ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Canthopexy and tarsal reinforcement using a periosteal flap
Cantopexia e reforço tarsal com retalho de periosteo
Original Article -
Year2013 -
Volume28 -
Issue
1
Vera Lucia Noccm Cardim1; Khaled Bazzi2; Alessandra dos Santos Silva3; Mariana Gomes e Silva2; Fernanda Martins dos Santos2; Rolf Lucas Salomons3; Adriano de Lima e Silva3; Rodrigo de Faria Valle Dornelles4
ABSTRACT
INTRODUCTION: The low resistance of the palpebral tissues to the retractable forces of postoperative scarring can predispose patients to undesirable surgical outcomes. Among the more effective techniques for solving this issue are the periosteal flaps. This report aims to present a technique for canthopexy and tarsal reconstitution using a periosteal flap to obtain a consistent and definitive reinforcement of the tarsal ligament and its continuity to the inner face of the sidewall of the orbit.
METHODS: From July 2009 to December 2012, 49 patients underwent canthopexy with flap rotation of the arcus marginalis of the inferior tarsus. The functional and aesthetic results were evaluated together with the presence of complications.
RESULTS: Eighty-four cantopexies and tarsal reinforcements using a periosteal flap were performed in 49 patients. No complications such as hematoma, infection, or necrosis were observed. Complete remission of the preoperative signals was observed in 45 (91.8%) patients, while the other 4 (8.2%) showed partial remission on at least one of the sides related to prior ocularis paralysis.
CONCLUSIONS: Canthopexy reinforced by a tarsal periosteal flap provides good tarsal ligament reconstitution with appropriate positioning of the outer corner and good contact of the eyelid with the ocular globe.
Keywords:
Blepharoplasty. Ectropion/surgery. Eyelids/surgery. Periosteum/surgery.
RESUMO
INTRODUÇÃO: A pouca resistência dos tecidos palpebrais quando submetidos ao poder retrátil dos planos cicatriciais predispõe a resultados cirúrgicos indesejáveis. Dentre as técnicas mais resolutivas destacam-se as que utilizam retalhos de periósteo. O presente artigo tem por objetivo apresentar uma técnica de cantopexia e reconstituição tarsoligamentar com retalho de periósteo, a fim de obter um reforço consistente e definitivo do tarso e sua continuidade tecidual à face interna da parede lateral da órbita.
MÉTODO: No período de julho de 2009 a dezembro de 2012, foram operados pacientes candidatos à realização de cantopexia com rotação de retalho do arcus marginalis sobre o tarso inferior. Foram avaliados os resultados estéticos e funcionais, bem como a presença de complicações.
RESULTADOS: Foram realizadas 84 cantopexias e reforço tarsal com retalho de periósteo, em 49 pacientes. Não foram observadas complicações, como hematoma, infecção ou necrose. Remissão total dos sinais pré-operatórios foi verificada em 45 (91,8%) pacientes e 4 (8,2%) apresentaram remissão parcial em pelo menos um dos lados, relacionada à prévia paresia orbicular.
CONCLUSÕES: A cantopexia com reforço tarsal com retalho de periósteo proporciona boa reconstituição tarsoligamentar, com posicionamento adequado do canto externo e bom contato da pálpebra com o bulbo ocular.
Palavras-chave:
Blefaroplastia. Ectrópio/cirurgia. Pálpebras/cirurgia. Periósteo/cirurgia.
INTRODUCTION
Lateral canthopexy is a widely used procedure for the treatment and prevention of various disorders of the lower eyelid in reconstructive and cosmetic surgery1. There are several techniques for positioning and tightening the outer corner of the eyelid from simple points of attachment to the tarsus and periosteal flaps. In all of these techniques, the lateral canthal ligament is suspended or reinserted at the level of the Whitnall's tubercle on the inner side of the orbital rim.
Bick2 and Tenzel3 contributed to the popularization of lateral canthopexy. Many surgeons perform it routinely during lower blepharoplasty or transpalpebral elevation of the middle third4-8.
