

Case Report - Year 2022 - Volume 37 -
Reverse sural flap as an alternative to microsurgical reconstruction of extensive foot wound after electrical burn: case report
Retalho sural reverso como alternativa à reconstrução microcirúrgica de ferimento extenso em pé após queimadura elétrica: relato de caso
ABSTRACT
Introduction: To present a reverse sural flap case report as an alternative to microsurgical flap in foot reconstruction after electrical trauma. The report presented is of a patient treated by the Burns and Complex Wounds groups of the Plastic Surgery Service of the Hospital das Clínicas of the Faculty of Medicine of the University of São Paulo in 2020.
Case Report: Male patient, 35 years old, without comorbidities, victim of high voltage electrical trauma (1300V) at home, affecting upper and lower limbs bilaterally. Due to the severity of the injuries, he underwent left transtibial amputation and serial debridement in the contralateral limb, resulting in a defect in the medial face, hallux and entire dorsum of the right foot, with bone exposure. Due to the failure of reconstruction with a microsurgical flap of the vastus lateralis muscle, reconstruction with a reverse sural flap was chosen. It evolved with distal necrosis, requiring new debridement and re-advancement of the flap. In the follow-up, he presented a favorable evolution and is in the process of rehabilitation.
Conclusion: The reverse sural flap proved to be suitable for the salvage treatment of extensive foot injuries after the failure of microsurgical therapy, offering stable coverage and excellent contour, thus allowing satisfactory patient rehabilitation.
Keywords: Burns; Wounds and injuries; Surgical flaps; Reconstructive surgical procedures; Wound closure techniques; Tissue transplantation.
RESUMO
Introdução: Apresentar um relato de caso de confecção de retalho sural reverso como alternativa ao retalho microcirúrgico na reconstrução de pé após trauma elétrico. O relato apresentado é de um paciente atendido pelos grupos de Queimaduras e Feridas Complexas do Serviço de Cirurgia Plástica do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, no ano de 2020.
Relato de Caso: Paciente masculino, 35 anos, sem comorbidades, vítima de trauma elétrico de alta voltagem (1300V) em domicílio, acometendo membros superiores e inferiores bilateralmente. Devido à gravidade das lesões, foi submetido a amputação transtibial à esquerda e desbridamentos seriados no membro contralateral, resultando em defeito em face medial, hálux e todo dorso do pé direito, com exposição óssea. Devido ao insucesso de reconstrução com retalho microcirúrgico de músculo vasto lateral, optou-se por reconstrução com retalho sural reverso. Evoluiu com necrose distal, sendo necessário novo desbridamento e reavanço do retalho. No seguimento, apresentou evolução favorável, e está em processo de reabilitação.
Conclusão: O retalho sural reverso mostrou-se adequado para o tratamento de resgate de lesão extensa em pé após falha da terapia microcirúrgica, oferecendo cobertura estável e ótimo contorno, permitindo, assim, reabilitação satisfatória do paciente.
Palavras-chave: Queimaduras; Ferimentos e lesões; Retalhos cirúrgicos; Procedimentos cirúrgicos reconstrutivos; Técnicas de fechamento de ferimentos; Transplante de tecidos
INTRODUCTION
Electrical trauma can range from minor skin burns to severe organic injuries1. Contact with high voltage electrical current (>1000 volts) can generate massive tissue necrosis and exposure of noble structures, especially at the point of contact. The extremities are typically the most affected areas2. Limb amputation is reported in up to 40% of patients suffering from high voltage electrical trauma. In order for these cases to be treated correctly, with the prevention of sequelae and rehabilitation, they must be followed up in referral centers for burns, ideally with a hand surgery service3.
Reconstruction of lower limbs, especially the foot, is challenging due to the need to cover specialized structures in an area with little excess skin. Reconstruction using flaps is the best alternative for limb salvage. The flap choice should be based on the needs of the recipient area and the availability of donor areas. Free flaps have great relevance in reconstructing the distal third of the lower limbs due to the limited options for local flaps and the availability of soft tissues4. Electrical trauma and vascular diseases are relative contraindications for the latter option5.
OBJECTIVE
This study aims to present a case report of making a reverse sural flap as an alternative to a microsurgical flap in foot reconstruction after electrical trauma. The report presented is of a patient treated by the Burns and Complex Wounds groups of the Plastic Surgery Service of the Hospital das Clínicas of the Faculty of Medicine of the University of São Paulo (HCFMUSP) in the year 2020.
CASE REPORT
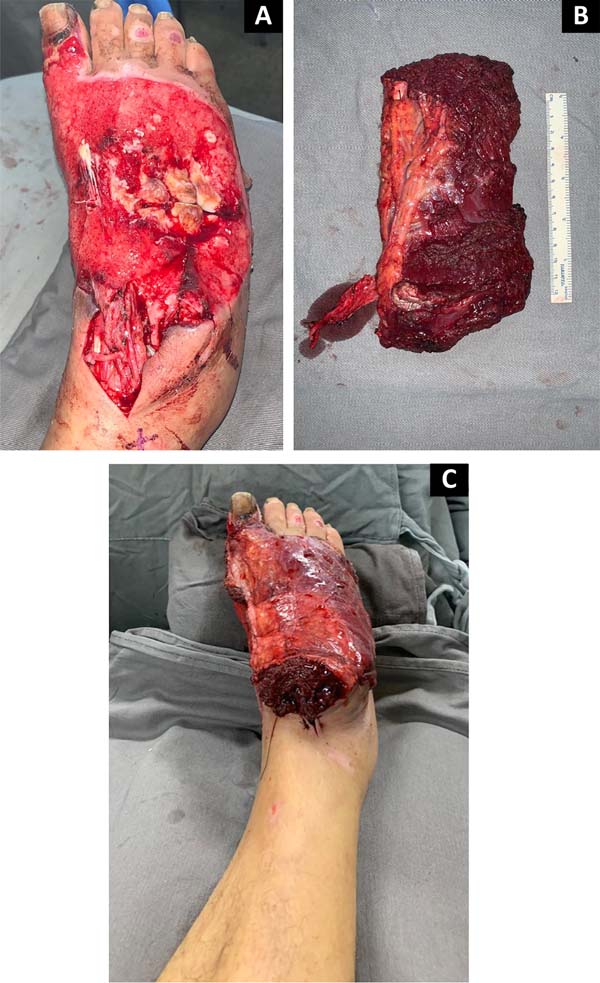
Male patient, 35 years old, smoker, victim of high voltage electrical trauma (1300V) at home. Brought to the emergency room of HCFMUSP by aeromedical transport with bilateral upper and lower limb burns (burned body surface totaling 8%). He had no other injuries resulting from the trauma and remained hemodynamically stable. He evolved with critical ischemia of the left lower limb, requiring transtibial amputation by the Vascular Surgery team. In treating the other injuries, he underwent serial debridement in the contralateral limb, resulting in a defect on the right foot’s medial face, hallux, and entire dorsum, with bone exposure (Figure 1).
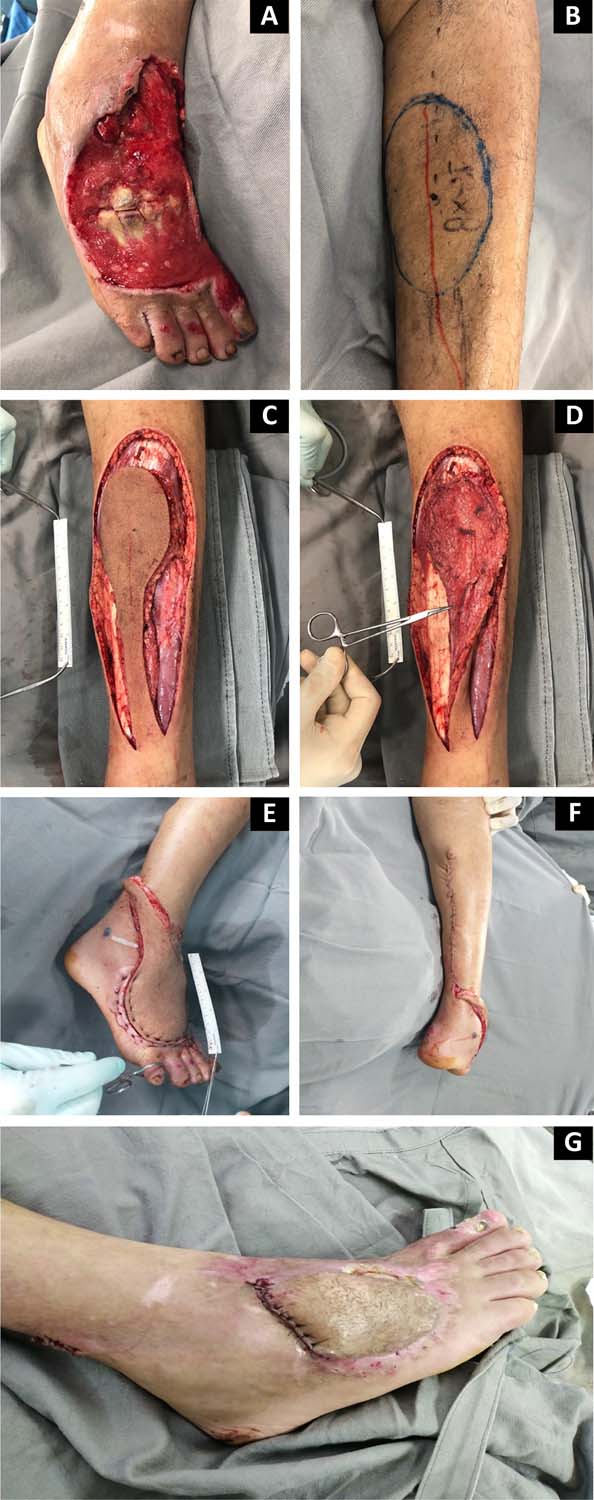
Thirty days after the trauma, to avoid amputation of the other extremity, reconstruction with a microsurgical flap of the vastus lateralis muscle was chosen, with anastomosis in the anterior tibial artery and the great saphenous vein (Figure 2). The flap showed no tissue perfusion on the third postoperative day, and venous thrombosis was identified. We opted for flap debridement and placement of negative pressure therapy for 5 days. Then, the defect was covered with a reverse sural flap to rescue the limb (Figure 3), whose skin island measured 12 x 8 cm and pedicle dissection up to 8 cm from the lateral malleolus. The donor area was closed primarily. A partial skin graft was performed in a lamina to cover the medial face and hallux.
On the eighth postoperative day of the last surgical approach, the patient was discharged from the hospital. During outpatient follow-up, at the first return visit, an area of v enous congestion and distal necrosis of the flap was observed, initially opting for treatment using topical enzymatic debriding agents (papain gel 10%) and autolytic agents (hydrocolloid). After 30 days, with lesion delimitation and bed preparation, a new surgical approach was performed for debridement and flap advancement (Figure 4). After 90 days of the initial surgery, the release of the vascular pedicle was performed. The patient presents a satisfactory evolution in outpatient follow-up after 5 months, with stable coverage, excellent contour of the right foot, and is in the rehabilitation process (Figure 5).
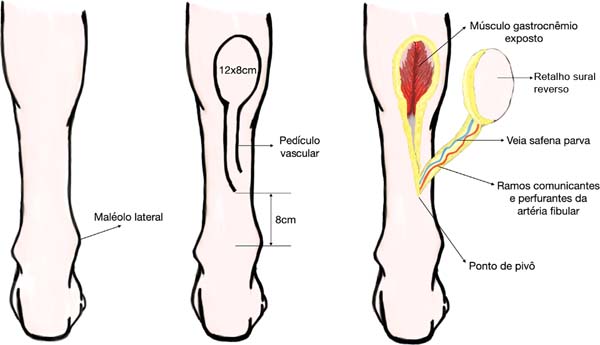
Surgical technique - reverse sural flap (Figure 6)
The patient underwent the procedure under general anesthesia. After being positioned in the left lateral decubitus position, the usual preparations were performed to keep the entire lower limb exposed in the operative field. Initially, surgical debridement of the lesion was performed with abundant irrigation with 0.9% saline and collected cultures from soft tissue samples. The defect area was estimated to demarcate the flap according to the necessary and sufficient dimensions to cover the entire lesion (12 x 8 cm), without excessive traction of the pedicle, with the skin island being drawn in the middle and proximal third of the leg, between the bellies medial and lateral of the gastrocnemius muscle.
Flap dissection was initiated by incising the skin at the proximal edge of the flap until it penetrated the deep fascia. The small saphenous vein and the sural nerve were identified in the center of the flap and ligated proximally. During the dissection, visualization of the pedicle was maintained to remain intact up to the rotation point. Cutaneous perforators, branches of the fibular artery responsible for vascularization of the flap, are frequently found on the posterolateral margin of the distal region of the leg.
Interpolation of the flap was performed for the defect area, with a rotation point 8 cm cranially to the lateral malleolus, and the flap was sutured over the bed to cover the exposed deep structures (metatarsals) with “U” stitches of non-absorbable mononylon thread. 3-0. Closure of the donor area was primary, with suturing in layers without excessive tension. In the other areas of granulation tissue, a partial skin graft was performed (donor area on the right thigh).
The study was approved by the Research Ethics Committee of the Hospital das Clínicas, Faculty of Medicine, University of São Paulo, under protocol number 35074420.1.0000.0068.
DISCUSSION
Electrical injuries to the lower limbs, especially the foot, often present with necrosis of tendons, muscles, and bone tissues, most of which are combined with extensive damage to the skin and local soft tissues. Injuries to deep structures, lack of local flaps, vascular damage, and unreliable blood supply make the treatment of foot injuries, especially medial and distal injuries, extremely difficult6.
Reconstruction of lower limbs with local flaps is limited by low tissue availability, associated with deficient vascularization in trauma and the presence of comorbidities. Muscle flaps are restricted to coverage in the proximal and middle thirds of the leg. The distal third of the leg and foot are mostly reconstructed using distant flaps. However, this type of reconstruction is laborious and is reserved for specialized centers7. In burn patients, microsurgical flaps should be indicated when there is the exposure of noble structures to preserve the function of the affected limb, with adequate results after correct planning, and performed in reference centers8.
In the case reported, due to the extensive distal defect in the foot with exposure of important structures caused by electrical trauma, reconstruction with a free flap was initially chosen to avoid extremity amputation. The microsurgical flap was chosen because it provides well-vascularized tissue for better coverage of the defect, associated with favorable local conditions, with the presence of adequate receptor vessels. However, after initial treatment failure, it was decided to perform reconstruction with a reverse sural flap to save the limb and provide good quality coverage and adequate contour for the affected region.
The use of fasciocutaneous flaps from the sural angiosome with a distal (or reverse) base is an alternative for covering defects in the lower third of the leg, ankle and foot. Among the main limitations, then, are arterial and venous vasculopathies. It is based on perforating branches of the fibular artery, whose origin is located between 5 and 6 cm above the lateral malleolus. The skin island is designed in the middle and proximal third of the leg. The arc of rotation must be calculated so as not to pull the pedicle. The donor area can be closed primarily or grafted3.
In a published series of 32 cases of reverse flow flaps, 14 of which were reverse sural flaps, the reliability and safety for covering various lesions in the distal third of the lower limbs were shown. These flaps were considered an alternative, even in complex lesions, to microsurgical flaps9.
The most common complications of the reverse sural flap are venous congestion and ischemia. Most flaps show some degree of congestion with improvement in a few days. However, necrosis (partial and complete) is the most relevant complication10. Follmar et al. reviewed 50 articles describing 720 flaps with a necrosis rate of 13.9%11. Skin islands marked cranial to the bifurcation of the gastrocnemius muscle showed higher rates of partial necrosis. The pivot point of the flap varies from 5 to 8 cm from the lateral malleolus. Changing this point can influence the occurrence of necrosis, although there is no study with statistical significance.
Finally, the width of the skin island greater than 8 cm can also influence the incidence of necrosis10.
Vendramin12 presented an experience of 61 cases accumulated over 10 years, suggesting that, after a learning curve and technical improvement, the results tend to present better rates and lower rates of complications.
Due to the electrical trauma associated with the flap’s dimensions, the patient evolved with distal necrosis, requiring an additional surgical procedure for debridement and re-advancement of the flap. Despite this, he presented wound resolution with adequate healing and satisfactory evolution.
CONCLUSION
The reverse sural flap proved to be a suitable alternative for treating extensive lesions with exposure of noble structures in the distal region of the foot after high-voltage electrical trauma, offering stable coverage with excellent contour, thus allowing satisfactory patient rehabilitation.
