

Original Article - Year 2016 - Volume 31 -
Abdominoplasty after bariatric surgery: experience in 315 cases
Abdominoplastia pós cirurgia bariátrica: experiência de 315 casos
ABSTRACT
INTRODUCTION: The abdomen is a critical region and is subjected to body contour deformity after significant weight loss. Knowing the profile of patients who undergo abdominoplasty after bariatric surgery facilitates the choice of the optimal time and surgical technique to restore abdominal contour, which is associated with a minimal rate of complications.
METHODS: A cross-sectional, descriptive, analytical, and retrospective clinical study was performed on medical record data of 315 patients who underwent abdominal dermolipectomy following bariatric surgery from January 2013 to December 2014.
RESULTS: A total of 265 female and 50 male patients were analyzed, with an average age of 39.9 years and an average body mass index of 27.5 kg/m2 after weight loss. The average time interval between bariatric surgery and dermolipectomy was 3 years and 11 months. Anchor abdominoplasty was used in 252 patients, while suprapubic transverse abdominoplasty was performed in 63 patients. The complication rate was 17.3%, including minor complications such as hematomas, seromas, and pathological scars, in addition to one case of pulmonary embolism.
CONCLUSION: The epidemiological profile of patients with deformity of the abdominal contour after bariatric surgery was in agreement with that reported in the current literature, except for earlier hospital discharge in the group studied.
Keywords: Reconstructive surgical procedures; Bariatric surgery; Gastroplasty; Abdominoplasty; Obesity.
RESUMO
INTRODUÇÃO: O abdome é considerado área crítica de deformidade do contorno corporal após perda ponderal significativa. Conhecer o perfil dos pacientes submetidos à abdominoplastia pós-cirurgia bariátrica facilita a escolha do tempo ideal e da técnica cirúrgica que visa restaurar este contorno com uma taxa mínima de complicações.
MÉTODOS: Estudo clínico, transversal, descritivo, analítico e retrospectivo com dados de 315 prontuários de pacientes submetidos à dermolipectomia abdominal pós-cirurgia bariátrica de janeiro de 2013 a dezembro de 2014.
RESULTADOS: Foram analisados 265 pacientes do gênero feminino e 50 do gênero masculino, com idade média de 39,9 anos e índice de massa corporal médio de 27,5 Kg/m2 após emagrecimento. O tempo médio de intervalo entre a cirurgia bariátrica e a dermolipectomia foi de 3 anos e 11 meses. A abdominoplastia em âncora foi utilizada em 252 pacientes e em 63 realizou-se abdominoplastia com cicatriz transversal suprapúbica. A taxa de complicações foi de 17,3%, incluindo complicações menores como hematomas, seromas e cicatrizes patológicas e um caso de embolia pulmonar.
CONCLUSÃO: O perfil epidemiológico dos pacientes com deformidade de contorno abdominal pós-cirurgia bariátrica estudados assemelha-se ao apresentado na literatura atual, exceto pela alta hospitalar precoce.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Cirurgia bariátrica; Gastroplastia; Abdominoplastia; Obesidade.
Obesity is considered pandemic and creates significant health risks in a population1,2. The increasing number of obese individuals worldwide has also resulted in an increased number of those seeking to lose weight. Whether through physical exercise, food reeducation, drug therapy, and/or bariatric surgical procedures, significant weight loss can lead to skin sagging and body contour deformities1-5.
A resolution published by the Federal Council of Medicine in January 20166 increased the number of approved comorbidities for bariatric surgery in patients with a body mass index (BMI) between 35 and 40 kg/m2. In a few years, this will lead to an increase in the number of patients with postoperative body contour deformities.
The abdomen is a critical area that undergoes deformity after massive weight loss. This creates new problems for patients, including difficulties with personal hygiene, social interaction at work, and even aspects of intimacy5,7-9.
The desire to improve physical contour and quality of life has resulted in an increased demand for plastic surgery2,6,8. Professionals should be able to correctly diagnose these deformities and recognize the different alternatives that need to be offered to ensure appropriate treatment1,2,9. Several surgical techniques aim at restoring abdominal contour. The choice of procedure should be individualized to improve the deformity in each patient7,8,10.
Knowing the profile of patients who undergo significant weight loss facilitates the correct clinical diagnosis, which enables the surgeon to recommend more effective operative treatments.
OBJECTIVE
This study aimed to analyze the profiles of patients undergoing abdominal dermolipectomy following bariatric surgery, with focus on the author's experience in 315 cases.