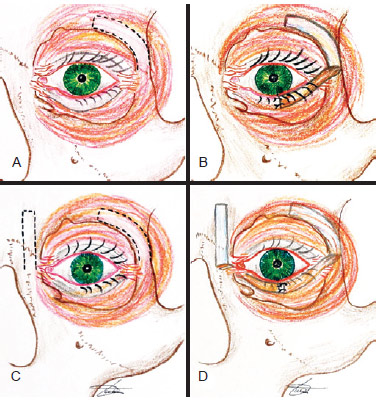
This report aims to present a technique of tarsal reconstitution using a periosteal flap to obtain a consistent and definitive tarsal reinforcement and tissue continuity to the inner face of the sidewall of the orbit (Figure 1).
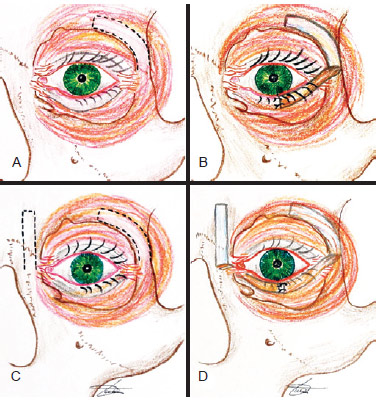
Figure 1 - Illustration of the surgical technique. In A, demarcation of the periosteal flap on the inner side of the orbit; In B, the positioned flap; In C, demarcation of the medial and lateral periosteal flaps; In D, positioned flaps (eyelid suspension "on clothesline" technique).
METHODS
From July 2009 to December 2012, all patients who were eligible for canthopexy underwent the technique described below and were included in this study. The following criteria were used for the indication of canthopexy: eligibility for transpalpebral elevation of the middle third of the face with tarsal laxity (snap test positive), lagophthalmos, canthal dystopia, ectropion, and loss of substance of the lower eyelid.
Patients were grouped into primary or secondary cases according to the indication for surgery and were evaluated for aesthetic and functional results (remission of signs and symptoms) as well as the presence of complications. The postoperative follow-up examination was conducted at an ambulatory care center in the first week and then monthly until the third month and semiannually until the second year. Photographs were taken preoperatively and at 3 and 6 months after surgery.
Surgical Technique
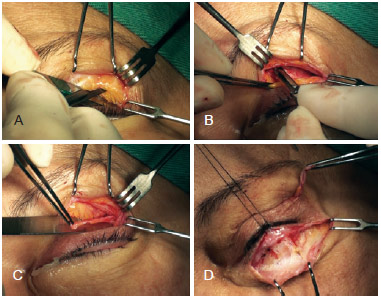
The procedure was performed under local anesthesia when isolated, and under sedation or general anesthesia depending on the associated surgeries and each patient's preference. The upper eyelid skin was incised in the palpebral crease to separate the orbicularis muscle in the direction of its fibers. The superolateral orbital margin was exposed and then the periosteum was incised with a scalpel to laterally transverse the bone crest to the supraorbital nerve until the lateral margin of the orbit above the external canthal ligament insertion was revealed. This point corresponds to the ligament insertion to be reinforced. The periosteum, or more specifically the arcus marginalis, was detached from the internal face of the orbital rim and a second incision parallel to the first one was made with an iris scissors or scalpel to delimit a 5-6-mm wide flap. The 2 incisions were united at the medial extremity and the flap remained pedicled in the inner lateral margin of the orbit just above the insertion of the lateral canthal ligament (Figure 2).
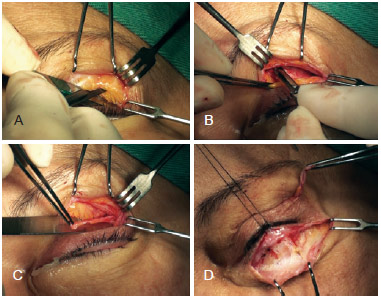
Figure 2 - In A, incision of the distal longitudinal edge of the periosteum flap in the orbital rim; In B, incision of the proximal edge of the flap on the inner orbit (arcus marginalis), after subperiosteal detachment; In C, preserving the lateral pedicle in the region of Whitnall's tubercle; In D, exposure of the lower eyelid tarsus.
