ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Extended cervicoplasty for correction of cervical changes
Cervicoplastia ampliada para correção de alterações cervicais
Original Article -
Year2011 -
Volume26 -
Issue
1
Daniel Nunes1; João Ilgenfritz Jr.2; Giovani Pires Viana1; Giovani André Pires Viana1; Kleder Gomes de Almeida1; Marcelo Cury2; Elaine Leal2; Diogo Gomes Augusto3
ABSTRACT
Introduction: Cervicoplasty is considered an important part of facial rejuvenation. Despite the various techniques already described, the search for the ideal treatment is ongoing. The technical difficulties increase in complex cases, in which excessive skin sagging and pronounced muscular ptosis affect the maintenance of long-term results. Objectives: The aim of this study was to assess the suitability of the authors' protocol for extended cervicoplasty and to discuss the technical options available for this procedure. Methods: Eighteen patients underwent "round lifting" associated with platysma flap elevation at the midcervical line and partial subplatysmal fat removal. The patients were followed for 12 months and the late postoperative outcomes were assessed by 5 surgeons of the Brazilian Society of Plastic Surgery. Results: Four patients were excluded because they were lost to follow-up. Of the 14 assessed patients, 7 (50%), 5 (35.7%), and 2 (14.3%) patients had excellent, moderate, and poor outcomes, respectively. No patient had a perfect or bad outcome. Conclusion: Extended cervicoplasty yielded satisfactory results even in difficult cases. The proposed technique is a valid alternative for the plastic surgeon, because it ensures a pleasant and natural outcome that is maintained over time.
Keywords:
Rhytidoplasty. Cervicoplasty. Neck Muscles/surgery.
RESUMO
Introdução: A cervicoplastia é considerada parte importante na cirurgia do rejuvenescimento facial. Apesar das diversas técnicas já descritas, a busca pelo tratamento ideal ainda persiste. As dificuldades aumentam nos casos considerados complexos, em que a flacidez excessiva de pele e a ptose muscular pronunciada prejudicam a manutenção dos resultados a longo prazo. Objetivos: No intuito de discutir as opções técnicas disponíveis para a cervicoplastia e apresentar a rotina cirúrgica utilizada pelo autor - com ênfase no tratamento ampliado sobre o músculo platisma - é que este estudo foi delineado. Método: Dezoito pacientes foram submetidos ao round lifting associado à confecção de retalhos musculares de platisma, na linha médio-cervical, e à retirada parcial da gordura subplatismal. Os pacientes foram acompanhados por 12 meses e o resultado pós-operatório tardio foi avaliado por cinco cirurgiões plásticos da SBCP. Resultados: Quatro pacientes foram excluídos do estudo por não retornarem para o acompanhamento pósoperatório tardio. Dos 14 pacientes avaliados, 7 (50%) tiveram o resultado classificado como excelente, 5 (35,7%) como moderado e 2 (14,3%) como fraco. Nenhum paciente teve o resultado classificado como perfeito ou ruim. Conclusão: A cervicoplastia ampliada proporcionou a obtenção de resultados satisfatórios, mesmo em casos difíceis. Acreditamos que a técnica é uma alternativa válida para o cirurgião plástico, podendo contribuir para que obtenhamos um resultado pós-operatório agradável, natural e mantido com o tempo.
Palavras-chave:
Ritidoplastia. Cervicoplastia. Músculos do Pescoço/cirurgia.
INTRODUCTION
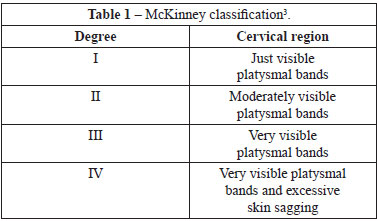
Since its origin, cervicoplasty has been considered an important part of facial rejuvenation, and its success remains defined by the ability to achieve a harmonious and natural neck1,2. Despite the various techniques already described, the search for the ideal treatment is ongoing, especially in complex or difficult cases, in which excessive skin sagging and pronounced muscular ptosis affect the maintenance of long-term results. Even today, "hard neck" treatment - a term made famous by McKinney3 (Table 1) - is considered a challenge for the plastic surgeon4-10.
