INTRODUCTION
Breast augmentation is the most commonly performed cosmetic surgery in the United
States and second in Brazil and worldwide1,2. Although
symmastia might have rare congenital causes, it usually results from a
complication of breast augmentation due to incorrect medial placement of
implants, which approach too closely or cross the midline, causing intermammary
sulcus loss3-5.
There are no reports in the literature regarding the incidence of iatrogenic
symmastia5. The diagnosis is
essentially clinical. It has a spectrum of intensity of symptoms, from mild
cases that go unnoticed to severe cases presenting important psychosocial
repercussions.
The main associated factors are excessive dissection of the implant plane toward
the sternum, excessive division of the medial insertion of the pectoralis major
muscle, use of implants with excessive diameter or volume, congenital symmastia,
and presence of lateral anomalous bundles of the pectoralis minor muscle4. Some factors can generally be controlled
by the surgeon, and iatrogenic symmastia can be prevented through subtle medial
dissection, which thereby prevents excessive volume or very close positioning
to
the midline4-6.
Complications such as seromas, hematomas, infections, or other factors that lead
to an increase in the pressure of plane or even a tissue adhesion rupture in
the
medial region of the plane also increase the risk of symmastia.
ObjeCtivE
To describe the experience and approach for the surgical treatment of iatrogenic
symmastia.
CASE REPORT
Work type: case series. Two patients underwent surgical symmastia repair after
breast augmentation with implants.
Patient 1
A 28-year-old patient underwent breast augmentation performed by another
surgeon with 280-mL high-profile silicone implants (retroglandular) in 2008,
and symmastia occurred. In 2009, the same surgeon changed the plane to
retromuscular, and the symmastia recurred (Figures 1 and 2).
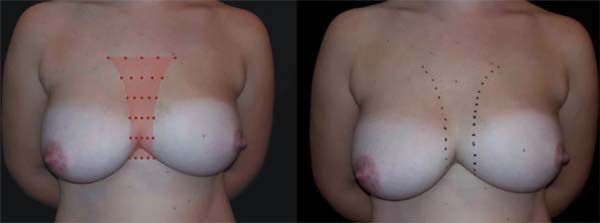
Figure 1 - Patient with visible symmastia even in static
situation.
Figure 1 - Patient with visible symmastia even in static
situation.
Figure 2 - Total loss of the intermammary sulcus in a dynamic
maneuver.
Figure 2 - Total loss of the intermammary sulcus in a dynamic
maneuver.
In 2016, she underwent surgical symmastia repair performed by the senior
author of this article. A vertical band on the sternum, approximately 4 cm
wide, was drawn (Figure 3). The access
route used was the inframammary sulcus, over a previous scar. The implants
were removed (Figure 4), and the
capsule on its anterior and posterior bands was scarified by electrocautery
(power 40, cauterization mode, electrocautery brand
Valleylab®).
Figure 3 - Marking of the region on the sternum.
Figure 3 - Marking of the region on the sternum.
Figure 4 - Implant removal, scarification of capsule surfaces, and
beginning of adhesion points.
Figure 4 - Implant removal, scarification of capsule surfaces, and
beginning of adhesion points.
Adhesion sutures were made with 3-0 nylon thread between the anterior and
posterior capsule surfaces (close to the sternum fascia) (Figure 5). Four lines with 6 sutures
each were made, comprising a vertical band approximately 4 cm wide; 420-mL
round, super-high-projection implants were inserted in the same plane (Figure 6). Delimitation and separation
of the planes was obtained, with an improved positioning of the implants, 60
days post-operatively (Figure 7).
Figure 5 - Total closure of the space between the 2 planes.
Figure 5 - Total closure of the space between the 2 planes.
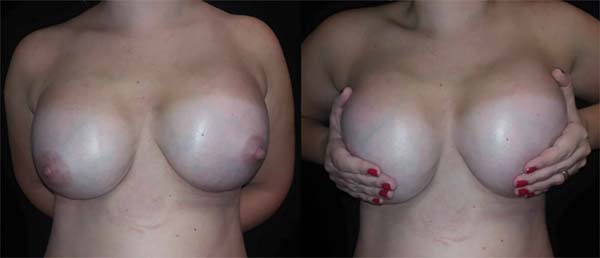
Figure 6 - Post-implant placement on the left (superoinferior view).
Delimitation of the left area is observed when lateralizing the
implant.
Figure 6 - Post-implant placement on the left (superoinferior view).
Delimitation of the left area is observed when lateralizing the
implant.
Figure 7 - Sixty days after surgery. Properly lateralized implants,
despite the maneuver to press them medially.
Figure 7 - Sixty days after surgery. Properly lateralized implants,
despite the maneuver to press them medially.
Patient 2
A 19-year-old patient underwent breast augmentation with 300-mL
retromuscular, round, high-projection implants in January 2016. This
procedure was performed by the senior author of the article. The patient
developed seroma and infection of the surgical site, requiring the removal
of the implants. Six months later, after she underwent new breast
augmentation, with implants of the same volume and maintaining the
retromuscular plane, symmastia occurred (Figure 8).
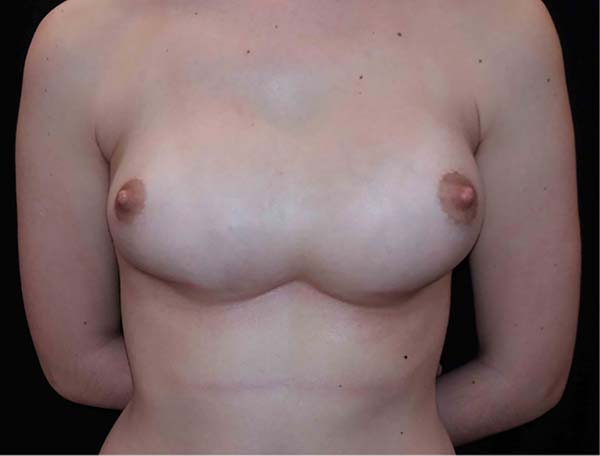
Figure 8 - Total loss of the intermammary sulcus after augmentation
mammoplasty with implants.
Figure 8 - Total loss of the intermammary sulcus after augmentation
mammoplasty with implants.
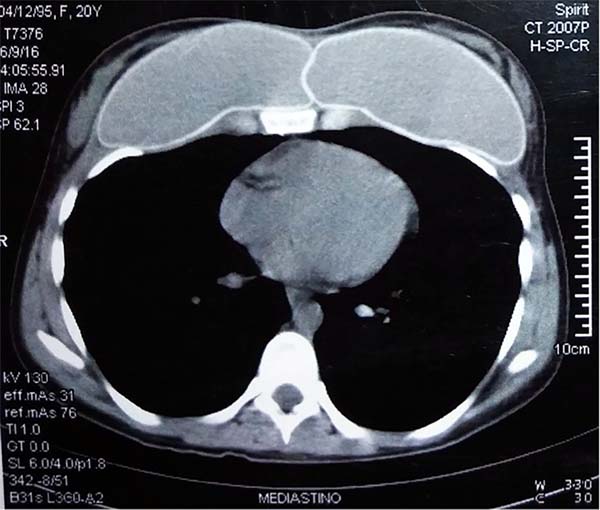
Computed tomographic examination showed total union of the planes and
medialization of the implants (Figure 9). A 2-step approach was proposed: in the first procedure, the
implants were removed, with the creation of a new medial sulcus using the
same technique (scarification of the capsule surfaces, creation of a
separation band approximately 4 cm between the planes, and creation of
adhesion sutures with nylon 3-0 thread) (Figures 10 and 11). After
3 months, 280-mL round, super-high-projection breast implants were placed in
the same plane, achieving symmastia repair and appropriate esthetic outcome
(Figure 12).
Figure 9 - CT scan showing implant plane unification.
Figure 9 - CT scan showing implant plane unification.
Figure 10 - Transoperative. Complete loss of separation between
planes.
Figure 10 - Transoperative. Complete loss of separation between
planes.