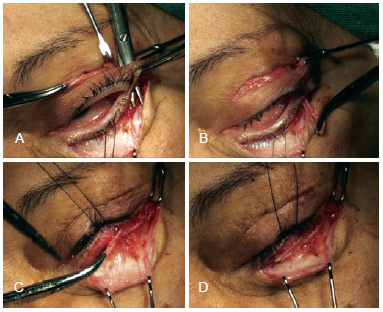
The lower eyelid incision was made as close as possible to the ciliary margin to detach the orbicularis muscle from the tarsus. A tunnel was made by divulsion with scissors, passing behind the skin and the orbicular bridge between the 2 skin incisions and ending at the front of the lateral extremity of the inferior tarsus. Through this tunnel, the flap was passed and distended on the tarsus and a stitch was made using a 6-0 nylon suture ligating its base to the lateral extremity of the tarsus. This stitch defined the correlation between the outer corner of the eyelid and the orbital margin as well as the tension given to the tarsal margin. Another 2 stitches were used to fixate the flap medially to the tarsus to ensure good contact between them (Figure 3). When canthopexy was performed as an isolated procedure, the skin incisions were sutured at this point. In contrast, if the canthopexy was performed together with other procedures, these were conducted sequentially (Figure 4).
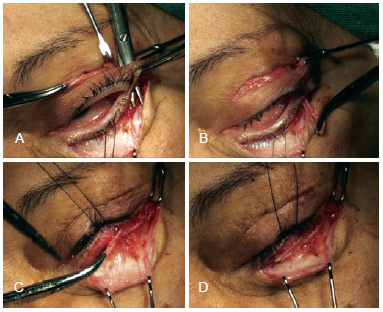
Figure 3 - In A, creation of a tunnel between the orbicularis muscle and the lateral canthal ligament; In B, transposition of the flap to the lower eyelid; In C, attachment of the flap near the tarsus; In D, the positioned flap.

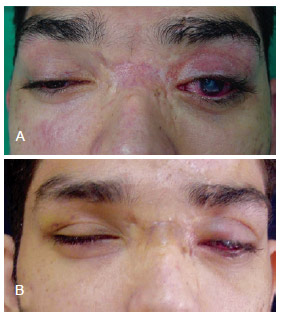
Figure 4 - A patient with canthal dystopia and lagophthalmos who underwent canthopexy with an arcus marginalis flap and a skin graft. In A, C, and E, preoperative aspect; In B, D, and F, 3-month postoperative appearance.
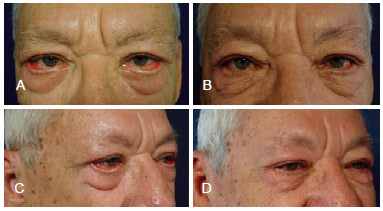
In patients in whom large tarsal ligament laxity was noted during the snap test, shortening of the eyelid margin was performed in an associated manner using the Kuhnt-Szymanowski technique (Figure 5). In those patients who underwent medial periosteal canthopexy, another periosteal flap was made vertically above the medial canthal ligament and the anterior glabella (Figures 1C and 1D). The tunnel for the flap transposition passed between the orbicularis muscle and the medial canthal ligament to preserve the tear ducts. The fusion of the extremities of the medial and lateral flaps at the center of the eyelid was intended to strengthen the tarsus along its length (eyelid suspension "on clothesline") (Figure 6).
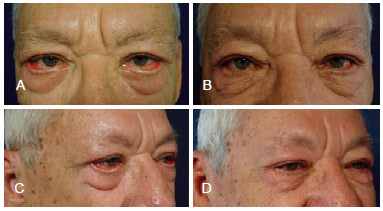
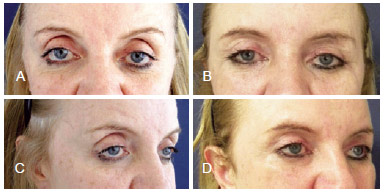
Figure 5 - A patient with severe ectropion who underwent lateral canthopexy using a periosteal flap and reduction of the eyelid margin using the Kuhnt-Szymanowski technique. In A and C, preoperative appearance; In B and D, 6-month postoperative appearance.
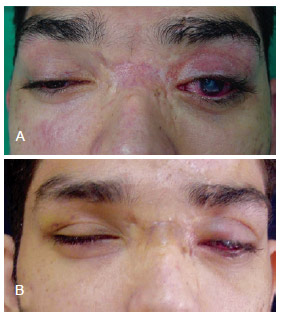
Figure 6 - A patient with posttraumatic buphthalmos and insufficient occlusion of the left eyelid who underwent lateral and medial canthopexy using periosteal flaps. In A, preoperative appearance; In B, 3-month postoperative appearance.