Modern cervicoplasty is compilation of the fundamental techniques proposed by several authors. For example, Millard et al.11, in 1968, systematized the access to the neck through the chin crease; Baker et al.12, in 1973, demonstrated the importance of approximating the medial edges of the platysma muscles and securing their lateral margins to the sternocleidomastoid muscles; and Feldeman13, in 1990, advocated the need for vigorous plication of the platysma at the midline. Later, authors such as McKinney3, Patrocínio and Patricínio6, and Pontes and Pontes14, among others, advocated the need for a more aggressive approach to cervicoplasty in complex cases, including subplatysmal fat resection and muscular flap elevation at the cervical midline8,15-17.
The aim of this study was to assess the suitability of the authors' protocol for extended cervicoplasty.
METHODS
All patients scheduled for cervicoplasty at the private clinics of the lead author between January 2007 and June 2009 were enrolled in this prospective study. The classic technique of "round lifting", recommended by Pitanguy18, was used in all cases along with platysma flap elevation at the cervical midline and partial subplatysmal fat removal. The surgical technique is summarized below.
Surgical Technique
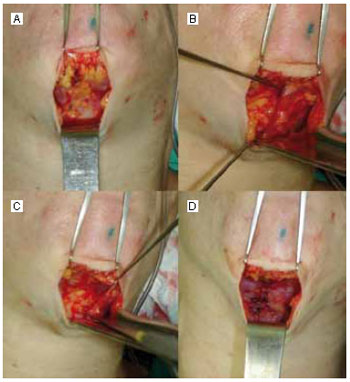
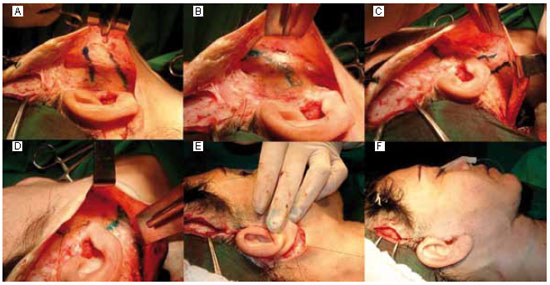
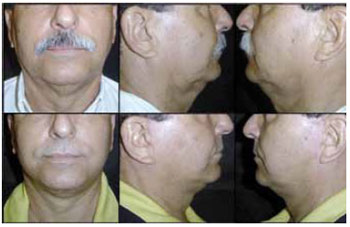
The procedure was performed under light sedation, administered by an anesthesiologist, with fentanyl (0.05 mg/ml IV) and midazolam (5 mg/ml IV). The patient was positioned in the prone position with the head flexed, and antisepsis was ensured with 2% chlorhexidine solution followed by placement of sterile drapes. The surgeon stood behind the patient's head and, with methylene blue, marked the chin crease, ranging from 4 cm to 6 cm. Then, the cervical region was anesthetized by infiltration of about 100 ml of a solution containing 0.125% lidocaine and 1:200,000 epinephrine. An 11 blade was used to create a small incision for mild or moderate liposuction of the midcervical region, depending on the case characteristics. Then, a 15 blade was used to incise the marked chin crease, and the region was widely dissected with Metzenbaum scissors. The dissection involved the jaw line, anterior edge of the sternocleidomastoid muscles, and cricoid cartilage, showing the anatomical limits of the platysma. Then, the middle portion of each platysma muscle was resected, when these were in excess. The remaining medial edge of each platysma muscle was laterally dissected by about 2.5 cm to release it from the underlying musculature, and 2 muscular flaps were elevated. The subplatysmal fat was partially removed with Metzenbaum scissors. Then, the medial edges of the platysma flaps were approximated at the midline and sutured in a single layer (about 5-8 cm long) with simple 3-0 monofilament nylon sutures from the chin incision to the region of the hyoid bone (Figure 1). Finally, the classical sequence "round lifting"18 was performed for plication of the SMAS-platysma system, at the malar, parotid, and infra-auricular regions (including the lateral border of the sternocleidomastoid; Figure 2) to improve the outcome.