METHODS
This was a clinical, cross-sectional, descriptive, analytical, and retrospective study. The medical records of 322 patients who underwent abdominoplasty after bariatric surgery from January 2013 to December 2014 were evaluated at the Clinic of Plastic Surgery of Felício Rocho Hospital, Belo Horizonte, MG.
Four medical charts were excluded from the study because the data were incomplete. Another 3 were also excluded, because the patients had previously undergone abdominal contour treatment, which would have categorized subsequent surgery as secondary abdominal dermolipectomy. The patients whose medical records were used in the study provided Informed Consent.
The study collected data of 315 patients who underwent bariatric surgery at least one year prior, and had a stable weight for at least 3 months. The variables studied were: gender, age, BMI before and after bariatric surgery, time interval between bariatric surgery and abdominoplasty, method used to perform gastroplasty (by laparoscopy or laparotomy), time of hospital discharge and whether the abdominoplasty used a classic or anchor technique.
The principles of the Declaration of Helsinki revised in 2000, and of Resolution 196/96 of the National Health Council were followed in this study.
The data obtained were entered in a Microsoft Office Excel spreadsheet (Microsoft Corporation, USA) for subsequent storage and analysis of the variables.
No conflicts of interest were reported and there were no funding sources.
RESULTS
Gender distribution was uneven, with a predominance of females: 265 (84.1%) patients were females and 50 (15.9%) were males.
The ages ranged between 19 and 71 years. The average age was 39.9 years. Similar averages were observed when the two genders were analyzed: 39.6 years in the female group and 41.4 years in the male group.
The minimum time between bariatric surgery and abdominoplasty was 1 year, while the maximum was 14 years and 2 months. The average time interval between surgeries was 3 years and 11 months. In males, this mean interval was longer, i.e., 5 years and 2 months. In females, this was 3 years and 10 months.
BMI values ranged between 31.57 and 71.7 kg/m2 before bariatric surgery. The mean BMI before bariatric surgery was 43.8 kg/m2. In female patients, the average was 43.3 kg/m2 while in males, the average was 46.7 kg/m2. After bariatric surgery, with weight loss and stabilization, the overall average was 27.5 kg/m2, with a mean value of 27.2 kg/m2 for females and 29.4 kg/m2 for males.
Of 315 studied cases, 159 (50.5%) had undergone open gastroplasty, while 156 (49.5%) had laparoscopic gastroplasty. Some preoperative cases are presented in Figures 1 to 3.
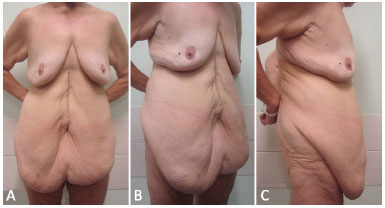
Figure 1. A: Preoperative frontal view of a 60-year-old female patient who underwent open bariatric surgery 3 years prior, with a weight loss of 68 kg. Previous BMI of 51.1 kg/m2, and BMI of 27.3 kg/m2 at the time of abdominoplasty. Frontal view; B: Lateral view; C: Right profile view. BMI: Body Mass Index.

Figure 2. A: Preoperative frontal view of a 23-year-old female patient who underwent laparoscopic bariatric surgery 2 years prior, with a weight loss of 52 kg. Previous BMI: 44.8 kg/m2; BMI at the time of abdominoplasty: 25.7 kg/m2; B: Lateral view; C: Right profile view. BMI: Body Mass Index.

Figure 3. A: Preoperative frontal view of a 43-year-old female patient who underwent laparoscopic bariatric surgery 2 years and 8 months prior, with a weight loss of 45 kg. Previous BMI: 40.4 kg/m2; BMI at the time of abdominoplasty: 23.8 kg/m2; B: Lateral view; C: Right profile view. BMI: Body Mass Index.
Sixty-three (20.0%) conventional abdominoplasties and 252 (80.0%) anchor abdominoplasties were performed. All patients who underwent open gastroplasty also underwent anchor abdominoplasty with umbilical amputation and neomphaloplasty, as described by Donnabella11.
In patients who underwent laparoscopic gastric bypass, the choice of abdominoplasty was dictated by the type of abdominal deformity presented by each patient. The patient's opinion and wishes were taken into consideration. In cases with a great transverse excess of skin sagging, we performed an anchor abdominoplasty. When the abdominal contour deformity had excess vertical sagging as the main component, we performed conventional abdominoplasty, with a suprapubic transverse incision.
In all cases of conventional abdominoplasty, the authors chose to use a closed tubular drainage system. On the other hand, in cases of anchor abdominoplasty, due to restricted detachment while using the technique and fixation of flaps to the aponeurosis, no drains were used.
The average operative time was 150 minutes.