RESULTS
Eighty-four canthopexies and tarsal reinforcements using periosteal flaps were performed in 49 patients. The patients were aged 7-89 years. The following were the indications for surgery: prophylactic (tarsal laxity) in 19 patients, loss of substance of the lower eyelids in 10 patients, ectropion in 7 patients, lagophthalmos in 7 patients, and canthal dystopia in 6 patients. Seventeen patients (34.7%) were considered secondary cases. Associated horizontal eyelid shortening was performed in 6 patients (12.2%). Four patients (8.2%) with a large degree of insufficient lid sealing also underwent medial canthopexy using a periosteal flap (suspension "on clothesline" technique). No procedure-related complications including hematoma, infection, or necrosis were noted. Chemosis was observed in 71.4% of the patients in the immediate postoperative period. Edema persisted for 2-3 weeks and lasted longer in older patients and smokers.
Complete remission of the preoperative signals was observed in 45 patients (91.8%), although 4 patients (8.2%) showed partial remission on at least one side related to previous orbicular paralysis.
DISCUSSION
The lid is composed of thin and compliant structures. The contractile capacity of the scar tissue that usually forms after a surgical procedure in this region can overcome the resistance of the palpebral tissues, resulting in retraction and lagophthalmos9. For this reason, it becomes necessary to find better eyelid support, both in cases of dystopia and in cases of tarsal laxity.
The simple technique of suturing the canthal ligament to the periosteum presents some difficulty because of the small space in that region and the low ability to adjust the tarsal tension after suture. Moreover, the results of these techniques are susceptible to early or late dehiscence and are highly dependent on the tissue resistance to shear with the tarsal suture1. For this reason, some authors advocate local periosteal flaps to technically facilitate the canthopexy procedure and prevent dehiscence10-13.
The periosteum of the outer face of the orbit is a structure that is commonly used in the reconstruction of the lateral and medial canthal ligament14. Lemke et al.12 in 1999 and Game & Morlet1 in 2007 described the use of short flaps of the periosteum overlying the tarsal strip to rebuild a new lateral canthal ligament and prevent dehiscence. As in these techniques, the flap proposed in this paper provides some advantages over conventional canthopexy using sutures. Among these advantages are the continuity of the tarsal tissue to the orbital rim, greater stretch control, and tarsal laxity correction, by not only lateral traction but also the incorporation of periosteal tissue into the tarsus. The role of the suture connecting the flap to the tarsus is to unite the tissue for the healing process rather than to provide long-term tension. Furthermore, a flap vector that is superiorly oriented and held fixed in the region of Whitnall's tubercle better simulates the anatomy of the lateral canthal ligament in contrast with the other periosteal flap described by some authors1,11,13.
The region of the periosteum used to create the flap corresponds to the arcus marginalis. This structure is a fusion zone of the periosteum, orbital septum, and periorbital region that forms an inelastic and resistant ligament. Its anatomical position allows for the creation of a flap based on the inner wall of the orbit. This allows the flap, after being fixed to the lower tarsus, to approximate the outer corner of the eyelid to the eyeball and restore contact between the tarsal and the sclera conjunctiva. Furthermore, the septectomy that results from their preparation releases the upper-lateral fat bags, which diminishes the hollowed appearance of the orbit (Figure 7).
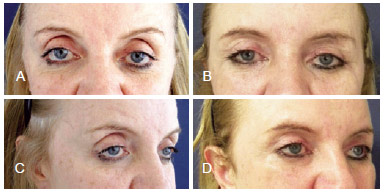
Figure 7 - A patient with scleral exposure and orbital hollow subjected to lateral orbital canthopexy by the proposed technique and transpalpebral elevation of the middle third. In A and C, preoperative appearance; In B and D, 6-month postoperative appearance
Since it provides a sturdy anchor of the tarsus to the orbital margin, the technique in the current study is of special importance in secondary cases and when it becomes necessary to reinsert the lateral canthal ligament because of trauma to correct an antimongolic fissure. It also represents a simpler alternative to other techniques described for the reintegration of the canthal ligament that require the creation of a hole in the bone for the passage of the suture, and its results are less prone to dehiscence since its suture is less vulnerable due to the incorporation of tissue into the tarsus and the distribution of the forces of tension7,15.