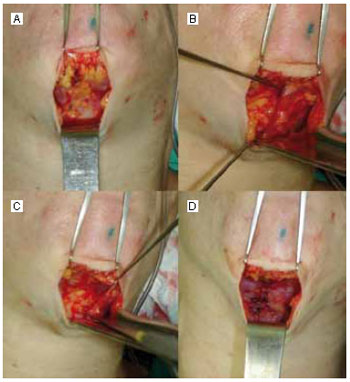
Figure 1 - Intraoperative period of patient K. A: Wide cervical dislocation and view of the medial edges of the bilateral platysma muscles; B: Medial border detachment of the left platysma and view of the subplatysmal fat; C: Left platysma flap elevation and partial removal of the subplatysmal fat; D: Advancement of 2 muscular flaps and suturing at the midcervical line.
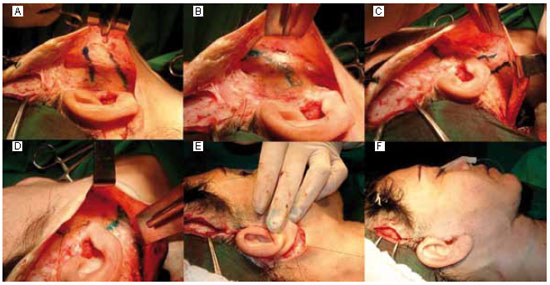
Figure 2 - Transoperative period of patient K. A: Marking the area of plication in the right malar-parotid region; B: Plication outcome; C: Marking the area of plication in the right infra-auricular region; D: Plication outcome; E: Placement of deep sutures for cervical flap support in the right auricular shell; F: Final aspect of cervicoplasty.
After completion of the indicated ancillary procedures in each case, a suction drain, skin sutures, and a pressure dressing were placed. After the first 24 h postoperatively, the drain was removed and the dressing was replaced with a specific cervical compression mesh. The patient was discharged and monitored as an outpatient. The sutures were removed on the seventh postoperative day. The patient was recommended absolute bed rest for 7 days, and lymphatic drainage was carried out by a physiotherapist from the third postoperative day. Thereafter, the patient was monitored weekly in the first month and every 2 months until the seventh month. Twelve months after the procedure, the last examination was performed. Patients who did not return for all the follow-ups were excluded from the analysis.
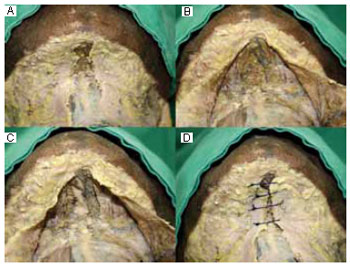
In an illustrative and didactic manner, Figure 3 shows images of anatomical dissections performed on formalinfixed specimens to demonstrate the platysmal detachment plane, subplatysmal fat removal, and muscular flap production at the midline.
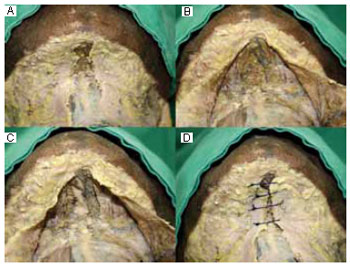
Figure 3 - Cadaveric neck dissection. A: Skin and subcutaneous tissue removal, exposing the bilateral platysma muscles; B: Dissection and muscular elevation with subplatysmal fat exposure; C: Subplatysmal fat removal, while maintaining the vascular plexus, and exposure of the underlying musculature; D: Illustrative approach to platysma flaps without muscular sectioning.
Assessment of Outcomes
The surgical outcomes were assessed by 5 surgeons of the Brazilian Society of Plastic Surgery (JI Jr, MC, EL, GAPV, and GPV) using the preoperative and late postoperative (12 months) photographs. The assessments, based on the modified method of Antell and Orsesk10, were scored as follows: 1 point = no improvement or poor outcome; 2 points = mild improvement; 3 points = moderate improvement; 4 points = substantial improvement; and 5 points = perfect outcome. The scores for each patient were summed and the result was deemed bad (5-8 points), poor (9-13 points), moderate (14-18 points), excellent (19-23 points), or perfect (24-25 points).
RESULTS
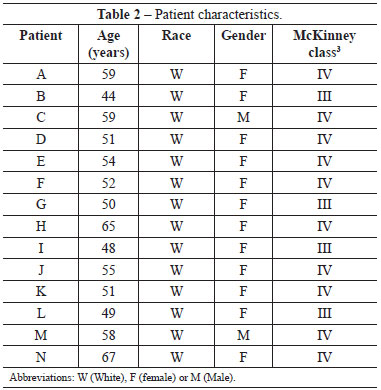
Of the 18 patients who underwent extended cervicoplasty, 4 were excluded because they did not return for the follow- up visits. The patient characteristics are summarized in Table 1.
The mean (standard deviation) surgical time was 225 (47) min. No difficulty was encountered during platysma flap elevation and subplatysmal fat removal. All the patients were discharged about 24 h after the procedure. Their recovery was satisfactory, without complications, and only 1 patient (patient D, smoker, and McKinney class IV) developed hematoma and bilateral superficial necrosis in the infra-auricular region, resulting in a hypochromic scar.
Table 2 shows the assessment scores allotted by each plastic surgeon and the surgical outcomes. Figure 4 shows the comparison between the McKinney classification and the final scores of each patient. In the 12th postoperative month, 7 (50%) patients had an excellent outcome, 5 (35.7%) had a moderate outcome, and 2 (14.3%) had a poor outcome. No patient had a perfect or bad outcome.
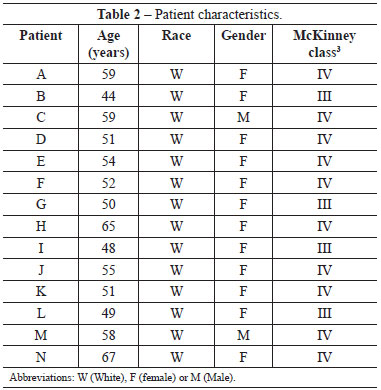
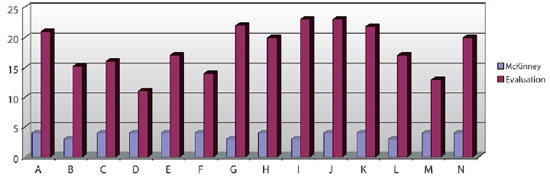
Figure 4 - Relationship between the McKinney classification and the final scores of each patient.
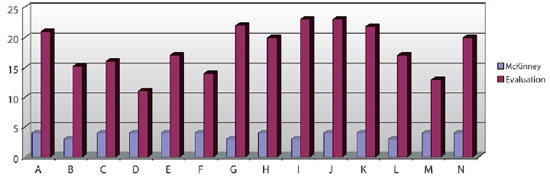
Figures 5 to 10 show the preoperative and 12-month postoperative photographs (frontal, left, and right views) of some patients.

Figure 5 - Preoperative and postoperative photographs of patient G.
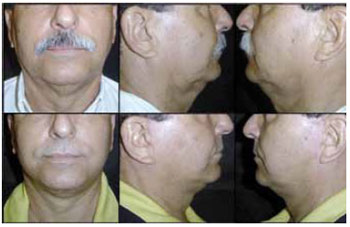
Figure 6 - Preoperative and postoperative photographs of patient M.

Figure 7 - Preoperative and postoperative photographs of patient H.

Figure 8 - Preoperative and postoperative photographs of patient J.

Figure 9 - Preoperative and postoperative photographs of patient K.

Figure 10 - Preoperative and postoperative photographs of patient E.
DISCUSSION
The literature seems to show a consensus regarding several aspects of the "hard neck" approach: the need for more effective technical options to deliver superior results has been described by several authors for years3,6,8,13,16,19,20.
Extended cervicoplasty, a combination of several surgical procedures, is a much recommended alternative by plastic surgeons who aim at high-quality treatment of complex cases9,15. According to Cardoso de Castro et al.2,15, in these cases, minor procedures, frequently indicated by inexperienced surgeons, yield limited and ephemeral outcomes besides causing complications. To achieve excellent outcomes in difficult cases, the extended cervicoplasty procedure described herein was performed with several technical options: neck liposuction21, wide detachment of the cervical subcutaneous tissue, partial subplatysmal fat removal6, elevation and advancement of platysma flaps at the midline22, and plication of the SMASplatysma complex at the malar region (cranial vector) and sternocleidomastoid region (side vector)15,18.
At present, superficial neck liposuction is performed by most surgeons. It ensures a smooth approach to the neck, reducing the occurrence of irregularities and facilitating posterior detachment with scissors2,8,16,17,21,23. Wide subcutaneous detachment, by means of a chin incision, is also considered important in difficult cases of cervicoplasty14,15,24. Pontes and Pontes14, Marchac et al.23, Cardoso de Castro25, and Gomes Filho et al.24 advocated this procedure, facilitating access to the cervical structures and the subsequent accommodation of skin. Some authors, however, argue for smaller detachments16,21. Although limited dissections preserve the skin quality and minimize the risk of complications, when compared with extensive rhytidoplasty16,21, we are of the opinion that wider detachments enable better treatment of the neck, especially in complex cases, as described by Cardoso de Castro et al.15.
Among the techniques used in this study, subplatysmal fat removal is the least discussed in the literature. Pontes and Pontes14 advocated this procedure, claiming that it enables superior outcomes. According to Patrocínio and Patrocínio6, the partial removal of subplatysmal fat enables greater advancement of the platysma toward the midline, reducing stress on the muscle and enhancing the outcome. Zins and Fardo16, Knize8, Gryskiewicz17, and Cardoso de Castro2 advocated subplatysmal fat removal when it is excessive. Neves et al.26, however, disagreed, stating that subplatysmal fat removal has more risks than benefits. Cardoso de Castro2 warned that excessive fat removal could cause inconvenient irregularities in the submental skin. According to Zins and Fardo16, great advocates of the technique, subplatysmal fat removal should not exceed the lower edge of the digastric muscle. From the present results, subplatysmal fat removal enables better approximation of the medial edges of platysma flaps, minimizing tension on the midline sutures, allowing long-lasting and natural outcomes, and reducing morbidity after cervicoplasty.
Platysma flap preparation, although described for years, is also undervalued in the literature today. In general, most authors have advocated only simple plication of the platysma at the midline8,16. This procedure repositions the elements supporting the neck but yields disappointing and ephemeral outcomes in more complex cases, with pronounced sagging2,5,6,9,15. Since Connell's paper22, in 1978, several authors achieved excellent results with platysma flaps at the midline of the neck. In 1979, Aston27, who advocated the importance of muscular flap elevation, developed a procedure that was later called "Aston's platysmoplasty". Zins and Fardo16 obtained excellent results with this technique. The anatomical dissections presented herein demonstrate the existence of a well-defined cleavage plane between the medial border of the platysma and the underlying musculature. Labbé et al.9 already identified a similar plane at the lateral border of the platysma. During cervicoplasty in this study, platysma flap elevation was facilitated by extensive muscular dissection in the aforementioned cleavage plane; subplatysmal fat removal also facilitated the approximation of these flaps, avoiding the need for sectioning the platysma. Aston27, Zins and Fardo16, and Cardoso de Castro2 proposed sectioning of the medial edges of the platysma below the hyoid bone. Aston27 emphasized that, without such sectioning, muscular flap elevation would skeletonize the neck. Further, Neves et al.26 stated that, without this sectioning, the technique would become considerably more difficult. However, platysmal sectioning was not performed in this study, because the combination of techniques for extended cervicoplasty was considered adequate to achieve satisfactory results with lower morbidity, besides avoiding platysmal weakening8.
We, as do many authors, consider the treatment of the SMAS-platysma complex as an essential part of cervicoplasty in difficult cases, coupled with the previously described midcervical approach2,9,15,25. Horizontal plication of the SMAS in the malar region ensures that the midfacial rise vector is vertically directed, not only latero-superior. This rise corrects sagging in the middle region of the mandible15. Vertical infra-auricular plication, secured on the sternocleidomastoid, ensures lateral traction of the platysma, which is considered essential for achieving a harmonious neck profile9,23. The depth approach, only in the midline of the neck, causes inappropriate treatment of the jaw line and submandibular gland ptosis5,15.
Analysis of surgical outcomes is essential to determine the success or failure of a technique. Cardoso de Castro et al.15 considered the assessment of a facial surgery outcome to be very difficult, subjective, and variable. Patrocínio and Patrocínio6, for example, measured only the degree of patient satisfaction in the postoperative period. Labbé et al.9 credited little scientific value to patient self-assessment. Ellenbogen and Karling28, Flores et al.7, Labbé et al.9, and Gryskiewicz17 used various assessment methodologies comparing different cerebrospinal profilometry angles, which hinders its applicability. For simpler and straightforward assessments that are comparable with other techniques, the methodology proposed by Antell and Orsesk10 was applied in this study. By assessing specific points preoperatively and postoperatively, a simple, efficient, fast, and reproducible method was developed.
The timing of postoperative assessment has also been discussed in the literature. Ellenbogen and Karling28, Antell and Orsesk10, Gryskiewicz17, and Labbé et al.9 argued that the minimum time to assess the outcomes of cervicoplasty properly is 12 months. On the other hand, Cardoso de Castro et al.29 and Patrocínio and Patrocínio6 stated that the outcomes can be assessed in 4-6 months. By using only the methodology of Antell and Orsesk10, the outcomes were assessed 12 months after cervicoplasty in the present study.
Antell and Orsesk10 compared several techniques (more and less aggressive), applied on 8 pairs of monozygotic twins, and reported results similar to those presented here: 44% excellent results, 25% moderate results, and 31% poor results. Among other aspects, precise comparison with other studies and techniques was hampered by the use of different methodologies or analyses (absent in several publications5,6,9,28).
Chia30, in 2008, discussed the principles for midfacial treatment, and we believe that they can also be applied to lower-third facial surgery. Especially, for successful facial rejuvenation surgery, it is necessary to combine the following principles: wide detachment of the tissue to be lifted, direct approach to the structure being treated, attenuation of opposing muscular forces, and repositioning and securing to steady or rigid structures30. These principles were followed for extended cervicoplasty in this study to obtain long-lasting outcomes.
CONCLUSION
Especially in patients with excessive local sagging, the outcome of cervicoplasty is closely related to the combination of techniques used during the procedure, including platysma flap elevation and partial removal of subplatysmal fat. The cervicoplasty technique described herein is a valid alternative for the plastic surgeon, because it ensures a pleasant and natural outcome that is maintained over time.
REFERENCES
1. Jonhson JB, Hardley RC. The aging face. In: Converse JM, ed. Reconstructive plastic surgery. Philadelphia:WB Saunders;1964. p.1328-49.
2. Cardoso de Castro C. The changing role of platysma in face lifting. Plast Reconstr Surg. 2000;105(2):764-75.
3. McKinney P. The management of platysma bands. Plast Reconstr Surg. 1996;98(6):999-1006.
4. Miller TA. Face-lift: which technique? Plast Reconstr Surg. 1997; 100(2):501.
5. Benito J, Righesso R. Tratamento cirúrgico da região cervical associado a suturas de suspensão platismal com fios de politetrafluoroetileno. Rev Bras Cir Plást. 2007;22(4):202-8.
6. Patrocínio LG, Patrocínio JA. Cervicoplastia anterior. Rev Bras Otorrinolaringol. 2004;70(5):597-601.
7. Flores D, Sperli A, Freitas JOG, Lino AP. Avanços no estudo perfilométrico aplicados ao rejuvenescimento facial. Rev Soc Bras Cir Plást. 2000;15(3):67-78.
8. Knize DM. Limited incision submental lipectomy and platysmaplasty. Plast Reconstr Surg. 1998;101(2):473-81.
9. Labbé D, Franco RG, Nicolas J. Platysma suspension and platysmaplasty during neck lift: anatomical study and analysis of 30 cases. Plast Reconstr Surg. 2006;117(6):2001-7.
10. Antell DE, Orseck MJ. A comparison of face lift techniques in eight consecutive sets of identical twins. Plast Reconstr Surg. 2007;120(6):1667-73.
11. Millard DR, Pigott RW, Hedo A. Submandibular lipectomy. Plast Reconstr Surg. 1968;41(6):513-22.
12. Baker TJ, Gordon HL, Whitlow DR. Our present technique for rhytidectomy. Plast Reconstr Surg. 1973;52(3):232-6.
13. Feldman JJ. Corset platysmaplasty. Plast Reconstr Surg. 1990;85(3):333-43.
14. Pontes R, Pontes G. Ritidoplastia no homem. In: Mélega JM, Baroudi R, eds. Cirurgia plástica fundamentos e arte: cirurgia estética. Rio de Janeiro:Medsi;2003. p.87-98.
15. Cardoso de Castro C, Aboudib Jr. JHC, Carvalho S. Região cervical: tecido adiposo, SMAS, platisma. In: Mélega JM, Baroudi R, eds. Cirurgia plástica fundamentos e arte: cirurgia estética. Rio de Janeiro: Medsi; 2003. p.43-57.
16. Zins JE, Fardo D. The "anterior-only" approach to neck rejuvenation: an alternative to face lift surgery. Plast Reconstr Surg. 2005;115(6):1761-8.
17. Gryskiewicz JM. Submental suction-assisted lipectomy without platysmaplasty: pushing the (skin) envelope to avoid a face lift for unsuitable candidates. Plast Reconstr Surg. 2003;112(5):1393-405.
18. Pitanguy I. The round-lifting technique. Facial Plast Surg. 2000;16(3):255-67.
19. Castro CC. The anatomy of the platysma muscle. Plast Reconstr Surg. 1980;66(5):680-3.
20. Castro CC. Superficial musculoaponeurotic system-platysma: a continuous study. Ann Plast Surg. 1991;26(3):203-11.
21. Daher M. Lipofacelift: plástica facial com descolamento mínimo da pele. Rev Bras Cir Plást. 2009;24(4):479-87.
22. Connell BF. Cervical lifts: the value of platysma muscle flaps. Ann Plast Surg. 1978;1(1):32-43.
23. Marchac D, Brady JA, Chiou P. Face lifts with hidden scars: the vertical U incision. Plast Reconstr Surg. 2002;109(7):2539-51.
24. Gomes Filho BS, Fleishmann Jr HW, Caldellas AV, Colombo FG, Andrade AAM. Ritidoplastia com cicatriz periauricular. Rev Bras Cir Plást. 2009;24(4):488-96.
25. Castro CC. The value of anatomical study of the platysma muscle in cervical lifting. Aesthetic Plast Surg. 1984;8(1):7-11.
26. Neves RE, Vasconcelos ZAA, Vasconcelos JJA. Terço médio da ritidoplastia cervicofacial. In: Mélega JM, Baroudi R, eds. Cirurgia plástica fundamentos e arte: cirurgia estética. Rio de Janeiro: Medsi; 2005. p.25-42.
27. Aston SJ. Platysma muscle in rhytidoplasty. Ann Plast Surg. 1979;3(6):529-39.
28. Ellenbogen R, Karling JV. Visual criteria for success in restoring the youthful neck. Plast Reconstr Surg. 1980;66(6):826-37.
29. Castro CC, Aboudib JHC, Giaquinto MGC, Moreira MBL. Avaliação sobre resultados tardios em ritidoplastia. Rev Soc Bras Cir Plást. 2005;20(2):124-6.
30. Chia CY. Reposicionamento do terço médio na cirurgia da face: uma técnica simples de suspensão e de fixação. Rev Bras Cir Plást. 2008;23(2):71-4.
1. Plastic Surgeon, Member of the Brazilian Society of Plastic Surgery.
2. Plastic Surgeon, Specialist Member of the Brazilian Society of Plastic Surgery.
3. Trainee Doctor at the Service.
Corresponding author:
Daniel Nunes
Rua da Paz, 129 apto 1 - Jardim dos Estados
Campo Grande, MS, Brazil - CEP 79002-190
E-mail: viva@dermatoeplastica.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery)
Received: November 24, 2010
Accepted: March 15, 2011
Work performed at the private clinics of the first author, Campo Grande, MS, Brazil.
Article submitted for promotion to the status of full member of the BSPS.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license