ABSTRACT
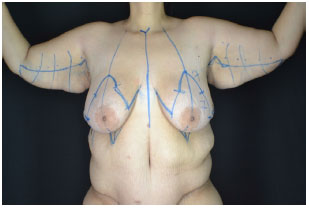
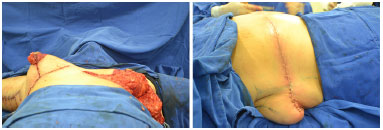
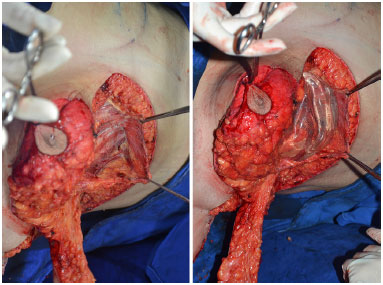
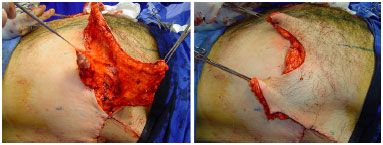
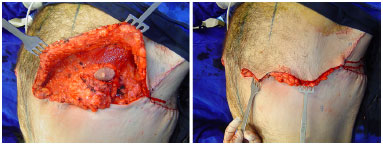
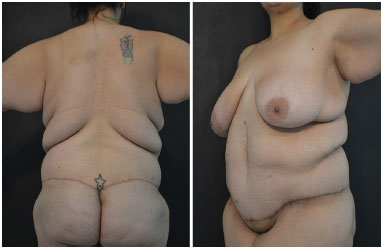
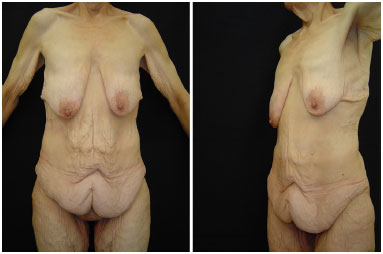
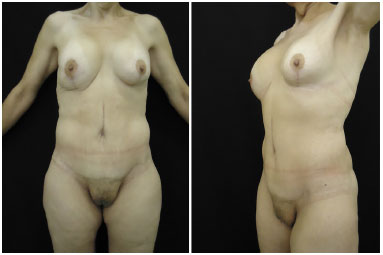
INTRODUCTION: In Brazil, 88000 bariatric surgeries were performed in 2014. After weight loss, deflation occurs around the trunk, with sagging and folding of excess skin of the breasts in the posterior dorsal region . We, therefore, propose a surgical procedure to treat upper region of the entire trunk, including breasts, side and rear back, and arms.
OBJECTIVE: To present a personal experience in brachial-dorsal mammoplasty surgeries.
METHOD: We operated 13 patients from 2007 to 2014, 11 women and two men.
RESULTS: The average age was 41.9 years. The brachial-dorsal mammoplasty was performed in all patients. In three cases, L-brachial-dorsal mammoplasty was performed, due to lower latero-posterior deformity. The average surgery duration was 4 hours and 30 minutes. The average Body Mass Index (BMI), before bariatric surgery, was 53.5 kg/m2. Weight loss ranged from 47 to 114 kg. The pre-surgery BMI ranged from 23 to 39 kg/m2. There were no cases of infection, large dehiscence or seroma. Two patients developed hematoma, requiring a new intervention for drainage.
CONCLUSION: Deformities of the thoracic region in patients with large weight loss are variable, requiring several surgical treatments that should address the entire chest as a single anatomical area. It is important to understand the deformity that each patient presents and adapt the surgical approach accordingly. The main indication for a brachial-dorsal mammoplasty is lateral drop of the inframammary fold.
Keywords: Torso; Bariatric surgery; Weight loss; Mammoplasty.