Figure 11 - Adhesion points between capsules.
Figure 11 - Adhesion points between capsules.
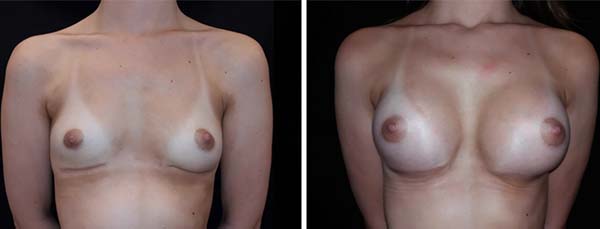
Figure 12 - Left: Post-implant removal and generation of the intermammary
sulcus. Right: Post-implant replacement (70 days after
surgery).
Figure 12 - Left: Post-implant removal and generation of the intermammary
sulcus. Right: Post-implant replacement (70 days after
surgery).
For both patients, there was no recurrence during follow-ups at 9 and 11
months, respectively, for cases 1 and 2.
DISCUSSION
Identification of risk factors for preoperative symmastia and transoperative care
are fundamental to avoid symmastia. Medial dissection should not exceed the
horizontal distance of 1.5 to 3 cm from the midpoint between the sternum angle
and the xiphoid process5.
Implants should not have dimensions that are extrapolated, as the literature
shows that most symmastia cases are associated with implants with excessive
diameter or volume4,5,7. The defect causing symmastia is usually found in the central
part. Cases of symmastia in the upper and lower parts are rarer5.
The diagnosis, in most of the cases, is evident and well defined, within 6 months
after the primary procedure. In milder cases, maneuvers such as application of
lateral pressure to both implants emphasize their anterior projection in the
presternal region4,5. There are few studies in the literature
on symmastia, and most of them are case series (Table 1).
Table 1 - Articles found in the literature on symmastia.
| Author |
Year |
Journal |
Number of cases |
| Becker |
2005 |
Plastic Reconstrutive Surgery |
5 |
| Spear |
2006 |
Plastic Reconstrutive Surgery |
20 |
| Spear et al.13 |
2009 |
Plastic Reconstrutive Surgery |
23 |
| Moliver et al.4 |
2015 |
Aesthetic Surgery Journal |
18 |
Table 1 - Articles found in the literature on symmastia.
These works proposed different surgical techniques for the treatment. There is
some agreement that the approach should be performed in a periareolar or
inframammary manner, depending on the previous incision, for adequate operative
field. Simple capsulorrhaphy may be effective and consists basically of a medial
suture between the anterior and posterior edges of medial capsule, but despite
its simplicity, its use is not very recommended due to the large number of
recurrence cases reported7,8.
Lateral and/or upper capsulotomy may be associated with decreased tension at the
medial edge. Another simple surgical option is the use of presternal
transcutaneous sutures. Their use is debatable, since the area is at high risk
for keloid formation, especially in patients with darker skin tones, despite
being recommended to minimize scars in the region.
More complex capsulorrhaphy techniques have been described to decrease the risk
of recurrence. Instead of a simple suture, using anterior and posterior flaps
that overlap on the medial breast edge, providing greater support, is possible.
However, the execution depends on a well-defined and mature capsule8,9. Another option for greater medial support is the use of a
C-shaped acellular dermal matrix in the band, which is medially fixed. Such a
technique is simple, but it adds cost to the procedure, despite its questionable
benefits10.
Replacing the implant plan can be a treatment strategy. Retroglandular implants
can be relocated to the retromuscular plane, providing better implant
coverage11,12. Retromuscular implants can be relocated
to the retroglandular plane if there is enough subcutaneous coverage6.
When there is insufficient coverage, repositioning the implants in an
intermediate plane can be attempted. Spear et al.13 described good esthetic results in their series of 23 patients
with subpectoral implants, which they attributed to the creation of
neo-subpectoral regions, a new anterior and posterior plane to the capsule to
the pectoralis major muscle, with no cases of recurrence.
