INTRODUCTION
Dentistry is a health science that aims to raise self-esteem and improve the patient’s
quality of life. These results can be achieved due to the healthy and aesthetic-functional
nature of certain dental procedures1. However, the search for procedures on the face with an aesthetic purpose has become
commonplace, which results in moral, ethical, and legal dilemmas concerning the area
of work of dentists.
In this way, limits of professional performance between different professions in the
health area, such as Medicine and Dentistry, have been the subject of debates and
even lawsuits when both professions do not reach an administrative pact mediated by
the councils of class. Thus, contestations with this approach have already occurred,
as is the case of the removal of the adipose body from the cheek (bichectomy) by dentists,
who must perform it exclusively for aesthetic and functional purposes2.
However, the emergence of new clinical procedures in different regions of the face
raises doubts and debates about the limits of the dentists’ area of expertise. This
area fits the intervention in the ear called “ear shut,” a procedure disclosed by
the dental class that promises the correction of protruding ears without surgery3.
OBJECTIVE
To survey the laws, regulations, and resolutions incumbent on the area of surgeon
dentists, as well as to discuss the limits and consequences of their extrapolation
from the perspective of the procedure propagated as “ear shut.”
CORRECTIVE PROCEDURES FOR PROTRUDING EAR IN MEDICINE AND DENTISTRY
Prominauris, popularly known as protruding ear, is one of the most common congenital anomalies
in the head and neck region, which genetic factors, environmental influences during
development, and auricular migration in the second trimester of pregnancy4,5 can cause.
It is characterized by anterior prominence of the ear, usually bilaterally, and although
it does not cause functional changes, it can affect the self-esteem of individuals,
the main reason for seeking corrective surgeries, as it can generate psychosocial
impacts, especially in childhood and adolescence, when the ridicule of physical characteristics
tends to have a negative influence, causing stress, anxiety, and difficulty in social
integration6.
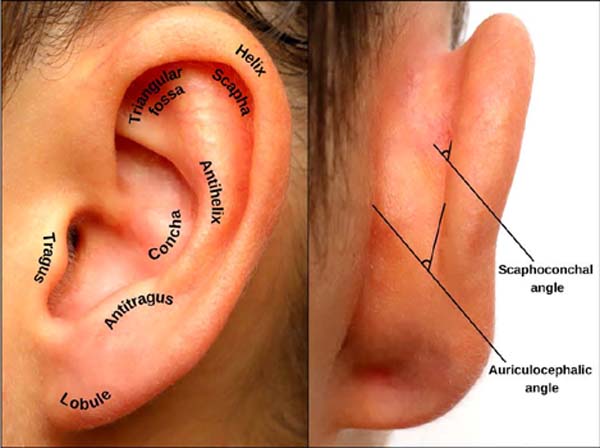
The ear is formed by anatomical regions directly related to the diagnosis of prominauris (Figure 1). Thus, there are three most frequent causes of protruding ears: underdevelopment
of the antihelix, which will increase the scaphoconchal angle; prominence of the concha,
which will increase the auriculocephalic angle; and lobe protrusion, and there may
also be an association between these causes7.
Figure 1 - Anatomical regions of the ear in frontal (on the left) and posterior (on the right)
norms.
Figure 1 - Anatomical regions of the ear in frontal (on the left) and posterior (on the right)
norms.
The auriculocephalic angle generally measures between 25° and 30°; and can reach more
than 40° of angulation. The scaphoconchal angle, of approximately 90°, can reach values
greater than 150° of angle8,9. That said, performing procedures in the ear region requires comprehensive knowledge
of its anatomy, encompassing superficial and deep anatomy, innervation, vascularization,
embryonic origin, and formation6.
In this context, otoplasty – plastic surgery of the ears - encompasses several techniques
for correcting the prominauris, and the choice of the appropriate technique depends on the analysis of several factors.
Therefore, the intervention aimed at the aesthetic correction of this condition must
be planned individually, and it is also possible to associate techniques to obtain
better results8.
In addition, the use of surgical techniques should consider the age at which the development
of the ear is completed, which occurs at around 6 years of age, so that from then
on, a surgical procedure to correct protruding ears can be performed, being this procedure
is performed under general anesthesia or sedation and local anesthesia, depending
on the patient’s age and level of compliance9.
As for the surgical techniques themselves, they vary according to their invasiveness,
tissue detachment, and incisions in strategic cartilage areas, with sutures that will
allow the creation of a new curvature9. On the other hand, less invasive techniques allow access to the cartilage through
small incisions to create weakening zones in the cartilage, where remodeling will
occur8. Although no gold standard technique exists, all have advantages and disadvantages,
converging on the same aesthetic goal10.
Closed otoplasty consists of a minimally invasive approach, which, based on the infiltration
and transcutaneous fixation of non-absorbable sutures, proposes the treatment of protruding
ears. The main intercurrences of the technique are the development of edema, ecchymosis,
recurrence, exposure of points, and asymmetry between the ears11.
Currently, in Dentistry, procedures related to the correction of protruding ears have
emerged as a novelty in the market, promising their execution without the need for
cuts, using only the suture, with transcutaneous stitches. This procedure, which became
known as “ear shut,” has been marketed as an innovative, fast, effective technique
that does not leave scars3.
The “ear shut” technique reproduces the steps of closed otoplasty, and no works in
the literature directly approach the subject with this nomenclature. Despite the promise
of results, Janis et al. (2005)12 state that non-surgical techniques for the correction of prominent ears demonstrated,
until that time, unsatisfactory results in most cases.
“EAR SHUT, “ TO DO OR NOT TO DO? LEGISLATIVE APPROACH
Properly and diligently caring for the health of their patients is the duty of every
dentist13. Abusive and harmful conduct that infringes this right is described in different
Brazilian legal norms14. Furthermore, in this sense, the professional practice of Dentistry must be practiced
with a high degree of zeal and with reliable scientific bases; in such a way, dentists
must know the procedures in depth, in addition to practicing them in the right measure
for each patient and their clinical condition15.
The World Health Organization defines health as a state of complete physical, mental,
and social well-being, and not just as the absence of disease or infirmity16. In this way, the prevention, recovery, and conservation of oral health is a basic
function of Dentistry, maintaining the integrity and proper functionality of the stomatognathic
system, restoring health, or even preventing the worsening of certain problems.
Dentists should not overlook moral, ethical, and legal issues during the execution
of any dental treatment or procedure since, in addition to the clinical act, this
also covers the professional-patient relationship in all its minutiae17. In addition to theoretical knowledge and clinical skills, professionals must be
well informed about their civil, criminal, ethical, and administrative obligations,
to which everyone is subject in this intimate relationship with their patients18.
Article 5 of the Federal Constitution enacted in 1988, item XIII establishes the right
to freedom of work or freedom to exercise any trade or profession, which can be defined
as the sovereignty of the human being to perform any work activity professionally,
provided that they are met professional qualifications established by law. As the
literalness of the constitutional provision suggests, there is the possibility that,
through the law, certain restrictions may be imposed on the exercise of any professional
activity19.
Already in item XXXIII of the same article, consumer protection is found as a constitutional
guarantee by stating that: “The State shall promote, as provided by law, consumer
protection.” To ensure the importance of health under the focus of the Federal Constitution,
article 6 also establishes health as one of the fundamental rights, inserted in the
title destined to the social order, which aims at well-being and social justice. Based
on this assessment, the State began to formulate social and economic policies aimed
at the specific protection of health19.
With the enactment of the Federal Constitution and in the wake of its articles, the
Consumer Defense Code was published, which covers the whole of society as a collective
of undetermined persons, in all their relations, being intended for the defense of
the person who acquires or uses product or service, materializing a consumption relationship.
In particular, article 2 defines the consumer as “every natural or legal person who
acquires or uses a product or service with a final recipient.” In this vein, any user
of dental services is a consumer to whom a service is provided, with a provider being
the professional who develops his activity for remuneration. Thus, it is emphasized
that the dental surgeon is a liberal profession, and the relationship with his patient
is consumerist nature20.
Preliminarily, it has to be pointed out that the patient will have the last word about
his own health. If it is not an emergency, only the doctor can decide whether or not
to implement a certain treatment, weighing risks and benefits. On this reasoning,
article 94 of the Brazilian Civil Code states that, in bilateral acts, the intentional
silence of one of the parties regarding a fact or quality that the other party has
ignored will constitute a willful omission, showing that without it, it would not
have been celebrated the contract. Thus, in understandable language, the patient must
be previously and duly clarified about his illness, the limits of the indicated treatment,
side effects, and possible complications21.
Focusing on the legal nature of civil liability, the Brazilian Civil Code, Law No.
10,406, of January 10, 2002, in articles 186, 187, 927, 949, 950, and 951, establishes
that the professional must have the corresponding academic training to the science
and ethics of the profession he embraced, exercising it within high scientific standards,
with prudence and expertise. Regular and recognized academies and institutions must
accept such training. It is never too much to emphasize that such articles have repercussions
on negligence, imprudence, or malpractice21.
When evaluating the criminal liability of dental surgeons in professional practice,
under the light of the Brazilian Penal Code, Decree-Law No. 2,848 of December 7, 1940,
it should be emphasized that this action is invasive par excellence, as it handles
a sharp instrument, blunt and cut blunt; which may cause various injuries and which
may lead to a complaint of a violation of article 129 and its sixth paragraph22:
“Decree-Law No. 2.848, of December 7,
1940. Penal Code
Chapter II
Bodily injuries
Bodily injuries
Art. 129. Offending the bodily integrity or health of others:
Penalty - detention, from three months to one year. (...) Culpable bodily injury
§ 6 If the injury is culpable:
Penalty - detention, from two months to one year. (...)”
In its article 132, the Penal Code is transparent in explaining that the exposure
of the life or health of another to imminent danger may lead to the penalty of detention,
from three months to one year, if the fact does not constitute a more serious crime.
This citation characterizes the crime of endangering life and health. It is imagined
when considering that the dental surgeon will act without malicious intent based on
his good faith. With this principle in mind, a criminal conviction will arise when
the professional’s guilt is demonstrated in his clinical practice. In this reasoning,
malpractice, imprudence, or negligence on the part of the professional should be characterized
since these are the elements that characterize guilt, and as a result, an injury was
produced during or as a result of their work22.
The same legal norm reinforces in article 282 that illicit professional activity is
foreseen and discusses that exercising, even if free of charge, the profession of
doctor, dentist, or pharmacist, without due legal authorization or exceeding its limits,
is subject to a penalty of detention, from six months to two years22. The lack of the appropriate title and the respective legal records characterizes
failure to comply with the legal authorization. As for the excess of limits mentioned
in the article’s writing, it is defined when the crime is committed by one of the
professionals referred to, performing typical acts of the profession in another field
of knowledge23.
“EAR SHUT” IN DENTISTRY: CURRENT ADMINISTRATIVE STANDARDS
In Brazil, Dentistry is regulated by Law No. 5081 of August 24, 1966, which dictates
dentists’ qualifications, skills, and prohibitions. In article 6, item I, the law
mentioned above states that it is the responsibility of dentists to practice all acts
relevant to Dentistry, whether the knowledge is acquired at the undergraduate or postgraduate
level. However, the Law does not detail dentists’ areas of expertise, with a description
of procedures or anatomical delimitations24.
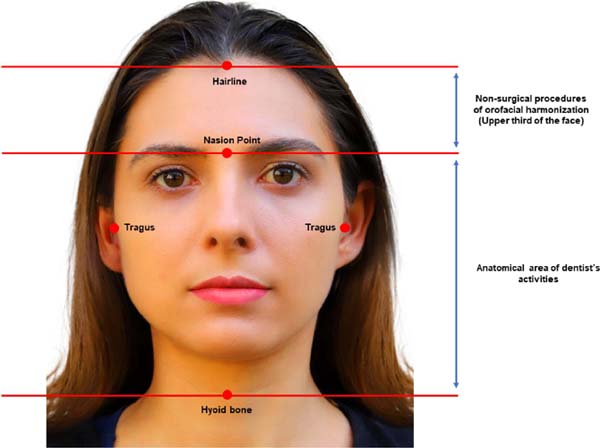
In this sense, in an attempt to resolve such doubts, Resolution No. 176/2016, published
by the Federal Council of Dentistry (CFO), in paragraph 1, discussed the use of botulinum
toxin in anatomical areas of clinical-surgical performance. These limits consist of
the upper portion of the hyoid bone, the lower portion of the nasal bones (nasion
point), and, laterally, the anterior portion of the tragus, encompassing what was
described in the regulation above as annex structures and the like. When in the condition
of non-surgical procedures, the upper third of the face is also included, from the
nasion point to the hairline. However, the anatomical delimitation presented in this
standard defines that the posterior part of the tragus is not an area of activity
for dental surgeons, in a way that it is not up to this professional to perform any
procedure for the treatment of protruding ears, whether surgical or not (Figure 2)25.
Figure 2 - Anatomical delimitation of the area of work of dentists according to Resolution No.
176/2016 of the Federal Council of Dentistry.
Figure 2 - Anatomical delimitation of the area of work of dentists according to Resolution No.
176/2016 of the Federal Council of Dentistry.
Following CFO Resolution No. 198/2019, orofacial harmonization was recognized as a
dental specialty, including botulinum toxin, facial fillers, percutaneous collagen-inducing
biomaterials, etc. intradermotherapy, biophotonic procedures, laser therapy, lipoplasty,
bichectomy, and liplifting. It can be seen in this agenda that no procedure is included
to intervene in the ears26.
Thus, to standardize, establish criteria and clarify the limits of dentists’ activities,
the CFO issued Resolution No. 230/2020, which prohibits the performance of certain
procedures in anatomical areas of the head and neck, listing, among these, otoplasty.
In addition, the same norm prohibits the publicity and publicity of non-dental procedures
unrelated to higher education in Dentistry21,27.
In addition to the anatomical region, as it has a strictly aesthetic nature, the “ear
shut” procedure directly affronts Resolution CFONº 63/2005, which in its article 48
provides for cosmetic surgery to be performed only by the medical class, with the
exception to those of an aesthetic-functionality of the stomatognathic apparatus29. Moreover, at this point, it is important to note that the Federal Council of Medicine
issued Resolution No. 2,272 of 2020, which states, in its 1st article, that it is the exclusive competence of the physician “the practice of surgery
and procedures with aesthetic and/or functional, with the exception, not exclusively,
of restorative surgery and with an aesthetic-functional purpose of the stomatognathic
apparatus”30, that is, indicating an interface of action with Dentistry, but in the case of the
“ear shut” procedure, there is no understanding in this norm of performance by a dental
surgeon.
1. Universidade de São Paulo. Faculdade de Medicina de Ribeirão Preto, Departamento
de Patologia e Medicina Legal, Ribeirão Preto, São Paulo, Brazil
2. Universidade de São Paulo. Faculdade de Odontologia de Ribeirão Preto, Departamento
de Odontologia Restauradora, Ribeirão Preto, São Paulo, Brazil
3. Universidade Federal da Paraíba, Hospital Regional da Asa Norte, Brasília, Distrito
Federal, Brazil
4. Universidade de São Paulo. Faculdade de Odontologia de Ribeirão Preto, Departamento
de Estomatologia, Saúde Coletiva e Odontologia Legal, Ribeirão Preto, São Paulo, Brazil
Corresponding author: Ricardo Henrique Alves da Silva USP – Faculdade de Odontologia de Ribeirão Preto. Área de Odontologia Legal. Av.
do Café, s/n, Bairro Monte Alegre, Ribeirão Preto, SP, Brazil. Zip Code: 14040-904
E-mail: ricardohenrique@usp.br