INTRODUCTION
The recent concern about the safety of silicone implants has led many women to
seek the removal of their implants, even without rupture, contracture, or any
other complication in the breasts1-3.
Since their creation, silicone implants have gone through several moments of
discussion about their safety1,4,5. Currently, social networks have made it easier to share
information among patients2,4.
When public figures remove their implants and share their anxieties on social
media, these anxieties spread quickly and their followers begin to wonder
whether their implants are also compromising their quality of life2,3.
Publications about anaplastic giant cell lymphoma (BIA-ALCL) and the growing
belief in diseases that are difficult to diagnose, such as ASIA syndrome and
silicone disease, have generated fear in patients with silicone
implants3-5. Furthermore, the use of
large-volume implants in recent years has caused early ptosis and aesthetic
dissatisfaction even in relatively recent postoperative periods.
For all these reasons, many women have wanted to remove their implants, even if
this means that their breasts may no longer please them aesthetically.
On the other hand, many surgeons do not feel comfortable performing explantation
due to the lack of scientific evidence regarding the possible insecurities of
implants associated with the fear that the patient will not like the aesthetic
result after removing the implants3.
Magnetic resonance imaging (MRI) is a valuable resource for the diagnostic
evaluation of the breasts. It has a high sensitivity for identifying oncological
changes in breast tissue and is capable of showing changes in implants and the
peri-implant capsule6,7.
To perform the exam, the patient is positioned face down and the images are
captured in axial, sagittal, and coronal sections, preferably using contrast
(to
assess the health of the breast tissue)6.
Careful analysis of the axial and sagittal sections allows the surgeon to
determine whether there are areas of thinning of the breast tissue (with a
tendency to depression after removal of the implants), breast asymmetry,
differences in the positioning of the implants, in addition to showing changes
in the implant.
OBJECTIVE
This work aims to demonstrate how the systematic analysis of breast MRI images
can help in planning silicone explants, facilitating communication between
surgeon and patient, making the decision for explantation more conscious, and
favoring the chance of post-operative satisfaction. operative.
METHOD
The author has been using this resource in the pre-operative planning of patients
intending to undergo explantation since November 2020, in São Paulo, SP.
The patients showed no resistance to undergoing the MRI, even though it was an
uncomfortable and expensive exam. An analysis of the axial and sagittal MRI
sections was performed to assess the amount of tissue in each breast. These
images were presented to patients during the preoperative consultation so that
they could clearly understand how much the implant influences the size of their
breasts.
At the same time, post-operative photos of patients with similar characteristics
(size and implant placement plan, body type, weight, height, technique used in
post-explant reconstruction) were presented so that the patient could analyze
them more objectively, whether or not she would be satisfied with the aesthetics
of her breasts after explantation.
RESULTS
The patients demonstrated a high degree of understanding of the images presented,
both the MRI and the results photos of other patients, chosen based on
similarity with the case under analysis.
Regardless of whether or not they decided to proceed with the explant, all
patients felt more confident with their choice after this individualized
prediction of post-explant results. All those who chose to proceed with the
explant considered the result consistent with the expectations set in the
preoperative period (Figure 1A-F).
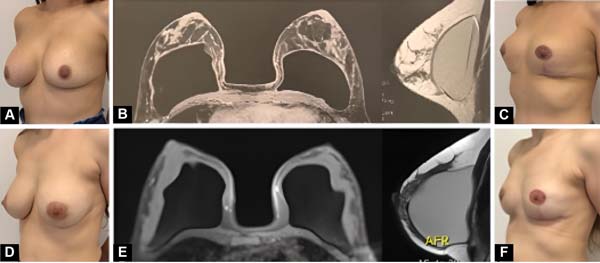
Figure 1 - A: IO pre-operative. Implants: 215 ml anteromuscular
14 years ago. Complaints: implant time, large breasts;
B: IO breast MRI; C: Post-operative
explantation with mastopexy (2 months). D: Preoperative
of MBGD, implants: 230ml anteromuscular 15 years ago. Complaint:
breast ptosis and implant time. E: MBGD breast MRI;
F: Post-operative explantation with mastopexy (2
months). Analyzing the MRI images, the preoperative expectation of
the MBGD patient was to have smaller breasts than the IO patient,
which was consistent with the result obtained.
Figure 1 - A: IO pre-operative. Implants: 215 ml anteromuscular
14 years ago. Complaints: implant time, large breasts;
B: IO breast MRI; C: Post-operative
explantation with mastopexy (2 months). D: Preoperative
of MBGD, implants: 230ml anteromuscular 15 years ago. Complaint:
breast ptosis and implant time. E: MBGD breast MRI;
F: Post-operative explantation with mastopexy (2
months). Analyzing the MRI images, the preoperative expectation of
the MBGD patient was to have smaller breasts than the IO patient,
which was consistent with the result obtained.
DISCUSSION
When the patient begins to consider permanently removing their implants,
insecurity arises regarding the possible aesthetic appearance of the breasts
after surgery. The fear of a bad result is fueled by doctors, friends, and
family, but even so, many patients follow their desire to explant seeking the
benefits of avoiding future surgeries and possible complications related to the
presence of a foreign body in the body.
Often, the aesthetic result is unsatisfactory, as the patient idealized a breast
similar to the one she had before the implant, but distortion of the breast
tissue and distension of the skin are inevitable.
As in any plastic surgery, aligning the expectation of results is essential for
patient satisfaction, and analyzing the breast MRI image together with
postoperative photos of other patients makes this dialogue more
intelligible.
It is important to make it clear that this is not a promise of results, but
rather a tool to facilitate communication between surgeon and patient and to
document the characteristics of the breast/implant relationship before
explantation.
To avoid errors in interpreting the amount of tissue in each breast, it is
important to compare MRI images respecting the implant placement plan, as the
expansion of breast tissue is greater when the implant is retroglandular than
when it is retropectoral.
It is worth noting that, to be coherent, comparisons must be made between similar
cases. Therefore, it is necessary to organize an image bank with data on the
implants (size, shape, placement plan) and patients (weight, height, technique
used in post-explant reconstruction) to make analyses more reliable and
reproducible.
CONCLUSION
Numerous factors can lead the patient to seek explantation, but, regardless of
the motivation, we cannot help but worry about the patient’s emotional capacity
to live well with her new self-image after the implants are removed.
The comparison of breast MRI images and postoperative results images brings
valuable information to align the expectations of patients seeking to remove
their implants, as it provides greater objectivity to the preoperative dialogue,
favoring understanding of the expected result and bringing greater clarity to
the decision for explantation.
REFERENCES
1. Calobrace MB. Elective Implant Removal and Replacement in
Asymptomatic Aesthetic Patients with Textured Devices. Plast Reconstr Surg.
2021;147(5S):14S-23S.
2. Magnusson MR, Cooter RD, Rakhorst H, McGuire PA, Adams WP Jr, Deva
AK. Breast Implant Illness: A Way Forward. Plast Reconstr Surg.
2019;143(3S):74S-81S.
3. Tanna N, Calobrace MB, Clemens MW, Hammond DC, Nahabedian MY,
Rohrich RJ, et al. Not All Breast Explants Are Equal: Contemporary Strategies
in
Breast Explantation Surgery. Plast Reconstr Surg.
2021;147(4):808-18.
4. Rohrich RJ, Bellamy JL, Alleyne B. Assessing Long-Term Outcomes in
Breast Implant Illness: The Missing Link? A Systematic Review. Plast Reconstr
Surg. 2022;149(4):638e-45e.
5. Rohrich RJ, Kaplan J, Dayan E. Silicone Implant Illness: Science
versus Myth? Plast Reconstr Surg. 2019;144(1):98-109.
6. Rossi AJRE, Kluthcovsky ACGC, Mansani FP. Comparison between
magnetic resonance imaging and ultrasonography as the best examination to
measure malignant breast tumors in surgical planning. Mastology.
2018;28(3):176-81.
7. Schmitt W, Coelho JM, Lopes J, Marques JC. O Papel da Radiologia na
Monitorização das Complicações Relacionadas com as Próteses Mamárias. Acta
Radiol Port. 2018;30(1):23-34.
1. Instituto de Cirurgia Plástica Santa Cruz, São
Paulo, SP, Brazil
Corresponding author: Patrícia Jackeline Maciel
Sales Rua Borges Lagoa, 1070, cj 62, Vila Clementino, São Paulo, SP,
Brazil, Zip Code: 04038-002, E-mail: patricia.cirurgia@gmail.com