ABSTRACT
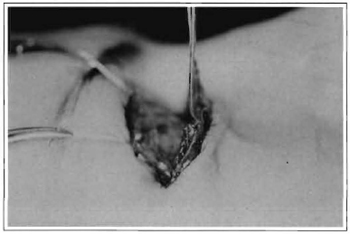
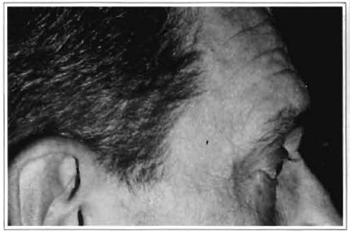
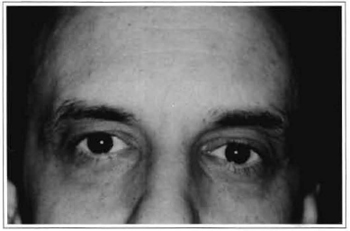
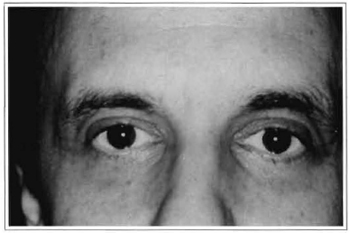
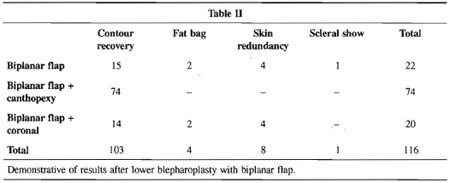
A byplanar flap, composed by cutaneous and muscular flaps with common musculocutaneous pedicle, is proposed to an adequate resection of the cutaneous and muscle excess in lower blepharoplasty. The byplanar flap allows to resect different quantities of the skin and muscle, in accordance to the palpebral deformity. It provides an appropriate vascular support, either for the cutaneous and for the muscular flap, through its common pedicle. The byplanar flap in association with the lateral canthopexy promotes the recovery of the lower eyelid muscular sling with the lateral canthus and lower eyelid support. The resection and fixation of the muscular portion of the biplanar flap elevate the skin and muscle flaps together, providing the adequate correction ofthe excess of both tissues, decreasing the occurrence of scleral show or ectropion.
Keywords: Biplanar flap; lower blepharoplasty; canthopexy