

Ideas and Innovation - Year 2020 - Volume 35 -
Upper Pedicle Breast Flap
Retalho mamário de pedículo superior
ABSTRACT
Introduction: Here we propose a tactic to fill the upper poles of breasts that are emptied by ptosis in primary and secondary cases to obtain anatomically beautiful breasts with sufficient breast volume.
Objective: To describe breast tissue flaps used to fill the upper breast pole when there is adequate or surplus volume.
Methods: In primary or secondary cases, if the measurement from point A to the submammary fold is long and that to the upper glandular ridge is short, one obtains from the difference between them a flap with na upper pedicle, termed a “book leaf,” and sutured at the upper mammary pole. Glandular detachment preserves the skin’s thickness with subcutaneous tissue in all maneuvers similar to the adjacent thorax according to the mammary gland’s vascular anatomy, which is irrigated and innervated from the subcutaneous tissue to the gland.
Results: The six patients presented no complications related to flap irrigation. Adequate mammary shape and volume were achieved by inverting measurements between the lower and upper poles.
Discussion: Here we proposed an innovative manner to fill the upper pole of the breast with a breast upper pedicle flap. A larger number of cases should be analyzed in the long term.
Conclusion: The flap is used to fill the upper pole of the breast when the largest volume is in the lower pole.
Keywords: Mammoplasty; Breast; Surgical flaps; Tissue and organ acquisition; Biological tissue flaps.
RESUMO
Introdução: É proposto uma tática para preenchimento do polo superior das mamas que se esvaziam pelo processo de ptose em casos primários e secundários, permitindo assim obtenção de mamas anatomicamente bonitas, em casos de volume mamário suficiente.
Objetivo: Descrever retalho de tecido mamário com a finalidade de preenchimento do polo mamário superior, quando exista volume adequado ou excedente.
Métodos: Em mamas primárias ou secundárias, se a medida do ponto A até o sulco submamário é longa e deste até o rebordo glandular superior é curta, obtêm-se da diferença entre elas um retalho com pedículo superior, revirado em "folha de livro" e suturado no polo mamário superior. Descolamentos glandulares preservando a espessura de pele com tecido subcutâneo em todas as manobras igualmente à do tórax adjacente. Baseando-se na anatomia vascular da glândula mamária que é irrigada e inervada desde à superfície subcutânea para dentro da glândula.
Resultados: As seis pacientes não apresentaram complicação na irrigação do retalho. A forma e volume mamários adequados foram alcançados através da inversão de medidas entre polo inferior e superior.
Discussão: Propõe-se uma ideia e inovação, de preenchimento o polo superior das mamas com tecidos próprios, através de retalho de pedículo superior mamário. Deve ser analisado a longo prazo um maior número de casos para análise dos resultados obtidos.
Conclusão: O retalho se presta ao preenchimento do polo superior da mama quando o maior volume está no polo inferior.
Palavras-chave: Mamoplastia; Mama; Retalhos cirúrgicos; Obtenção de tecidos e órgãos; Retalhos de tecido biológico
INTRODUCTION
During the aging process and consequent breast ptosis, emptying of the upper pole occurs. The breast loses its anatomically beautiful shape and its base becomes transversal, inverting its diameters1. The more the horizontal direction is elongated, the greater the ptosis. In the frontal view, the vertical diameter of the breast should be aesthetically perfect and longer than the horizontal in the proportion of 1.3:1. This is a frequent complaint in the postoperative period because the possible flaps for upper pole projection and elongation of the vertical diameter and horizontal reduction do not offer full filling in all cases because they do not reach the highest horizontal breast line (HHBL), the connection between the two anterior axillary folds1.
Breast tissue flaps are used for this purpose. The most commonly used is the lower pedicle axial flap described by Ribeiro et al. in 20022 in its various forms2,3. However, in some cases, it does not reach the upper pole when the measurement between the submammary groove (at the vascular pedicle) and the areola is insufficient for its end under the breast to reach the HHBL1. This excellent flap fills the upper and lower poles, not changing the proportion between them. Crossed flaps of the medial and lateral sides of the breast would have the same purpose: one would fill the upper breast pole and the other assuming the position of the first4,5,6.
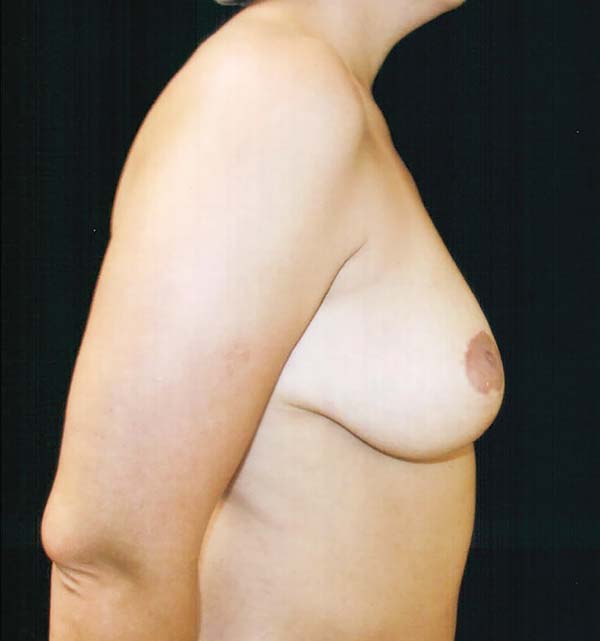
In the breast ptosis process, on breast profiles (Figure 1), the measurement between the cone’s apex and the groove expands, while that between the apex and the upper pole ridge shortens. The ratio of the proportion between the lower and upper measurement that should be from 1:1.6 to 1:1.41; as it approaches 1, the breast becomes more flaccid. It also occurs in postoperative techniques that do not model and structure the cone’s breast as a fundamental principle with appropriate proportions and measures and use the skin’s traction and resistance to provide shape. In the medium term, the breast acquires the shape left by the surgeon and the flap distends the skin, acting as an expander. This elongates the vertical scar even if it is initially short and under tension. The proportion between the upper and lower poles is inverted and the breast loses its original shape in the early postoperative period.
In cases of secondary mammoplasty, where there is enough volume to recreate the proper shape and the proportion between the lower and upper segments is inverted, the proposed tactic will be indicated. This is also true in primary breasts with the same inversion, which is sometimes called pseudoptosis7.
METHODS
There is a fundamental principle governing the flap’s vascular anatomy. The breasts are considered deeply modified sweat glands that are fundamentally ectodermic, that is, fixed to the skin.
At birth, the mammary glands show the same development in both sexes. In females at puberty or during pregnancy and breastfeeding, they change under hormonal influence.
During female puberty, breast buds develop and distend the skin and subcutaneous tissue, decreasing their thickness from the peripheral adjacent thorax to the gland to the areola. It is in this tissue that blood vessels, lymphatic vessels, and nerves run in a converging network up to the nipple–areola complex (NAC). Degree of breast growth depends on both hormone dosage and number of buds.
Breast shape depends on the skin’s distensibility. The more resistant the skin, the less projected the breast will be with a wider base. The thinner the skin, the narrower the base. Therefore, the base’s extension and breast cone’s projection can be classified into 4 groups of hypertrophies and 4 groups of hypomastia8,9.
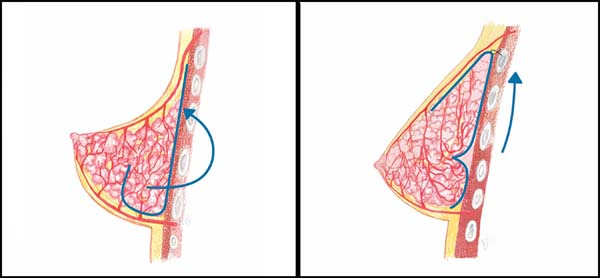
The upper vascularization originates from the perforators of the internal thoracic artery, with its branches of the second and third more calibrous veins. They irrigate the upper internal portion from the subcutaneous tissue inward toward the mammary tissue. In the upper lateral portion, the mammary branches penetrating the gland from the subcutaneous tissue originate from the lateral thoracic artery, an axillary branch. In the upper pole, irrigation comes from the pectoral branches of the thoracoacromial artery, penetrating the gland in the same way as the others through the subcutaneous tissue (Figures 2A, 2B, and 2C)10.

The thickness of the subcutaneous tissue in the thorax changes only with changes in body weight. It serves as a guide for obtaining flaps or detaching glands without damaging the arterial irrigation, venous drainage, lymphatic system, or innervation.
Surgery
Excess skin markings for resection to correct ptosis should be performed according to the surgeon’s experience. This can appear as an inverted T, L, or vertical line depending on the degree of ptosis.
In the breast meridian, the measurement between point A and the upper glandular ridge is equal to or less than that from point A to the submammary groove. In primary or secondary cases, with sufficient volume, the proposed tactic is indicated except in secondary cases in which the primary surgery was performed by techniques that detached the skin from the gland.
The excess skin is de-epidermized from the demarcated area to the submammary groove. Both periareolar and subareolar, this lower region can be removed.
Using Kocher forceps, point A is pulled perpendicular to the thorax until the gland is cone-shaped (Figure 3A).
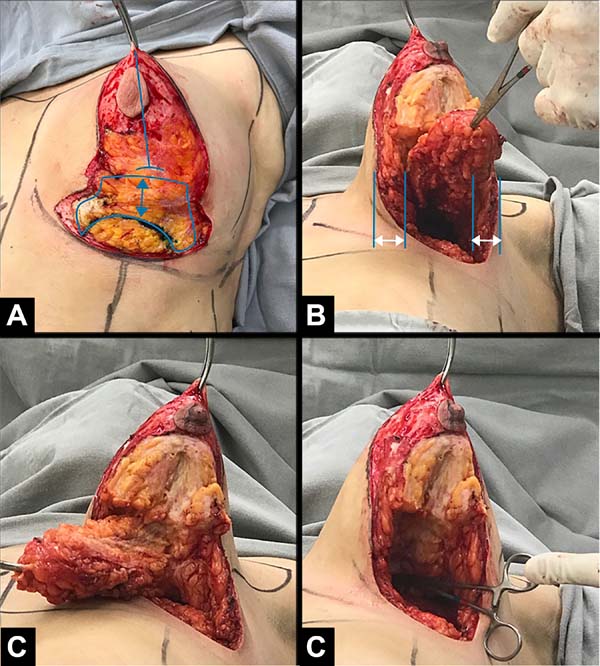
In the mammary meridian, at point A, the lower measurement is marked for the desired side (6–8 cm) toward the submammary groove. It is from this point to the groove that the possible flap thickness is obtained (it can be reduced if necessary). This represents how much it is possible to increase the upper pole by reducing the lower pole. Mathematically, the proportions can be inverted by transporting tissue from the lower pole to the upper pole and the proportion between 1:1.4 to 1:1.6 can be offered between the lower and upper measurements based on the A point of the future papilla.
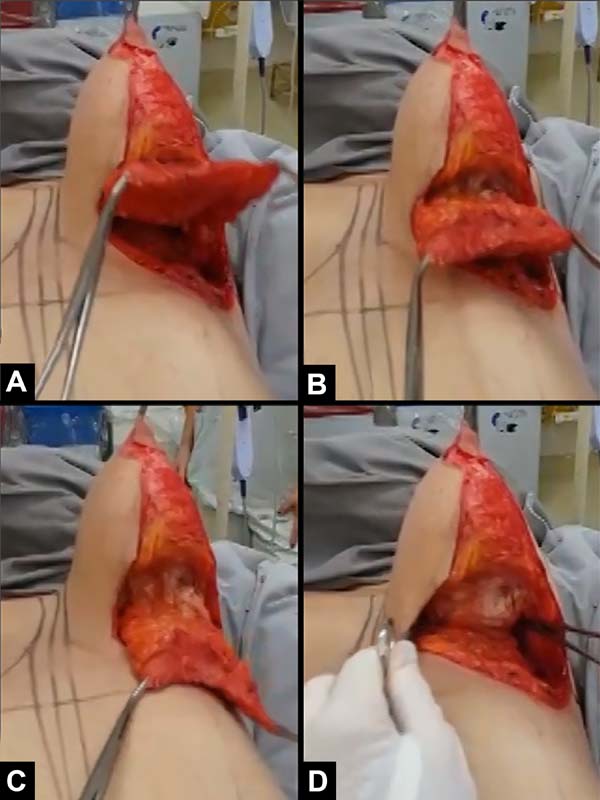
The breast should be detached from the pectoral muscles. The medial and lateral thickness of the peripheral subcutaneous tissue should be preserved without detachment, avoiding lesions to the vessels that irrigate it. In the upper pole, it detaches until it reaches the upper horizontal breast line without reaching the upper nutrient vessels present in the subcutaneous tissue. In the lower pole, at the meridian, a mini lower pedicle described by Ribeiro et al. in 20022 is left to recompose it (Figure 3A). The mammary tissue is detached from the flap at the lateral and medial sides, in the skin and subcutaneous tissue, again preserving the thickness equal to the adjacent thorax (Figure 3B).
The gland is transversally incised where the flap thickness was marked, directing it to the upper pole until just above the transversal diameter of the breast cone base (Figure 3C).
This glandular flap is obtained in a slightly cylindrical way; if reduced in its lateral and medial ridges (Figures 3B, 3C), it resembles a half moon (Figures 4A, 4B). It is turned into what is termed a “book leaf,” with the transversal axis of the pedicle above half of the breast base. It is introduced through the upper detached area reaching the HHBL1 (Figures 3D, 4C, and 4D), where its end is fixed. It redoes the upper breast pole, filling it, reducing the lower one and inverting the measurements between the two segments (Figures 5A and 5B). If there is a need to reduce the lateral diameter of the mammary cone, a vertical wedge can be made in the remaining mammary tissue of the lower pole up to before the flap pedicle (Figures 3C, 3D).
If further volume reductions are required, part of the flaps or tissue of the bottom base will be resected. In all tactical maneuvers, the thickness of the subcutaneous should be preserved equal to that of the thorax except in the upper pole where the flap will be implanted.
RESULTS
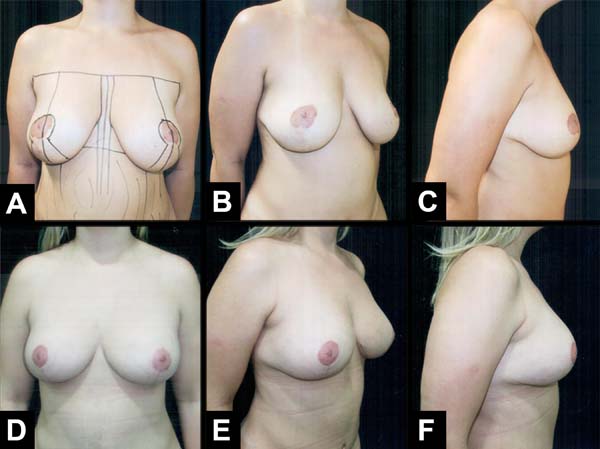
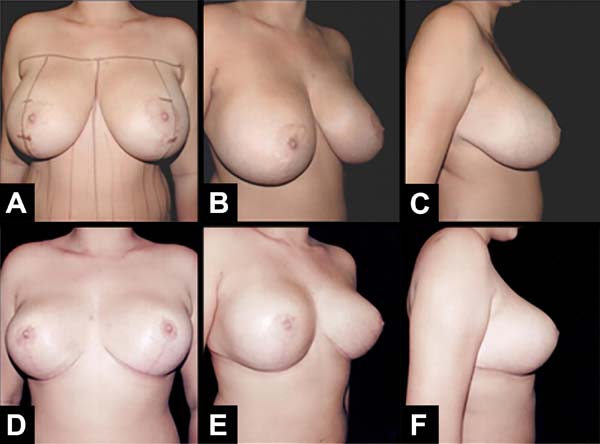
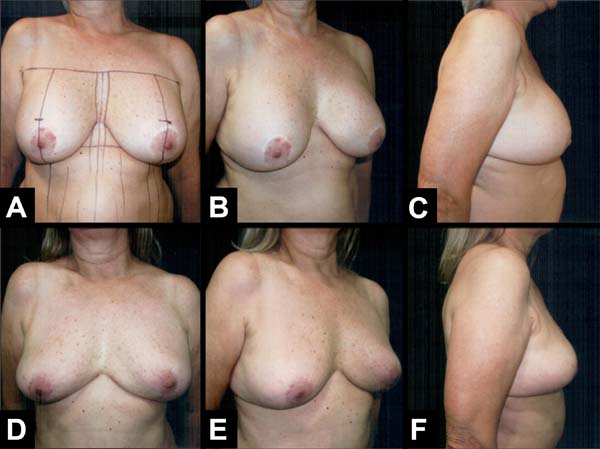
The authors operated on six patients at the Base Hospital of the Medical School of São José do Rio Preto. All patients signed an informed consent form prior to participating. The results showed that the upper pole was filled through inversion of the lower and upper pole measurements as well as adequate projection (Figures 6A–6F) and (Figures 7A–7F), and the consequent breast shape improvement. There were no complications related to breast tissue vascularization. This remained natural on palpation without hardening or clinical signs of steatonecrosis. In one case, the implants were removed, the fibrous capsule was recent with no signs of a calcium deposit; its anterior portion was fixed to the flap, facilitating its suture to the upper pole (Figures 8A–8F). Additional cases are needed to analyze the long-term results of the mammary forms obtained as well as possible complications since this is an innovative rather than technical surgical tactic of mammoplasty.
DISCUSSION
Using our knowledge of ectodermic embryology and breast anatomy, we can make any flap with or without the NAC if the thickness of the subcutaneous is preserved progressively thinner as it approaches it. Glandular flaps can also be created if their pedicles are based on the subcutaneous tissue and skin. They can be axial if they follow the vascular path and are randomized or mixed (flap of Ribeiro et al. in 20022). If randomized, the appropriate proportions between their widths and lengths are maintained around 1:1.
The mammary gland embryologically originates from the ectoderm, so it is fixed to the skin that covers it. The preservation of the peripheral subcutaneous tissue equal to the thickness of the subcutaneous thorax is fundamental to preserving the vessels and nerves that converge in a network to the NAC because they irrigate and enervate the mammary tissue and the remaining skin surface.
The length of the proposed flap does not exceed its width, so its irrigation is satisfactory, running from top to bottom and from the surface to its depth. Its blood supply is derived from the branches of the pectoral artery of the thoracoacromial artery and the perforating vessels of the internal thoracic artery, the second and third intercostal spaces, and the branches of the thoracic-lateral artery, as long as the subcutaneous of the thorax peripheral to the gland is preserved, without detachments, except the upper area where the flap will be introduced.
When the breast tissue includes more adipose than glandular tissue, the flap should be shorter with a thick pedicle. This is generally enough to fill the upper mammary pole. If less consistent, it is more difficult to attach it to the appropriate place and may lead to low-quality results.
There were no major complications denoting a lack of adequate irrigation of the proposed flap.
In the frontal view, if the areolas are positioned close to the ideal measurements from the sternal furcula, thus appear too high, the proposed procedure corrects the visual distortion of the inverted proportions between the upper and lower breast poles. This tactic was developed by observing the breasts’ vascular behavior during skin-preserving mastectomies and by making flaps with or without NAC transport performed for over 45 years by the authors.
CONCLUSION
The described flap is proposed to fill the upper breast pole and invert the measures and proportions between the upper and lower breast segments in primary or secondary cases, promoting improved breast esthetics.
REFERENCES
1. Bozola AR, Longato FM, Bozola AP. Análise geométrica da forma da beleza da mama e da forma de prótese baseado na proporção Phi: aplicação prática. Rev Bras Cir Plást. 2011;26(1):94-103.
2. Ribeiro L, Accorsi Junior A, Buss A, Marcal-Pessoa M. Creation and evolution of 30 years of the inferior pedicle in reduction mammaplasties. Plast Recontr Surg. 2002;110(3):960-70.
3. Bozola AR. Mamaplastia - Técnica de Ari “Invertida”- Nota Prévia. In: Anais da I Jornada Sulbrasileira de Cirurgia Plástica. 1984. p. 157-160.
4. Sperli AE. Reduction mammaplasty under cross-flap. In: I Congress of the International Aesthetic Plastic Surgery; 1972 feb 6-11; Rio de Janeiro (RJ): ISAPS; 1972.
5. Hakme F, Gomes Filho BS, Muller PM, Sjostedt C. Técnica em “L” nas ptoses mamarias com confecção de retalhos cruzados. Rev Bras Cir Plást. 1983;73(2):87-91.
6. Fischer R, Sperli AS. Mastoplastia pela técnica dos retalhos cruzados: reavaliação de técnica. Rev Bras Cir Plást. 2008;23(3):173-8.
7. Regnault P. Reduction mammaplasty by “B” technique. Plast Reconst Surg. 1974;53(1):19-24.
8. Bozola AR. Breast reduction with short L scar. Plast Reconst Surg. 1990;85(5):728-38.
9. Bozola AR. Reduction mammaplasty: preferred techniques. In: Goldwyn RM, editor. Reduction mammaplasty. Boston: Litlle Brown & Co.; 1990. p. 407-37.
10. Grotting JC, De La Torre JI, Davis MR. Anatomia em cirurgia plástica – Vol. 5: Mama. In: Neligan PC, editor. Cirurgia plástica. 3ª ed. Rio de Janeiro: Elsevier; 2015. p. 6-8.
1. Faculdade de Medicina de São José do Rio Preto, São José do Rio Preto, SP, Brazil.
Corresponding author: Antonio Roberto Bozola Avenida José Munia 7075, São José do Rio Preto, SP, Brazil. Zip Code: 15085-350. E-mail: ceplastica@hospitaldebase.com.br
Article received: June 21, 2018.
Article accepted: October 21, 2019.
Conflicts of interest: none.











 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter