INTRODUCTION
Liposuction is among the most commonly performed aesthetic procedures in Brazil and
worldwide1,2. Since its inception, several technical improvements have been made; curettage, designated
lipexeresis, preceded contemporary fat removal techniques (Schrudde, 1972)3,4. Illouz (1980)5 described another technique involving the use of large-bore blunt cannulae to remove
subcutaneous fat, leaving 1-2 cm of subcutaneous cellular tissue to prevent the formation
of irregularities5.
Superficial liposuction, one of the most significant advancements in traditional suction-assisted
lipoplasty, improves skin retraction and was described by Gasperoni6-9, Gasparotti10-12, and De Souza Pinto13-15. However, this advancement increased the risk of abdominal deformities and irregularities
in the abdominal musculature and the production of cutis marmorata when excessive
fat was removed.
Liposuction can be performed in isolation or in association with abdominal skin resection.
In 1985, Hakme16 introduced the technique of miniabdominoplasty with liposuction, which included elliptical
resection of the suprapubic skin in selected cases. Saldanha popularized liposuction
associated with abdominoplasty with preservation of the Scarpa fascia without undermining
the abdominal flap17. This technique was safe, corrected aesthetic and functional deformities of the abdomen,
and produced a better and more harmonious contour of the abdominal musculature. Bozola
and Psillakis (1988)18 proposed a new concept of abdominal contouring and a classification based on the
deformities of each layer of the abdominal wall and their differentiated treatment
in patients eligible for abdominoplasty. The authors noted that a perfect and attractive
abdomen is not flat but had relief resembling an English lyre18. Nahas (2001) described a classification for abdominoplasty based on excess skin
and subcutaneous deformities19 and another classification based on myoaponeurotic deformities20.
Traditional liposuction failed to give the abdomen a defined contour and produced
a flat appearance. Mentz et al. (1993)21 was the first to describe high definition liposculpture, in which selective superficial
liposuction was performed to sculpt the abdomens of athletic men. A new concept of
liposculpture was created using these principles that allowed surgeons to sculpt the
body and enhance the abdominal musculature. Ersek and Salisbury (1997)22 performed superficial liposuction for abdominal etching in 25 athletic men using
a customized cannula.
Hoyos (2003)23 improved Mentz’s concepts to a three-dimensional approach involving other muscle
groups (trunk, legs, and back) and defined different aesthetic results to be achieved
between men and women. Hoyos et al. (2007)24 introduced the combination of vibration amplification of sound energy at resonance
(VASER), also known as ultrasonic liposuction, with high definition liposculpture24, miniabdominoplasty25, and liposuction + abdominoplasty26.
Danilla (2017)27 described the rectus abdominis fat transfer (RAFT) technique to improve abdominal
contouring using liposuction + abdominoplasty, while Motta (2018)28 introduced the technique of diode lasering combined with high definition liposculpture.
OBJECTIVE
To evaluate the aesthetic results of abdominal etching using liposuction.
METHODS
Patient selection
All consecutive patients who underwent abdominal liposuction performed by the lead
author between November 2017 and November 2018 were selected. All patients were healthy
women who were evaluated preoperatively. Patients with extensive abdominal scars and
deformities due to previous liposculpture were excluded from the study.
All patients provided written informed consent, including authorization for disclosing
images for academic purposes. The study complied with the guidelines of the Declaration
of Helsinki and was approved by the Medical Ethics Committee of the Unimed General
Hospital of Santa Maria, Rio Grande do Sul, Brazil (protocol no. 0012019).
Surgical procedure
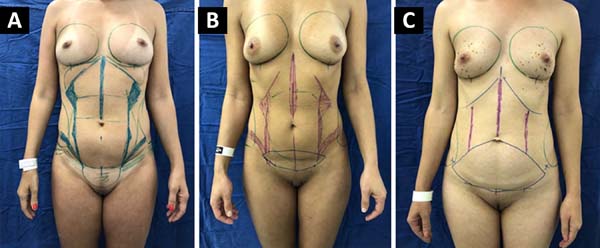
Surgical demarcation was performed with the patient in the standing position. Maneuvers
to facilitate palpation of the abdominal and subcostal muscles were performed to identify
areas requiring improvement (linea alba, linea semilunaris, subcostal muscles, Spigelian
fascia, and oblique muscles) (Figure 1). Matarasso’s classification29 was used to evaluate the type of surgery to be performed.
Figure 1. - Surgical demarcation. A: Liposuction; B: Liposuction + miniabdominoplasty; C: Liposuction + abdominoplasty
Figure 1. - Surgical demarcation. A: Liposuction; B: Liposuction + miniabdominoplasty; C: Liposuction + abdominoplasty
All procedures were performed under general anesthesia. A thermal blanket and pneumatic
compression boot were routinely used. Antimicrobial prophylaxis with 2 g of cefazolin
was administered at the time of anesthetic induction.
When liposuction of the dorsal region was indicated, the procedure was started with
the patient in prone position. After this stage was completed, the patient was placed
in the supine position for finishing the liposuction and performing other surgeries
when necessary. The super-wet technique was used with the infiltration of adrenaline
in saline (1:1000).
After a mean 15 min, liposuction using a straight 3.5-mm Mercedes cannula connected
to a vacuum (MEDAP-BORA UP 2080; Germany) at a constant pressure of 80 cmHg was performed.
Deep liposuction was initially performed in the demarcated areas. When abdominoplasty,
reverse abdominoplasty, or miniabdominoplasty was indicated, the skin was removed
following the surgical markings and the rectus abdominis muscles were plicated when
necessary. Next, liposuction was performed in the demarcated areas to define the shape
of the abdominal musculature. Only superficial liposuction was performed in cases
in which deep liposuction was not indicated.
In the anterior region, the cannula was inserted through one port each in the inguinal
region, inframammary fold, and umbilicus. In the dorsal region, the cannula was inserted
through one port in the intergluteal cleft and two sites lateral to it, following
the contour of the gluteus maximus. Two additional ports located in bilateral paravertebral
muscles were used to complement the treatment of the lower back, while two ports located
near the scapular region were used treatment in the upper back was necessary.
Prolonged drainage was required in the intergluteal region when liposuction from the
dorsal area was extensive or considerable bleeding occurred in this region during
the procedure. Drainage was required in the ventral region only in cases involving
abdominoplasty. At the end of the procedure, compression bandaging was used in the
operated areas in all patients.
The patients received antibiotic prophylaxis of 500 mg of cefadroxil for 7 days and
chemoprophylaxis of 40 mg of enoxaparin for 7-14 days starting the morning after surgery.
The mean length of hospital stay for patients undergoing abdominoplasty was 1 day.
Patients who underwent liposuction, even when associated with other procedures, were
discharged on the day of surgery. The first follow-up visit was on mean day 7 after
surgery. Subsequent visits were made at 14 days, 30 days, 3 months, 6 months, and
1 year after surgery. Photographs were acquired in the anterior, lateral, oblique,
and posterior views with the patient standing since the first follow-up consultation.
The patients were evaluated by the author for the extent of improvement in body image
and surgical complications. The extent of improvement was classified as follows: grade
0, no improvement; grade 1, presence of midline or linea semilunaris, or very faint
midline and linea semilunaris; grade 2, well-defined midline and linea semilunaris;
and grade 3, significant improvement.
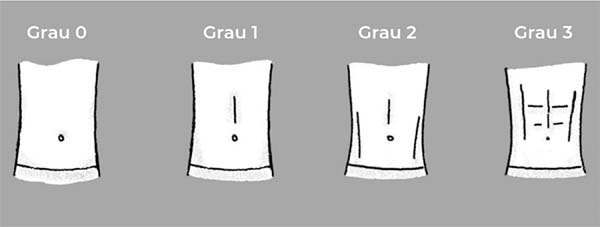
The patients assessed the extent of improvement, overall level of satisfaction, naturalness
of the result, and lifestyle changes (exercise and diet) using a standard questionnaire.
The extent of improvement was assessed by the patient, who chose one of the schematic
drawings that reflected the postoperative abdominal contour (Figure 2).
Figure 2. - Schematic drawing of abdominal shape according to patient assessment.
Figure 2. - Schematic drawing of abdominal shape according to patient assessment.
RESULTS
Eighty female patients were included in this study. The average age was 38.96 (range,
26-63) years, while the average body mass index was 24.01 (range, 18.32-30.97). In
addition, 73.75% of patients had previous pregnancies, while 25% had previous abdominal
surgeries (liposuction or abdominoplasty). Two (2.5%) patients had a history of smoking.
Simultaneous procedures were performed in 90% of the patients. The mean postoperative
follow-up period was 7.27 (range, 2-13) months. The following types of surgery were
performed: liposuction alone (40.00%), liposuction + abdominoplasty (36.25%), miniabdominoplasty
(12.5%), abdominoplasty + liposuction (10.00%), and reverse abdominoplasty (1.25%)
(Table 1).
Table 1 - Patient characteristics (N = 80)
| Variable |
Mean |
Variation |
Percentage |
| Age |
38,96 |
26-63 |
|
| Body mass index |
24,01 |
18,32-30,97 |
|
| Previous pregnancy |
59 |
|
73,75% |
| Previous abdominal surgery |
20 |
|
25% |
| Smoking (No) |
2 |
|
2,50% |
| Surgery |
80 |
|
100% |
| Liposuction |
32 |
|
40% |
| Abdominoplasty + liposuction |
8 |
|
10% |
| Liposuction + abdominoplasty |
29 |
|
36,25% |
| Miniabdominoplasty |
10 |
|
12,50% |
| Reverse abdominoplasty |
1 |
|
1,25% |
| Associated surgeries |
72 |
|
90% |
| Gluteal fat grafting |
50 |
|
62,50% |
| Mammoplasty |
34 |
|
42,50% |
| Other surgical procedures |
2 |
|
2,50% |
Table 1 - Patient characteristics (N = 80)
Most (86.25%) patients reported moderate (grade 2) improvement in abdominal shape
(well-defined midline and linea semilunaris). Five (6.25%) patients had no improvement,
while four (5%) and three (3.75%) patients classified the improvement as minor (grade
1) and significant (grade 3), respectively.
Typical complications occurred in four (5%) patients who underwent lipoabdominoplasty,
including keloid scars (two cases [2.5%]), seroma (one case [1.25%]), and minor abdominal
flap necrosis (one case [1.25%]). Surgical complications occurred in four (5%) patients,
including contour asymmetry in the semilunar lines (two cases [2.5%]) and abdominal
deformities (two cases [2.5%]) (Table 2).
Tabela 2 - Complicações.
| Complications |
N (%) |
| Typical |
| Keloid scar |
2 (2,5%) |
| Seroma |
1 (1,25%) |
| Abdominal flap necrosis |
1 (1,25%) |
| Directly related to surgical technique |
| Asymmetry of the linea semilunaris |
2 (2,5%) |
| Irregularities |
2 (2,5%) |
All patients answered the questionnaire via email or in person. Forty-nine patients
(61.25%) classified the improvement as grade 2. Two (2.5%) patients reported no improvement,
whereas seven (8.75%) and 22 (27.5%) patients rated the improvement as grades 1 and
3, respectively (Table 3).
Table 3 - Degree of abdominal etching*
| Examiner |
Grade 0 |
Grade 1 |
Grade 2 |
Grade 3 |
| Author |
6,25% |
5% |
82,25% |
3,75% |
| Patient |
2,50% |
8,75% |
61,25% |
27,50% |
Table 3 - Degree of abdominal etching*
Most patients were very satisfied (71.25%) with the outcome, 30% were satisfied, and
8.75% were reasonably satisfied. None of the study patients were dissatisfied with
the surgical results.
The result was classified as natural by 97.5% of the patients. All patients would
undergo the surgery again and would recommend it to another person. Among our sample,
63.5% of the patients increased their physical activity level, 81.25% improved their
dietary habits, and 55% lost weight (Figures 3-9).
Figure 3. - Preoperative aspect and postoperative (6 months) result of liposuction and correction
of postoperative deformities, resulting in significantly improved (grade 3) abdominal
contouring.
Figure 3. - Preoperative aspect and postoperative (6 months) result of liposuction and correction
of postoperative deformities, resulting in significantly improved (grade 3) abdominal
contouring.
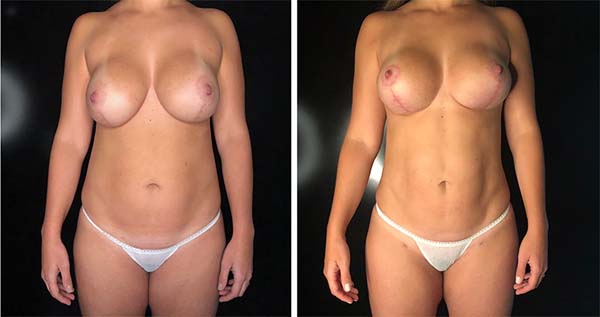
Figure 4. - Preoperative aspect and postoperative (6 months) result of liposuction + abdominoplasty,
with moderately improved (grade 2) abdominal shape.
Figure 4. - Preoperative aspect and postoperative (6 months) result of liposuction + abdominoplasty,
with moderately improved (grade 2) abdominal shape.
Figure 5. - Preoperative aspect and postoperative (6 months) result of liposuction + abdominoplasty,
with little improvement (grade 1) in body image
Figure 5. - Preoperative aspect and postoperative (6 months) result of liposuction + abdominoplasty,
with little improvement (grade 1) in body image
Figure 6. - Preoperative aspect and postoperative (12 months) result of liposuction, with significant
improvement (grade 3) in abdominal contouring.
Figure 6. - Preoperative aspect and postoperative (12 months) result of liposuction, with significant
improvement (grade 3) in abdominal contouring.
Figure 7. - Preoperative aspect and postoperative (3 months) result of liposuction, with moderately
improved (grade 2) body image.
Figure 7. - Preoperative aspect and postoperative (3 months) result of liposuction, with moderately
improved (grade 2) body image.
Figure 8. - Preoperative aspect and postoperative (3 months) outcome of miniabdominoplasty, with
intermediate improvement (grade 2) in abdominal shape.
Figure 8. - Preoperative aspect and postoperative (3 months) outcome of miniabdominoplasty, with
intermediate improvement (grade 2) in abdominal shape.
Figure 9. - Preoperative aspect and postoperative (3 months) result of liposuction with asymmetry
of the semilunar lines.
Figure 9. - Preoperative aspect and postoperative (3 months) result of liposuction with asymmetry
of the semilunar lines.
DISCUSSION
The ideal abdomen is not flat; rather, it is a combination of convex and concave shapes
that follow the deep bone and muscle anatomy30.
Superficial liposuction for abdominal etching is an evolution of traditional suction-assisted
lipoplasty. The removal of superficial fat is necessary to achieve the abdominal shape
of athletes. It consists of enhancing specific areas (alba line, linea semilunaris,
subcostal muscles, semilunar fascia, and oblique muscles) by removing fat from all
skin layers, including the superficial layer.
Abdominal etching in female patients involves improving the lateral margins and midline
of the rectus abdominis muscle but not of transverse tendinous intersections. Women
usually prefer partial to complete abdominal etching31.
In the present study, most patients reported intermediate improvement (grade 2) in
abdominal shape (well-defined midline and linea semilunaris). Little or no improvement
was observed in patients with excessive weight and residual abdominal flaccidity.
Almost one-third of the patients rated the improvement as grade 3 (significant), although
only 5% (three patients) received this grade by the surgeon. This result may be explained
by the subjectivity of the outcome and/or the fact that removal of the deep fat layer
above the rectus abdominis muscle combined with adequate eating habits and exercise
after surgery favors the appearance of transverse tendinous intersections, improving
body contour.
Abdominal etching may help improve patient lifestyles after surgery, including dietary
and exercise habits. The present results showed that most patients improved their
habits during the study period, particularly diet.
Almost all patients reported that the abdominal contour appeared natural after the
procedure, and the high satisfaction rate here (91.25%) agrees with the literature.
Hoyos and Millard (2007)24 reported an 84% satisfaction rate of the sample. Hoyos et al. (2018)26 showed a 91.79% satisfaction rate of procedures involving lipoabdominoplasty. Motta
(2018)28 observed that all study patients were satisfied with the surgical outcome.
Abdominal etching can be achieved using liposuction, VASER24-26, or lasering28 without the need for other techniques21,22,27. The most effective procedure is unknown because no studies have compared the outcomes
of abdominal etching. Mentz et al. (1993)21 used conventional liposuction in the 8 male patients in his study. Danilla (2017)27 found a high degree of abdominal definition in his 26 patients associating rectus
abdominis fat grafting with lipoabdominoplasty without the use of associated technologies.
The main complications related to superficial liposculpture are irregularities and
asymmetries, which impart an unnatural appearance to the abdomen. In our assessment,
4% of patients had irregularities and/or asymmetries due to excessive liposuction
from the deep layers and asymmetrical positioning and/or closer proximity of the linea
semilunaris. Hoyos et al. (2007)24 reported that 3.2% of patients had irregularities that required surgical revision.
Most patients presented fibrosis in the abdominal area subjected to superficial liposuction,
and the compromised areas healed spontaneously after 6 months or less. Danilla (2017)27 observed that these irregular fibrotic areas resolved spontaneously in 3-4 months
and healed completely in up to 8 months.
One of the limitations of this study was its short follow-up period. For this reason,
whether the lifestyle changes of these patients continued over time is unknown. In
addition, future studies are necessary to assess whether situations such as variability
in body weight and pregnancy created loss of naturalness of the result. The literature
on the subject is scarce21-28, and few studies have evaluated the results of abdominal etching with long-term follow-up.
CONCLUSION
Abdominal etching using liposuction was very satisfactory and gave a natural appearance
to the abdomen. This result can be achieved through conventional liposuction technique
without the need for additional technological devices.
COLLABORATIONS
|
MSSV
|
Analysis and/or data interpretation, Conception and design study, Conceptualization,
Data Curation, Final manuscript approval, Formal Analysis, Funding Acquisition, Investigation,
Methodology, Project Administration, Realization of operations and/or trials, Resources,
Software, Supervision, Validation, Visualization, Writing - Original Draft Preparation,
Writing - Review & Editing
|
REFERENCES
1. International Society of Aesthetic Plastic Surgery (ISAPS). ISAPS Global Statistics
[Internet]. 2019; [cited 2019 Jan 11]. Available from: https://www.isaps.org/medical-professionals/isaps-global-statistics/
2. Heidekrueger PI, Juran S, Patel A, Tanna N, Broer PN. Plastic surgery statistics in
the US: evidence and implications. Aesthetic Plast Surg. 2016 Apr;40(2):293-300. DOI:
https://doi.org/10.1007/s00266-016-0611-3
3. Schrudde J. Lipektomie und lipexhaerese im Bereich der unteren Extremitäten. Langenbecks
Archiv für Chirurgie. 1977 Dec;345(1):127-31. DOI: https://doi.org/10.1007/BF01305460
4. Schrudde J. Lipexeresis as a means of eliminating local adiposity. Aesthetic Plast
Surg. 1980 Dec;4(1):215-26. DOI: https://doi.org/10.1007/BF01575221
5. Illouz YG. Surgical remodeling of the silhouette by aspiration lipolysis or selective
lipectomy. Aesthetic Plast Surg. 1985;9(1):7-21. PMID: 2986432 DOI: https://doi.org/10.1007/BF01570678
6. Gasperoni C, Salgarello M. Suction-assisted lipectomy of the subdermal fat layer:
a new way of performing liposuction. Annals of the International Symposium Recent
Advances in Plastic Surgery. s.l, RAPS International Corporation [Internet]. 1990;
[cited 2019 Jan 11]. Available from: http://pesquisa.bvsalud.org/portal/resource/pt/lil-130513
DOI: https://doi.org/10.1007/BF01578339
7. Gasperoni C, Salgarello M, Emiliozzi P, Gargani G. Subdermal liposuction. Aesthetic
Plast Surg. 1990;14(2):137-42. PMID: 2333810
8. Gasperoni C, Salgarello M. Rationale of subdermal superficial liposuction related
to the anatomy of subcutaneous fat and the superficial fascial system. Aesthetic Plast
Surg. 1995 Jan/Feb;19(1):13-20. DOI: https://doi.org/10.1007/BF01578339
9. Gasperoni C, Salgarello M. MALL liposuction: the natural evolution of subdermal superficial
liposuction. Aesthetic Plast Surg. 1994 Jun;18(3):253-7. PMID: 7976757 DOI: https://doi.org/10.1007/BF00209305
10. Gasparotti M, Lewis CM, Toledo L. Superficial Liposculpture: manual of technique.
New York: Springer-Verlag New York; 1993.
11. Gasparotti M. Superficial liposuction: a new application of the technique for aged
and flaccid skin. Aesthetic Plast Surg. 1992;16(2):141-53. PMID: 1570777
12. Gasparotti M. Superficial liposuction for flaccid skin patients. In: Annals of the
International Symposium Recent Advances in Plastic. Surgery. 1990;90:441. DOI: https://doi.org/10.1007/BF00450606
13. De Souza Pinto EB, de Almeida AE, Knudsen AF, de Andrade SM, de Medeiros JC. A new
methodology in abdominal aesthetic surgery. Aesthetic Plast Surg. 1987;11(4):213-22.
PMID: 3445812
14. Souza Pinto EB, Indaburo PE, Muniz Ada C, Martinez YP, Gerent KM, Iwamoto H, et al.
Superficial liposuction. Body contouring. Clin Plast Surg. 1996 Oct;23(4):529-48;
discussion:49.
15. Souza Pinto EB. Superficial liposuction. Rio de Janeiro (RJ): Revinter; 1999.
16. Hakme F. Technical details in the lipoaspiration associate with liposuction. Rev Bras
Cir. 1985;75(5):331-7.
17. Saldanha OR, Souza Pinto EB, Mattos Júnior WN, Pazetti CE, Bello EML, Rojas Y, et
al. Lipoabdominoplasty with selective and safe undermining. Aesthetic Plast Surg.
2003 Jul/Aug;27(4):322-7. PMID: 15058559 DOI: https://doi.org/10.1007/s00266-003-3016-z
18. Bozola AR, Psillakis JM. Abdominoplasty: a new concept and classification for treatment.
Plast Reconstr Surg. 1988 Dec;82(6):983-93. PMID: 2974166 DOI: https://doi.org/10.1097/00006534-198812000-00008
19. Nahas FX. A pragmatic way to treat abdominal deformities based on skin and subcutaneous
excess. Aesthetic Plast Surg. 2001 Sep/Oct;25(5):365-71. DOI: https://doi.org/10.1007/s00266-001-0025-7
20. Nahas FX. An aesthetic classification of the abdomen based on the myoaponeurotic layer.
Plast Reconstr Surg. 2001 Nov;108(6):1787-95; discussion:96-7. DOI: https://doi.org/10.1097/00006534-200111000-00058
21. Mentz HA 3rd, Gilliland MD, Patronella CK. Abdominal etching: differential liposuction
to detail abdominal musculature. Aesthetic Plast Surg. 1993;17(4):287-90. DOI: https://doi.org/10.1007/BF00437100
22. Ersek RA, Salisbury AV. Abdominal etching. Aesthetic Plast Surg. 1997 Sep/Oct;21(5):328-31.
DOI: https://doi.org/10.1007/s002669900131
23. Hoyos AE. High Definition liposculpture. Bucaramanga, Colombia: XIII International
Course of Plastic Surgery; 2003.
24. Hoyos AE, Millard JA. VASER-assisted high-definition liposculpture. Aesthet Surg J.
2007 Nov/Dec;27(6):594-604. DOI: https://doi.org/10.1016/j.asj.2007.08.007
25. Hoyos AE, Perez ME, Castillo L. Dynamic definition mini-lipoabdominoplasty combining
multilayer liposculpture, fat grafting, and muscular plication. Aesthet Surg J. 2013
May;33(4):545-60. PMID: 23636628 DOI: https://doi.org/10.1177/1090820X13484493
26. Hoyos A, Perez ME, Guarin DE, Montenegro A. A report of 736 high-definition lipoabdominoplasties
performed in conjunction with circumferential VASER Liposuction. Plast Reconstr Surg.
2018 Sep;142(3):662-75. DOI: https://doi.org/10.1097/PRS.0000000000004705
27. Danilla S. Rectus Abdominis Fat Transfer (RAFT) in lipoabdominoplasty: a new technique
to achieve fitness body contour in patients that require tummy tuck. Aesthetic Plast
Surg. 2017 Dec;41(6):1389-99. DOI: https://doi.org/10.1007/s00266-017-0909-9
28. Motta RP. Lipoaspiração laser-assistida de alta definição. Rev Bras Cir Plást. 2018;33(1):48-55.
29. Matarasso A, Swift RW, Rankin M. Abdominoplasty and abdominal contour surgery: a national
plastic surgery survey. Plast Reconstr Surg. 2006 May;117(6):1797-808. PMID: 16651953
DOI: https://doi.org/10.1097/01.prs.0000209918.55752.f3
30. Avelar J. Regional distribution and behavior of the subcutaneous tissue concerning
selection and indication for liposuction. Aesthetic Plast Surg. 1989;13(3):155-65.
PMID: 2801296 DOI: https://doi.org/10.1007/BF01570212
31. Hoyos A, Prendergast PM. High Definition Body Sculpting: art and advanced lipoplasty
techniques. Berlin, Heidelberg: Springer-Verlag; 2014.
1. Sa.Vi Medicina, Santa Maria, RS, Brazil.
Corresponding author: Mauricio Schneider Salomone Viaro Avenida Presidente Vargas 2084, sala 1301, Santa Maria, RS, Brazil. Zip Code: 97015-512.
E-mail: msviaro@hotmail.com
Article received: January 22, 2019.
Article accepted: June 22, 2019.
Conflicts of interest: none.