In 307 (97.5%) cases, the patient was discharged 1 day after surgery, and 2 days after surgery in 8 (2.5%) cases. The use of an elastic compressive belt was not indicated in any of the cases.
All patients returned to the hospital at least 4 times after surgery: the first visit was between the third and seventh postoperative day and the second visit was 2 weeks postoperatively, regardless of the technique used. The third evaluation occurred approximately 30 days after surgery. In late postoperative assessment, the patients were followed for a period ranging from 3 months to 1 year.
Complications occurred in 55 (17.4%) patients, and concomitant complications were also detected in 5 cases. Two hematomas, 19 seromas, 13 minor dehiscences, 5 local infections (infected seroma and cellulitis), and 21 pathological scars (11 enlarged scars, 6 wound-healing adhesions, and 4 hypertrophic scars) were observed.
There was 1 (0.3%) case of diagnosed deep vein thrombosis (DVT), which evolved to a pulmonary embolism (PE) that required hospitalization to ensure appropriate treatment. The 2 cases of hematoma were drained at the surgical center during the immediate postoperative period. Other local complications were treated and followed up in the outpatient clinic, and all were satisfactorily resolved.
Satisfaction with the results was reported by 311 (98.7%) patients after surgery. Only 4 (1.3%) patients reported dissatisfaction, and all associated this complaint with the final appearance of the scar, which in 2 cases (0.6%) was enlarged and in the other 2 (0.6%) was hypertrophic.
No patient complained about their body contour after abdominoplasty. Some results are shown in Figures 4 to 6.
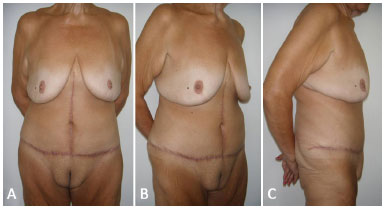
Figure 4. A: 6-month postoperative frontal view of the patient shown in Figure 1A, 1B, and 1C. Good recovery of the abdominal contour is observed, along with proper healing and a new navel presenting a harmonious aspect; B: Lateral view; C: Right profile view.
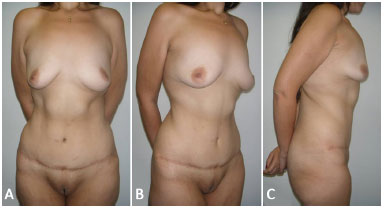
Figure 5. A: 9-month postoperative frontal view of the patient shown in Figure 2A, 2B, and 2C. Significant improvement of the abdominal contour deformity and good scar evolution; B: Lateral view; C: Right profile view.
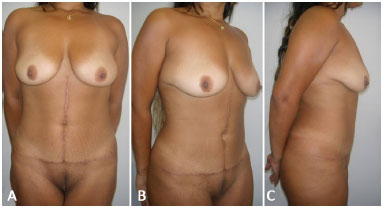
Figure 6. A: 7-month postoperative frontal view of the patient shown in Figure 3A, 3B, and 3C. There is good definition of the body contour with proper healing and a new, well positioned navel; B: Lateral view; C: Right profile view.
DISCUSSION
The large weight loss after bariatric surgery leads to significant deformities of body contour1-5,11-15. The abdominal region is a critical point for this deformity, generating consequences for the personal and social life of patients1,2,9,14,15.
The search for the best treatment to restore abdominal contour led to the development of several abdominoplasty techniques1,2,7-10. The optimal technique should be based on an individualized analysis of the deformity in each patient. Knowing the profile of these patients facilitates the correct clinical diagnosis and leads to satisfactory results.
The prevalence of females in this study is consistent with that reported by various authors who studied patients undergoing abdominoplasty after significant weight loss1,2,9-11,15-17. The average age of the patients was about 40 years, which was also in agreement with that found in similar reports in the literature1,2,17,18.
The average time of 55 months between bariatric surgery and abdominoplasty was longer than that reported in the literature1,2,7,10. This is probably due to the fact that the authors waited for the patients to achieve weight stability after bariatric surgery, before performing surgery to correct the abdominal contour.
The average BMI at the time of bariatric surgery is quite variable. The average of 43.8 kg/m2 was lower than that reported in adult patients by Tardelli et al.10.
At the time of abdominoplasty, the average BMI of the patients in this study was 27.5 kg/m2. These values are similar to those reported by several authors2,16,18,19. Some of these authors used a threshold of 30.0 kg/m2 to include patients in a study of abdominal contour7.
