeiro RC. Anestesia para cirurgia
não-obstétrica durante a gravidez. Rev Med Minas Gerais. 2009;19(3 Supl
1):S70-S79.
9. Einarson A, Bailey B, Inocencion G, Ormond K, Koren G. Accidental
electric shock in pregnancy: a prospective cohort study. Am J Obstet Gynecol.
1997;176(3):678-81. PMID: 9077628 DOI: http://dx.doi.org/10.1016/S0002-9378(97)70569-6
1. Universidade Federal de São Paulo, Escola
Paulista de Medicina, São Paulo, SP, Brazil.
Corresponding author: Andrea Fernandes
de Oliveira, Rua Napoleão de Barros, 737 - 14º andar, Vila Clementino - São
Paulo, SP, Brazil. Zip Code 04024-002. E-mail:
dra.afo@gmail.com
Article received: September 24, 2017.
Article accepted: September 5, 2018.
Conflicts of interest: none.