REFERENCES
1. Waldmann V, Narayanan K, Combes N, Marijon E. Electrical injury. BMJ. 2017;357:j1418. DOI: 10.1136/bmj.j1418. DOI: https://doi.org/10.1136/bmj.j1418
2. Luz DP, Millan LS, Alessi MS, Uguetto WF, Paggiaro A, Gomez DS, et al. Electrical burns: a retrospective analysis across a 5-year period. Burns. 2009;35(7):1015-9. DOI: https://doi.org/10.1016/j.burns.2009.01.014
3. Carvalho CM, Ferrari Neto O, Faria GEL, Milcheski DA, Gomez DS, Ferreira MC. Uso de retalhos em queimaduras elétricas nos últimos 10 anos. Rev Bras Queimaduras. 2013;12(1):2-5.
4. Daar DA, Abdou SA, David JA, Kirby DJ, Wilson SC, Saadeh PB. Revisiting the Reverse Sural Artery Flap in Distal Lower Extremity Reconstruction: A Systematic Review and Risk Analysis. Ann Plast Surg. 2020;84(4):463-70. PMID: 31688112 DOI: https://doi.org/10.1097/SAP.0000000000002041
5. Basile A, Stopponi M, Loreti A, Minniti de Simeonibus AU. Heel coverage using a distally based sural artery fasciocutaneous crossleg flap: report of a small series. J Foot Ankle Surg. 2008;47(2):112-7. DOI: https://doi.org/10.1053/j.jfas.2007.12.005
6. Li Y, Xu J, Zhang XZ. Lowering the pivot point of sural neurofasciocutaneous flaps to reconstruct deep electrical burn wounds in the distal foot. Burns. 2013;39(4):808-13. PMID: 22995425 DOI: https://doi.org/10.1016/j.burns.2012.08.014
7. Gumener R, Zbrodowski A, Montandon D. The reversed fasciosubcutaneous flap in the leg. Plast Reconstr Surg. 1991;88(6):1034-41. DOI: https://doi.org/10.1097/00006534-199112000-00013
8. Milcheski DA, Busnardo F, Ferreira MC. Reconstrução microcirúrgica em queimaduras. Rev Bras Queimaduras. 2010;9(3):100-4.
9. Marcondes CA, Pessoa SGP, Pessoa BBGP, Hartmann AA. Complex reconstruction of the upper and lower limbs by using reverse-flow flaps: a series of 32 cases. Rev Bras Cir Plást. 2015;30(4):622-5.
10. Wei JW, Dong ZG, Ni JD, Liu LH, Luo SH, Luo ZB, et al. Influence of flap factors on partial necrosis of reverse sural artery flap: a study of 179 consecutive flaps. J Trauma Acute Care Surg. 2012;72(3):744-50. PMID: 22491564 DOI: https://doi.org/10.1097/TA.0b013e31822a2f2b
11. Follmar KE, Baccarani A, Baumeister SP, Levin LS, Erdmann D. The distally based sural flap. Plast Reconstr Surg. 2007;119(6):138e-48e. DOI: https://doi.org/10.1097/01.prs.0000259203.79909.7e
12. Vendramin FS. Reverse-flow sural flap: 10 years of clinical experience and modifications. Rev Bras Cir Plást. 2012;27(2):30915. DOI: https://doi.org/10.1590/S1983-51752012000200023
1. Universidade de São Paulo, Hospital das Clínicas, Faculdade de Medicina, São Paulo,
SP, Brazil
Institution: Universidade de São Paulo, Hospital das Clínicas, Faculdade de Medicina, São Paulo, SP, Brazil.
GMC Analysis and/or interpretation of data, Data Collection, Conceptualization, Conception and design of the study, Methodology, Writing - Preparation of the original, Writing - Review and Editing.
RDAR Analysis and/or interpretation of data, Data Collection, Writing - Preparation of the original, Writing - Review and Editing.
DNB Analysis and/or interpretation of data, Data Collection, Writing - Preparation of the original, Writing - Review and Editing.
CEVG Conceptualization, Conception and design of the study, Carrying out operations and/or experiments.
DAM Final approval of the manuscript, Conceptualization, Conception and design of the study, Project Management, Carrying out operations and/or experiments, Writing - Review and Editing, Supervision.
Corresponding author: Gustavo Moreira Clivatti Avenida Dr. Enéas de Carvalho Aguiar, 255, serviço de Cirurgia Plástica, 8º andar, São Paulo, SP, Brazil Zip Code: 05403-900, E-mail: clivatti@gmail.com
Article received: April 14, 2021.
Article accepted: July 12, 2021.
Conflicts of interest: none.












 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter