INTRODUCTION
Pressure ulcers are alterations of the integrity of the skin and underlying
tissues, caused by pressure, most commonly on the protuberances, especially in
areas deprived of local sensitivity, which lead to necrosis and ulceration.
Data from the international literature estimate that between 3% and 14% of all
hospitalized patients develop pressure ulcers1, which emphasizes the importance of preventive measures in
patients with increased risk. The surgical treatment of pressure ulcers dates
back to 1947, with Croce and Beakes2 using
skin flaps.
The use of muscle and musculocutaneous flaps (proposed by Ger3, Minami et al.4, and Nahai et al.5)
and fasciocutaneous flaps (proposed by Hurwitz et al.6, Alonso et al.7,
Ramirez8, Calil et al.9, and Paletta et al.10) was a significant improvement to the
surgical arsenal for the treatment of these conditions. Within the widely varied
situations that arise in daily clinical practice, surgical solutions with
characteristics appropriate to the patient’s local needs are vital.
OBJECTIVE
This study aimed to describe the simultaneous correction of extensive sacral and
ischial pressure ulcers with a single flap in a 21-year-old paraplegic patient.
He was admitted with anemia, urinary infection, necrotic ulcers, and spastic
contracture in the lower limbs. After clinical treatment, he was submitted to
correction of the ulcers by rotation of a fasciomyocutaneous flap from the
gluteus maximus and posterior surface of the thigh, pediculated by the superior
and inferior gluteal artery and the posterior fasciocutaneous branch of the
thigh.
In spite of the dimensions, the flap used displayed good blood perfusion,
evolving without necrosis or dehiscence. The flap proved to be a valid option
for young patients without diseases that lead to circulatory impairment.
CASE REPORT
A 21-year-old male patient with a 1-year history of paraplegia received
inadequate care, which led to the development of multiple pressure ulcers,
including extensive right sacral and ischial ulcers. The patient was admitted
febrile, malnourished, anemic, and with urinary tract infection, necrotic
ulcers, and spastic contracture in the lower limbs.
After clinical preparation, simultaneous correction of the right sacral and
ischial ulcers through the rotation of a single fasciomyocutaneous flap was
performed.
Surgical technique
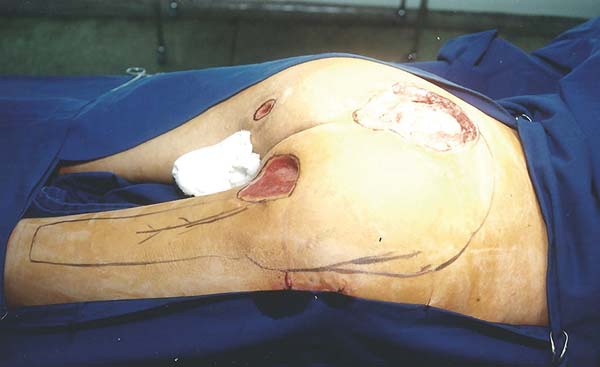
The patient was positioned in ventral decubitus, with the flap and edges of
the ulcers demarcated (Figure 1),
followed by dissection of the flap from the distal extremity while securing
the fascia to the subcutaneous cell tissue (TCSC), elevation of the gluteus
maximus and cutaneous portions (Figure 2), rotation and suturing of the flap closing the two ulcers
(Figure 3), and closing the donor
area of the thigh edge to edge. The flap and donor area evolved with good
healing (Figures 4 and 5).
Figure 1 - Demarcation of the flap and edges of the ulcers.
Figure 1 - Demarcation of the flap and edges of the ulcers.
Figure 2 - Intraoperative aspect of the elevated flap.
Figure 2 - Intraoperative aspect of the elevated flap.
Figure 3 - The flap positioned and the donor area with temporary
sutures.
Figure 3 - The flap positioned and the donor area with temporary
sutures.
Figure 4 - Postoperative aspect of the treated sacral ulcer.
Figure 4 - Postoperative aspect of the treated sacral ulcer.
Figure 5 - Postoperative aspect of the treated ischial ulcer. The
treated trochanteric ulcer is also shown.
Figure 5 - Postoperative aspect of the treated ischial ulcer. The
treated trochanteric ulcer is also shown.
RESULTS
The flap used for the simultaneous correction of the right sacral and ischial
ulcers showed good blood perfusion and evolved without necrosis or hematoma. The
patient presented mild superficial pressure sores at the proximal extremity of
the posterior thigh donor area by tension in the suture line, which healed
spontaneously, and presented serous-sanguineous secretion drainage in its
distal end, which did not prevent proper healing. We emphasize that the tension
did not impair the venous return of the right lower limb.
DISCUSSION
According to Alonso et al.7 and Paleta et
al.10, the circulation of the
posterior fasciocutaneous portion of the thigh flap was programed to be
nourished from the fasciocutaneous branch of the inferior gluteal artery. The
anatomical studies of Calil et al.9 showed
an intersection between the first and second perforating branches of the deep
femoral artery, which leads to an extensive area of cutaneous perfusion in the
posterior aspect of the thigh, which allows the preparation of large flaps.
The study of Hurwitz et al.6 showed
inferior gluteal artery anastomoses with branches of the medial femoral
circumflex artery. When these and other anastomotic vessels were sectioned, the
inferior gluteal artery could supply the circulation of the posterior region of
the thigh.
Ramirez8 mentioned the importance of the
first perforating artery for the perfusion of the posterior fasciocutaneous
thigh flap. In two-thirds of flaps in the study, the artery was ligated without
impairment of the flap. The author also mentioned the importance of the branches
of the medial femoral circumflex artery with its more superior and medial
location than the first perforator.
Owing to the arc of rotation of the flap used in the present study and the
inclusion of the gluteus maximus muscle, ligation of the first and second
perforating arteries was needed to maintain the perfusion of the posterior
fasciocutaneous portion of the thigh through the inferior fasciocutaneous
gluteal artery branch. The inclusion of the gluteus maximus muscle in the flap
enabled a better filling of the extensive sacral ulcers.
In the event of necrosis of the fasciocutaneous portion, one option would be to
use the myocutaneous flap of the local gracilis or fasciocutaneous. In sacral
ulcer relapse, a fasciocutaneous flap may be made for closure alone or
associated with a musculocutaneous or fasciocutaneous flap of the contralateral
gluteal region.
CONCLUSIONS
The use of fasciomyocutaneous flaps from the gluteus maximus and posterior
surface of the thigh proved to be a good surgical option for simultaneous
correction of right sacral and ischial ulcers as demonstrated in the case of a
young patient described herein, who had no illnesses that would lead to
circulatory impairment and clinical imbalance.
COLLABORATIONS
|
ACJ
|
Conception and design of the study; execution of the operations
and/or experiments; and drafting and preparation of the original
manuscript.
|
|
RSF
|
Final approval of the manuscript; and drafting; revision; and editing
of the manuscript.
|
REFERENCES
1. Bergstrom N, Allman RM, Alvarez OM, Carlsson CE, Eaglesetein W,
Frantz RA, et al. Pressure ulcer in adults: prediction and prevention.
Rockville: Agency for Health Care Policy and Research; 1992.
2. Croce EJ, Beakes HC. The operative treatment of decubitus ulcer. N
Engl J Med. 1947;237(5):141-9.
3. Ger R. The surgical management of decubitus ulcers by muscle
transposition. Surgery. 1977;69(1);106-10.
4. Minami RT, Mills R, Pardoe R. Gluteus maximus myocutaneous flaps for
repair of pressure sores. Plast Reconstr Surg.
1977;60(2):242-9.
5. Nahai F, Silverton JS, Hill HL, Vasconez LO. The tensor fascia lata
musculocutaneous flap. Ann Plast Surg. 1978;1(4):372-9.
6. Hurwitz DJ, Swartz WM, Mathes SJ. The gluteal thigh flap: a
reliable, sensate flap for the closure of buttock and perineal wounds. Plast
Reconstr Surg. 1981;68(4):521-32.
7. Alonso N, Carramaschi F, Calonge HCF, Gemperli R, Monteiro Júnior
AA, Ferreira MC. Retalho fasciocutâneo posterior da coxa no tratamento de
úlceras de pressão. Rev Bras Ortop. 1986;21(1):13-5.
8. Ramirez OM. The distal gluteus maximus advancement musculocutaneous
flap for coverage of trochanteric pressure sores. Ann Plast Surg.
1987;18(4):295-302.
9. Calil JA, Ferreira LM, Neto MS, Castilho HT, Garcia EB. Aplicação
clínica do retalho fasciocutâneo da região posterior da coxa em V-Y. Rev Assoc
Med Bras. 2001;47(4):311-9.
10. Paletta C, Bartell T, Shahadi S. Applications of the posterior thigh
flap. Ann Plast Surg. 1993;30(1):41-7.
1. Universidade Estadual de Londrina, Londrina,
PR, Brazil.
2. Universidade Federal do Paraná, Curitiba, PR,
Brazil.
Corresponding author: Antonio Chiquetti Junior, Rua Paes Leme, nº
1264, sala 601 - Jardim das Américas - Londrina, PR, Brazil, Zip Code:
86010-610. E-mail: chiqueti@sercomtel.com
Article received: April 12, 2018.
Article accepted: October 1, 2018.
Conflicts of interest: none.