In the current study, this threshold was not considered, since the authors believe that the BMI alone cannot be a contraindication to abdominoplasty. Before bariatric surgery, some patients had a BMI close to 70.0 kg/m2. However, it was more important to comparatively evaluate the weight loss, the body contour deformities in these patients, and their clinical conditions.
The decision by the authors to perform anchor abdominoplasty in all cases that previously underwent an open approach was based on two factors: the possibility of removing a previous median supraumbilical scar, which in many cases was enlarged or hypertrophic, and the possibility of creating a new navel.
The choice of umbilical amputation and neomphaloplasty was based on the ease of execution, good esthetic results, minor local complications, and the supportive opinion of other authors in the literature15,20. The technique used to perform neomphaloplasty was previously described by one of the authors of this study11. In patients with a previous laparoscopic approach who presented with a great transverse excess of skin sagging, the technique of anchor abdominoplasty was also chosen, a trend supported by several authors in the literature in recent years9-11,15.
In those patients who underwent laparoscopic bariatric surgery and presented with an abdominal deformity with a predominance of excess vertical sagging and little transverse excess, we recommended conventional abdominoplasty, using a suprapubic transverse incision.
Surgical complications occurred in 17.4% of the cases, and most were minor. This was a lower rate than the average of 20% reported in the literature2,3,17,19,21. Most of the authors also described the prevalence of minor complications, including wound healing changes, seromas, and small dehiscences. André5 and Cavalcante3 reported the occurrence of major complications, such as partial flap necrosis and atelectasis with pneumonia, but always at low rates. The current study reiterates this finding, with a major complication rate of 0.3%, corresponding to one case of DVT.
The patients were discharged 1 day after surgery. This was earlier than that reported by most published studies, which usually indicated that patients were discharged 2 to 3 days after surgery3,10.
Lage et al.1 also reported an early discharge profile, which was related to the small detachment of flaps and early encouragement of ambulation, the same reasons that can be cited in this study. Only patients with walking difficulty and cases of hematoma drainage were discharged 2 days after surgery. Postoperative monitoring was the same as that widely described in the literature, which was extended for an average period of 1 year1,2,5,10.
We believe that the efficacy of treatment of abdominal deformities after major weight loss is due to the proper choice of surgical technique in each case, without taking into account the presence or absence of prior supraumbilical midline scars, while recommending anchor abdominoplasty.
The absence of a previous midline scar should not be a contraindication to anchor abdominoplasty, but its presence facilitates the acceptance of this technique by the patient. The plastic surgeon should be able to identify the technique that will most benefit the patient and guide the patient through the available options, since the opinion of the patient should always be considered in the final decision.
CONCLUSION
The epidemiological profile of patients with deformities of abdominal contour after bariatric surgery was similar in this study to that reported in the current literature, except for earlier hospital discharge in this study.
The selection of optimal surgical technique for each case is crucial in the treatment of abdominal deformities after major weight loss.
The decision about the best technique for each patient must be based on evaluation by the plastic surgeon, while always considering the opinion of the patient.
COLLABORATIONS
AD Analyzed and/or interpreted the data; performed statistical analyses; approved the final version of the manuscript; elaborated and designed the study; performed surgeries and/or experiments; wrote the manuscript, and/or critically reviewed its content.
LN Analyzed and/or interpreted the data; performed statistical analyses; approved the final version of the manuscript; elaborated and designed the study; performed surgeries and/or experiments; wrote the manuscript, and/or critically reviewed its content.
BBB Analyzed and/or interpreted the data; performed statistical analyses; approved the final version of the manuscript; performed surgeries and/ or experiments; wrote the manuscript, and/or critically reviewed its content.
FPS Analyzed and/or interpreted the data; performed statistical analyses; approved the final version of the manuscript; wrote the manuscript and/or critically reviewed its content.
REFERENCES
1. Lage RR, Amado BN, Sizenando RP, Heitor BS, Ferreira BM. Dermolipectomia abdominal pós-gastroplastia: avaliação de 100 casos operados pela técnica do "peixinho". Rev Bras Cir Plást. 2011;26(4):675-9.
2. Tuma Jr P, Batista BPSN, Milan LS, Faria GEL, Milcheski DA, Ferreira MC. Abdominoplastia vertical para tratamento do excesso de pele abdominal após perdas ponderais maciças. Rev Bras Cir Plást. 2012;27(3):445-9.
3. Cavalcante HA. Abdominoplastia após perda de peso maciça: abordagens, técnicas e complicações. Rev Bras Cir Plást. 2010;25(1):92-9.
4. Zammerilla LL, Zou RH, Dong ZM, Winger DG, Rubin JP, Gusenoff JA. Classifying severity of abdominal contour deformities after weight loss to aid in patient counseling: a review of 1006 cases. Plast Reconstr Surg. 2014;134(6):888e-94e.