Our repair procedure proposal used sutures between the anterior and posterior
capsules under the medial sulcus, which is associated with the scarification
of
their surfaces and results in a good adherence between planes. Since there are
no transcutaneous sutures, we avoided the risk of keloid formation. We believe
that promoting adhesion between capsule surfaces, i.e., their scarification,
is
important. Electrocauterization was used with the aim of promoting local
inflammation and increasing the possibility of adhesions.
The patient in case 1, who had mammary ptosis, was evaluated for the need for
simultaneous mastopexy. Because of the complexity of managing several variables
and to prevent the risk of breast devascularization, we chose to correct only
symmastia and proposed to perform mastopexy at another time, depending on the
need.
We observed that skin adhesion to the presternal region in the medial portion of
the breasts and the creation of a new sulcus reduced excess skin, which we
attribute to a mathematical explanation: the skin, in a situation of symmastia
detected in a tomographic position (caudo-cranial), forms an almost straight
line between the nipples. With symmastia repair, part of the excess skin is used
when remaking the correct curvature of the medial poles of the breasts. We also
observed a medialization of the areola-papillary complex. Such management proved
to be successful and led to good esthetic results, with the patient being
satisfied after the first surgery, with no need for a second intervention thus
far.
Patient 2 presented with significant psychological impairment, due to 3
unsuccessful surgical interventions. Thus, the maintenance of a good
doctor-patient relationship was fundamental for the therapeutic success of the
case.
The literature suggests that in certain cases of difficult resolution of
symmastia, the removal of the implants is primarily the best option, as it can
immediately improve the esthetic aspect, giving the patient the closest
semblance to the anatomy she had before breast augmentation13. When replacing the implants, we chose to use
super-high-projection ones because they have a smaller base diameter, compared
with high-projection implants, and thus occupy a smaller horizontal space.
CONCLUSION
Iatrogenic symmastia is a rare condition that has serious repercussions for the
patient; hence, its prevention is fundamental. It is difficult to conclude which
is the best technique for the correction of this condition because few studies
were published, with only a small number of cases. Although our case series is
modest, considering that this is a relatively rare condition, we believe the
technique we described can be used in the treatment of this condition, which
is
complex and has a high rate of recurrence.
COLLABORATIONS
|
MP
|
Analysis and/or interpretation of data; statistical analyses; final
approval of the manuscript; conception and design of the study;
completion of surgeries and/or experiments; writing the manuscript
or critical review of its contents.
|
|
FBF
|
Analysis and/or interpretation of data; statistical analyses; final
approval of the manuscript; conception and design of the study;
completion of surgeries and/or experiments; writing the manuscript
or critical review of its contents.
|
|
EMZ
|
Analysis and/or interpretation of data; statistical analyses; final
approval of the manuscript; conception and design of the study;
completion of surgeries and/or experiments; writing the manuscript
or critical review of its contents.
|
|
BDMG
|
Analysis and/or interpretation of data; statistical analyses; final
approval of the manuscript; conception and design of the study;
completion of surgeries and/or experiments; writing the manuscript
or critical review of its contents.
|
|
FMFN
|
Analysis and/or interpretation of data; statistical analyses; final
approval of the manuscript; conception and design of the study;
completion of surgeries and/or experiments; writing the manuscript
or critical review of its contents.
|
|
LMP
|
Analysis and/or interpretation of data; statistical analyses; final
approval of the manuscript; conception and design of the study;
completion of surgeries and/or experiments; writing the manuscript
or critical review of its contents.
|
|
RSW
|
Analysis and/or interpretation of data; statistical analyses; final
approval of the manuscript; conception and design of the study;
completion of surgeries and/or experiments; writing the manuscript
or critical review of its contents.
|
|
PBE
|
Analysis and/or interpretation of data; statistical analyses; final
approval of the manuscript; conception and design of the study;
completion of surgeries and/or experiments; writing the manuscript
or critical review of its contents.
|
REFERENCES
1. American Society of Plastic Surgeons [Internet]. American Society of
Plastic Surgeons. 2017 [cited 24 May 2017]. Available from: https://www.plasticsurgery.org
2. Surgery I. ISAPS - Sociedade Internacional de Cirurgia Plástica
Estética (ISAPS) [Internet]. Isaps.org. 2017 [cited 24 May 2017]. Available
from: http://www.isaps.org/pt/
3. Brown MH, Somogyi RB, Aggarwal S. Secondary Breast Augmentation.
Plast Reconstr Surg. 2016;138(1):119e-35e. PMID: 27348674 DOI: http://dx.doi.org/10.1097/PRS.0000000000002280
4. Moliver CL, Sanchez ER, Kaltwasser K, Sanchez RJ. A Muscular
Etiology for Medial Implant Malposition Following Subpectoral Augmentation.
Aesth Surg J. 2015;35(7):NP203-10. DOI: http://dx.doi.org/10.1093/asj/sjv072
5. Selvaggi G, Giordano S, Ishak L. Synmastia: prevention and
correction. Ann Plast Surg. 2010;65(5):455-61. DOI: http://dx.doi.org/10.1097/SAP.0b013e3181d37648
6. Lesavoy MA, Trussler AP, Dickinson BP. Difficulties with subpectoral
augmentation mammaplasty and its correction: the role of subglandular site
change in revision aesthetic breast surgery. Plast Reconstr Surg.
2010;125(1):363-71. PMID: 20048627 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181c2a4b0
7. Foustanos A, Zavrides H. Surgical reconstruction of iatrogenic
symmastia. Plast Reconstr Surg. 2008;121(3):143e-144e. PMID: 18317108 DOI:
http://dx.doi.org/10.1097/01.prs.0000300199.69982.48
8. Yoo G, Lee PK. Capsular flaps for the management of malpositioned
implants after augmentation mammoplasty. Aesth Surg J. 2010;34(1):111-5. DOI:
http://dx.doi.org/10.1007/s00266-009-9456-3
9. Parsa FD, Koehler SD, Parsa AA, Murariu D, Daher P. Symmastia after
breast augmentation. Plast Reconstr Surg. 2011;127(3):63e-65e. PMID: 21364388
DOI: http://dx.doi.org/10.1097/PRS.0b013e31820635b5
10. Curtis MS, Mahmood F, Nguyen MD, Lee BT. Use of AlloDerm for
correction of symmastia. Plast Reconstr Surg. 2010;126(4):192e-193e. DOI:
http://dx.doi.org/10.1097/PRS.0b013e3181ea92a3
11. Harley OJ, Arnstein PM. Retrocapsular pocket to correct symmastia.
Plast Reconstr Surg. 2011;128(1):329-31. PMID: 21701362 DOI: http://dx.doi.org/10.1097/PRS.0b013e3182174661
12. Parsa FD, Parsa AA, Koehler SM, Daniel M. Surgical correction of
symmastia. Plast Reconstr Surg. 2010;125(5):1577-9. PMID: 20440189 DOI:
http://dx.doi.org/10.1097/PRS.0b013e3181d513f0
13. Spear SL, Dayan JH, Bogue D, Clemens MW, Newman M, Teitelbaum S, et
al. The "neosubpectoral" pocket for the correction of symmastia. Plast Reconstr
Surg. 2009;124(3):695-703. PMID: 19363454 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181a8c89d
1. Universidade Federal de Ciências da Saúde de
Porto Alegre, Porto Alegre, RS, Brazil.
2. Santa Casa de Misericórdia de Porto Alegre,
Porto Alegre, RS, Brazil.
3. Universidade de Passo Fundo, Passo Fundo, RS,
Brazil.
4. Pontifícia Universidade Católica do Rio Grande
do Sul, Porto Alegre, RS, Brazil.
5. Universidade Federal de São Paulo, São Paulo,
SP, Brazil.
Corresponding author: Felipe Bilhar
Fasolin
Rua General Lima e Silva, 757, apto 1207 - Cidade Baixa
Porto Alegre, RS, Brazil Zip Code 90050-101
E-mail: felipefasolin@hotmail.com
Article received: October 09, 2017.
Article accepted: May 17, 2018.
Conflicts of interest: none.