CONCLUSIONS
Canthopexy with tarsal reinforcement using a periosteal flap provides good tarsal reconstitution as well as adequate positioning of the outer corner of the eyelid and good contact with the eyeball.
REFERENCES
1. Game J, Morlet N. Lateral canthal fixation using an oblique vertically orientated asymmetric periosteal transposition flap. Clin Experiment Ophthalmol. 2007;35(3):204-7.
2. Bick MW. Surgical management of orbital tarsal disparity. Arch Ophthalmol. 1966;75(3):386-9.
3. Tenzel RR. Treatment of lagophthalmos of the lower lid. Arch Ophthalmol. 1969;81(3):366-8.
4. McCord CD, Boswell CB, Hester TR. Lateral canthal anchoring. Plast Reconstr Surg. 2003;112(1):222-37.
5. Cardim VLN. Blefaroplastia subperiostal. Rev Soc Bras Cir Plast. 1996;11(2):7-14.
6. Hester TR Jr, Codner MA, McCord CD, Nahai F, Giannopoulos A. Evolution of technique of the direct transblepharoplasty approach for the correction of lower lid and midfacial aging: maximizing results and minimizing complications in a 5-year experience. Plast Reconstr Surg. 2000;105(1):393-406.
7. Flowers RS. Canthopexy as a routine blepharoplasty component. Clin Plast Surg. 1993;20(2):351-65.
8. Fagien S. Algorithm for canthoplasty: the lateral retinacular suspension: a simplified suture canthopexy. Plast Reconstr Surg. 1999;103(7):2042-53.
9. Hwang K, Nam YS, Kim DJ, Han SH, Hwang SH. Anatomic study of the lateral palpebral raphe and lateral palpebral ligament. Ann Plast Surg. 2009;62(3):232-6.
10. Leone CR Jr. Lateral canthal reconstruction. Ophthalmology. 1987;94(3):238-41.
11. Leone CR Jr. Periosteal flap for lower eyelid reconstruction. Am J Ophthalmol. 1992; 114(4):513-4.
12. Lemke BN, Sires BS, Dortzbach RK. A tarsal strip-periosteal flap technique for lateral canthal fixation. Ophthalmic Surg Lasers. 1999;30(3):232-6.
13. Marsh JL, Edgerton MT. Periosteal pennant lateral canthoplasty. Plast Reconstr Surg. 1979;64(1):24-9.
14. Leibsohn JM, Hahn F. Medial canthal tendon reconstruction with nasal periosteum. Ophthal Plast Reconstr Surg. 1992;8(1):35-40.
15. McCord CD, Ford DT, Hanna K, Hester TR, Codner MA, Nahai F. Lateral canthal anchoring: special situations. Plast Reconstr Surg. 2005; 116(4):1149-57.
1. Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP) and the Brazilian Association of Craniomaxillofacial Surgery (ABCCMF), Doctor in general surgery by the Faculty of Medical Sciences of Santa Casa de São Paulo (FCMSCSP), postdoctoral fellow at the FCMSCSP, responsible for the Lato Sensy post-graduate degree craniofacial surgery of the Portuguese beneficence of São Paulo and by the Center for Advanced Plastic (NPA), São Paulo, SP, Brazil
2. Plastic surgeon, associate member of the SBCP, post-graduate in craniofacial surgery by the Portuguese beneficence of São Paulo, São Paulo, SP, Brazil
3. Plastic surgeon, full member of the SBCP and ABCCMF, medical assistant of the NPA, São Paulo, SP, Brazil
4. Plastic surgeon, full member of the SBCP and ABCCMF, master of plastic surgery by the Faculty of Medicine of the University of São Paulo (FMUSP), medical assistant of the NPA, São Paulo, SP, Brazil
Correspondence to:
Vera Lucia Nocchi Cardim
Rua Augusta, 2709 - cj. 42 - Cerqueira César
São Paulo, SP, Brazil - CEP 01413-100
E-mail: vera@npa.med.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article submitted: January 6, 2013
Article accepted: February 27, 2013
This study was performed at the Portuguese Beneficent Hospital of São Paulo, São Paulo, SP, Brazil.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license