5. André FS. Cirurgia plástica após grande perda ponderal. Rev Bras Cir Plást. 2010;25(3):532-9.
6. Brasil. Conselho Federal de Medicina. Resolução no. 2.131/2015, de 12 de novembro de 2015. 13 Jan 2016; Seção 1. Brasília: Diário Oficial da União; 2016.
7. Rocha RI, Gemperli R, Modolin MLA, Cintra Junior W, Velhote MCP, Ferreira MC. Cirurgias plásticas para readequação de contorno corporal de pacientes submetidos a cirurgia bariátrica durante a adolescência. Rev Bras Cir Plást. 2012;27(4):588-93.
8. de Zwaan M, Georgiadou E, Stroh CE, Teufel M, Köhler H, Tengler M, et al. Body image and quality of life in patients with and without body contouring surgery following bariatric surgery: a comparison of pre- and post-surgery groups. Front Psychol. 2014;5:1310.
9. André FS. Abdominoplastia e lifting do púbis. Rev Bras Cir Plást. 2009;24(3):35-50.
10. Tardelli HC, Vilela DB, Schwartzmann GLES, Azevedo M, Mello Júnior AM, Farina Júnior JA. Padronização cirúrgica das abdominoplastias em âncora pós-gastroplastia. Rev Bras Cir Plást. 2011;26(2):266-74.
11. Donnabella A. Reconstrução anatômica da cicatriz umbilical. Rev Bras Cir Plást. 2013;28(1):119-23.
12. Koolen PG, Ibrahim AM, Kim K, Sinno HH, Lee BT, Schneider BE, et al. Patient selection optimization following combined abdominal procedures: analysis of 4925 patients undergoing panniculectomy/abdominoplasty with or without concurrent hernia repair. Plast Reconstr Surg. 2014;134(4):539e-50e.
13. Lievain L, Aktouf A, Auquit-Auckbur I, Coquerel-Beghin D, Scotte M, Milliez PY. Abdominoplasty complications: particularities of the post-bariatric patients within a 238 patients series. Ann Chir Plast Esthet. 2015;60(1):26-34.
14. Kornstein A. SERI Surgical Scaffold as an Adjunct for Circumferential Abdominoplasty and Lower Body Lift. Plast Reconstr Surg Glob Open. 2014;2(11):e244.
15. Reno BA, Mizukami A, Calaes IL, Staut JG, Claro BM, Baroudi R, et al. Neo-onfaloplastia no decurso das abdominoplastias em âncora em pacientes pós-cirurgia bariátrica. Rev Bras Cir Plást. 2013;28(1):114-8.
16. Fischer JP, Wes AM, Serletti JM, Kovach SJ. Complications in body contouring procedures: an analysis of 1797 patients from the 2005 to 2010 American College of Surgeons National Surgical Quality Improvement Program databases. Plast Reconstr Surg. 2013;132(6):1411-20.
17. Karthikesalingam A, Kitcat M, Malata CM. Abdominoplasty in patients with and without pre-existing scars: a retrospective comparison. J Plast Reconstr Aesthet Surg. 2011;64(3):369-74.
18. Iglesias M, Ortega-Rojo A, Garcia-Alvarez MN, Vargas-Vorackova F, Gonzalez-Chavez AM, Gonzalez-Chavez MA, et al. Demographic factors, outcomes, and complications in abdominal contouring surgery after massive weight loss in a developing country. Ann Plast Surg. 2012;69(1):54-8.
19. Staalesen T, Olsén MF, Elander A. Complications of abdominoplasty after weight loss as a result of bariatric surgery or dieting/postpregnancy. J Plast Surg Hand Surg. 2012;46(6):416-20.
20. Silva FN, Oliveira EA. Neo-onfaloplastia na abdominoplastia vertical. Rev Bras Cir Plást. 2010;25(2):330-6.
21. Zuelzer HB, Ratliff CR, Drake DB. Complications of abdominal contouring surgery in obese patients: current status. Ann Plast Surg. 2010;64(5):598-604.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Felício Rocho, Belo Horizonte, MG, Brazil
3. Faculdade de Medicina de Barbacena, Barbacena, MG, Brazil
Institution: Hospital Felício Rocho, Belo Horizonte, MG, Brazil.
Corresponding author:
Alfredo Donnabella
Rua dos Inconfidentes, 334/1801
Belo Horizonte, MG, Brazil Zip Code 30140-120
E-mail: adonnabella@uol.com.br
Article received: March 23, 2016.
Article accepted: October 30, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter