Introduction
Highly effective procedures used for facial rejuvenation include injectable neurotoxins,
soft-tissue fillers, and chemical peels. Soft-tissue fillers have an impressive ability
to volumize and reshape aging, sagging skin with a small time commitment and minimal
side effects. A variety of filling agents have been approved by the United States
Food and Drug Administration (FDA) to correct moderate to severe facial wrinkles such
as hyaluronic acid, poly-l-lactic acid, calcium hydroxyapatite, and polymethylmethacrylate.
Although not FDA approved and forbidden in many countries for the treatment of facial
aesthetic contours, silicone is used “off-label” for cosmetic purposes for treating
acne scars or performing facial augmentation.
Reported complications after soft-tissue augmentation may be related to poor injection
technique or the filler material itself. Complications such as visible product, hypertrophic
scarring, nodule formation, and the Tyndall effect (bluish discoloration from hydroxyapatite
fillers) can occur if the soft-tissue synthetic materials are placed too superficially.
Persistent and painful erythematous nodules have been associated with every type of
injectable filler as granulomatous reactions. Their treatment ranges from antibiotics
to surgical removal.
Here we present the case of a patient who underwent static lip reanimation for facial
nerve damage following nodule removal as a filler complication.
Case report
A 50-year-old woman presented at our clinic with a lower lip deformity. She had a
history of facial rejuvenation using silicone to restore the volume of the nasolabial
folds and cheeks. Persistent erythematous nodules granulomatous reactions occurred
and were removed surgically.
On examination 2 years after primary surgery, she had a bilaterally elongated upper
lip, a right lower lip drop with evident lip dynamic distortion when she smiled, and
bilateral cheek deformity probably due to marginal mandibular nerve damage (Figure 1). Using a flexible ruler, the distances of the modiolus to the cupid’s and commissure
to the cupid’s bow were 4.5 and 3.5 cm on the paralyzed side and 4 and 3 cm on the
non-paralyzed side.
Figure 1 - Patient presented with a right lower lip drop and evident bilateral cheek deformity.
Figure 1 - Patient presented with a right lower lip drop and evident bilateral cheek deformity.
Preoperative markings in unilateral facial palsy are essential. With the patient seated
upright, the nasolabial fold and cheek deformities were marked. A “modified bull’s
horn approach” was taken to the upper lip lift1. The flap markings included the “bull’s horn” drawn around the nasal wings and columella
and its pedicle along the right nasolabial fold (Figure 2). A line was drawn from the columellar-labial fold and extended laterally around
the nasal wings to define the superior limit of the bull’s horn flap. Another line
was drawn parallel to the first one in a lower position to define the inferior border
of the flap, meeting the upper one at the lateral edges. Under local anesthesia and
sedation, the flap was de-epithelized, and a dermoadiposal flap was harvested from
the lateral left margin to the lateral right margin, and its pedicle was left attached
to the upper ptotic right lip. Using the open tip of a small liposuction cannula,
the flap was tunneled and fixed directly in a C-loop fashion using U stitches, and
the flap was transfixed to the periosteum of the zygomatic arch. The traction tension
of the flap was adjusted to balance the paralyzed and nonparalyzed sides of the upper
and lower lips. During surgery, a first fat-graft injection was also made to correct
cheek contour deformity, while a second fat-graft session was planned 3 months later
to improve the aesthetic results (Figure 3).
Figure 2 - Preoperative markings. With the patient seated upright the nasolabial folds and cheeks
deformity were marked. A "modified bull's horn" upper lip lift markings were carried
out around the nasal wings and columella and along the right nasolabial fold.
Figure 2 - Preoperative markings. With the patient seated upright the nasolabial folds and cheeks
deformity were marked. A "modified bull's horn" upper lip lift markings were carried
out around the nasal wings and columella and along the right nasolabial fold.
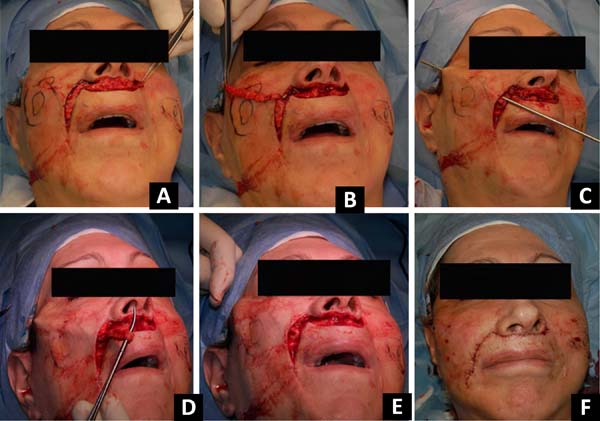
Figure 3 - Intraoperative view. The flap was deepithelized (A) and a dermoadiposal flap was harvested (B). By the use of the open tip of a small liposuction cannula, the distal portion of
the flap was tunneled and fixed in a C-loop fashion (C,D). The traction tension of the flap was adjusted to balance the length of the paralyzed
and nonparalyzed segments of the upper and lower lips (E,F).
Figure 3 - Intraoperative view. The flap was deepithelized (A) and a dermoadiposal flap was harvested (B). By the use of the open tip of a small liposuction cannula, the distal portion of
the flap was tunneled and fixed in a C-loop fashion (C,D). The traction tension of the flap was adjusted to balance the length of the paralyzed
and nonparalyzed segments of the upper and lower lips (E,F).
Fat tissue was harvested using dry technique with a 3-mm multi-hole barbed cannula
and a 10-mL syringe under manually generated negative pressure. The fat was centrifuged
at 1000 rpm for 3 minutes and finally injected with a 19G needle. The high-density
fraction of the concentrated adipose tissue was used to restore the cheek deformities,
while the low-density fraction was used for aesthetic refinements of the face2.
No significant complications were observed, and the patient reported no functional
limitations or dissatisfaction with the aspect of the scars in the nasolabial fold
or around the nasal wings and columella. The upper and lower lips appeared to be well
positioned with a slight deviation of the cupid’s bow toward the reconstructed side
because of the overcorrection. An adequately shaped, intense smile was observed despite
some incoordination with the non-paralyzed side. Postoperatively, the distances of
the modiolus to the cupid’s bow and commissure to the cupid’s bow were 4 and 3 cm,
respectively, on both sides. Balance and adequate positioning of philtrum on the median
line were evaluated, dividing the distance from the paralyzed side with the sum of
the measurements of the paralyzed and non-paralyzed sides. The pre- and postoperative
values of 53.3% and 50%, respectively, for the modiolus and commissure distances suggested
a static good outcome. The results at 3 years of follow-up are shown in Figure 4.
Figure 4 - Results at three-year of follow-up.
Figure 4 - Results at three-year of follow-up.
Discussion
Facial paralysis is a profoundly disfiguring condition with significant psychological
and functional consequences. Prior to the introduction of surgical reanimation, treatment
was based on medical therapies (botulinum toxin injection) and prostheses3. Over time, static surgical procedures were introduced; thereafter, the use of temporalis
and masseteric muscle transfers became popular.
Recently, nerve grafts and free muscle flap transfers have been considered by many
surgeons the ideal procedures for long-standing facial paralysis to restore symmetry
at rest and during smiling. However, facial movements are generally unidirectional
and localized and cannot precisely reproduce the function of multiple muscles responsible
for oral expressions4,5.
Differences in patients, facial perceptions, and various treatment strategies preclude
a direct comparison of reconstructive techniques.
Tissue transfer is correlated to major trauma and donor site morbidity; it can require
a two-stage operation, prolonged re-innervation time, and multiple revision procedures
over time6. Even if it is performed at specialized centers, a patient’s baseline health status
requires evaluation. Thus, elderly or frail patients may not choose microneurovascular
tissue transfer.
Static restoration of the lower face is generally used to achieve symmetry at rest.
Slings such as harvested tensor fascia lata are commonly used7. Even if static procedures cannot achieve mimic movements, they generate limited
trauma and can be completed in a single surgical stage.
Here we presented an easy way to correct a lip deformity using a modified bull’s horn
approach. The original technique was first described by Ramirez et al1 for an upper lip lift. It consisted of an excision of the white part of the upper
lip directly beneath the nose in the shape of a bull’s horn, with advancement of the
inferior border of the incision to the area directly beneath the nose. We used the
same approach to harvest a dermoadiposal flap by using commonly discarded tissues
and adding the pedicle flap markings in the nasolabial fold with a final concealed
scar.
The patient was informed of the different techniques available to correct her defect
as a consequence of facial nerve damage. She did not suffer from any particular disease
and was considered a good candidate for a temporalis muscle transposition with a facelift.
The patient refused this option because she did not want to undergo an invasive procedure.
Because she complained of lower lip elongation, another option was offered to correct
her defect as described.
A fat transfer procedure was carried out simultaneously with the flap transfer to
correct a volume defect. At 3 months after the first surgery, a second fat transfer
session was planned to improve the residual cheek deformity bilaterally as a consequence
of the nodule removal. At 3 years of follow-up, the asymmetry correction appeared
stable and the dermoadiposal flap was a good autologous suspension material for static
correction of the lip deformity.
COLLABORATIONS
|
AC
|
Realization of operations and/or trials, Supervision
|
|
RL
|
Conception and design study, Final manuscript approval, Writing - Original Draft Preparation,
Writing - Review & Editing
|
REFERENCES
1. Ramirez OM, Khan AS, Robertson KM. The upper lip lift using the ‘bull’s horn’ approach.
J Drugs Dermatol. 2003 Jun;2(3):303-6.
2. Caggiati A, Germani A, Di Carlo A, Borsellino G, Capogrossi MC, Picozza M. Naturally
adipose stromal cell-enriched fat graft: comparative polychromatic flow cytometry
study of fat harvested by barbed or blunt multihole cannula. Aesthet Surg J. 2017
May;37(5):591-602. PMID: 28052909 DOI: https://doi.org/10.1093/asj/sjw211
3. Biglioli F, Frigerio A, Colombo V, Colletti G, Rabbiosi D, Mortini P, Dalla ET, Lozza
A, Brusati R. Masseteric-facial nerve anastomosis for early facial reanimation. J
Craniomaxillofac Surg. 2012 Feb;40(2):149-55. DOI: https://doi.org/10.1016/j.jcms.2011.03.005
4. Biglioli F, Frigerio A, Autelitano L, Colletti G, Rabbiosi D, Brusati R. Deep-planes
lift associated with free flap surgery for facial reanimation. J Craniomaxillofac
Surg. 2001 Oct;39(7):475-81. DOI: https://doi.org/10.1016/j.jcms.2010.09.003
5. Chuang DC. Technique evolution for facial paralysis reconstruction using functioning
free muscle transplantation - experience of Chang Gung Memorial Hospital. Clin Plast
Surg. 2002 Oct;29(4):449-59. DOI: https://doi.org/10.1016/S0094-1298(02)00021-4
6. Harrison DH, Grobbelaar AO. Pectoralis minor muscle transfer for unilateral facial
palsy reanimation: an experience of 35 years and 637 cases. J Plast Reconstr Aesthet
Surg. 2012;65(7):845-50. DOI: https://doi.org/10.1016/j.bjps.2012.01.024
7. Rose EH. Autogenous fascia lata grafts: clinical applications in reanimation of the
totally or partially paralyzed face. Plast Reconstr Surg. 2005 Jul;116(1):20-32;discussion:33-5.
DOI: https://doi.org/10.1097/01.PRS.0000169685.54862.18
1. Istituto Dermopatico dell’Immaticolata IDI, Rome, Italy.
Corresponding author: Rosaria Laporta Via dei Monti di Creta, 104, Rome, RM, Italy. Zipe Code: 00167 E-mail: r.laporta@idi.it
Article received: November 11, 2018.
Article accepted: April 16, 2019.
Institution: Istituto Dermopatico Dell’immacolata, Idi, Irccs, Rome, Italy.
Conflicts of interest: none.