ABSTRACT
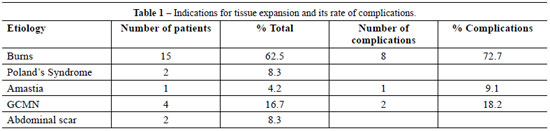
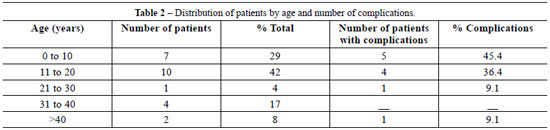
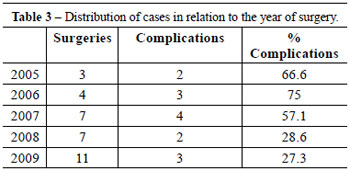
Background: The shortage of tissue for large defect reconstruction is a challenge for the plastic surgeon. Tissue expansion emerged in this context, and in the last 30 years has become one of the most widely used modalities in reconstructive surgery. Tissue expansion is a very versatile technique that can be performed in patients of all ages for the correction of different pathologies. The most common indications are burn sequelae and giant congenital nevus. The present study describes the indications and use of tissue expanders at the Hospital de Clínicas of Universidade Federal do Paraná. Methods: Patients who underwent tissue expansion for reconstructive surgery between January 2005 and December 2009 were retrospectively reviewed. Results: A total of 24 patients (70.8% female and 29.2% male) were analyzed. Ages ranged from 3 to 46 years old (average, 17.1 years). The most common indication for tissue expansion was the treatment of burn sequelae (62.5%), mainly in the head and neck. Alopecia was the second most prevalent indication (29.2%), followed by scar retraction in the neck (20.8%). Other indications were giant congenital melanocytic nevus (16.7%), Poland's syndrome (8.3%), abdominal scar (8.3%), and amastia (4.2%). Complications developed in 11 patients, and the highest incidence of complications, reported in 8 (72.7%) patients, was among those with burn sequelae as the primary pathology. The complications were infection, rupture, extrusion, wound dehiscence, and displacement of the expander. Conclusions: Tissue expansion is indicated for the treatment of several diseases among which burn sequelae is one of the most common indications.
Keywords:
Tissue expansion devices. Tissue expansion. Reconstructive surgical procedures.
RESUMO
Introdução: A escassez de tecidos para reconstrução de grandes defeitos é um desafio ao cirurgião plástico. Nesse contexto, surgiu a expansão tecidual, que, nos últimos 30 anos, se tornou uma das modalidades mais utilizadas na cirurgia reparadora. A expansão é uma técnica muito versátil, que pode ser realizada em todas as idades e para correção de diferentes afecções. As principais indicações são sequelas de queimadura e nevo congênito gigante. Este estudo teve como objetivo demonstrar as indicações na utilização dos expansores tissulares e sua evolução em pacientes do Hospital de Clínicas da Universidade Federal do Paraná. Métodos: Estudo retrospectivo, incluindo pacientes submetidos a expansão tecidual para cirurgia reconstrutora, no período de janeiro 2005 a dezembro 2009. Resultados: Foram analisados 24 pacientes, sendo 70,8% do sexo feminino e 29,2% do sexo masculino. A idade variou entre 3 anos e 46 anos (média de 17,1 anos). A principal indicação de expansão tecidual foi o tratamento de sequelas de queimaduras (62,5%), principalmente na região da cabeça e do pescoço. Alopecia foi a indicação mais prevalente (29,2%), seguida por retração cicatricial em região cervical (20,8%). Outras indicações foram nevo melanocítico congênito gigante (16,7%), síndrome de Poland (8,3%), cicatriz abdominal (8,3%) e amastia (4,2%). Entre os pacientes avaliados, 11 evoluíram com alguma complicação, 8 (72,7%) dos quais tinham como doença primária sequela de queimaduras, demonstrando maior incidência de complicações em relação às outras indicações. As complicações encontradas foram: infecção, ruptura, extrusão, deiscência de sutura e deslocamento do expansor. Conclusões: A expansão tissular é indicada no tratamento de múltiplas doenças e uma das principais indicações continua sendo o tratamento de sequelas de queimaduras.
Palavras-chave:
Dispositivos para expansão de tecidos. Expansão de tecido. Procedimentos cirúrgicos reconstrutivos.