

Review Article - Year 2023 - Volume 38 - Issue 1
Complications in liposuction: systematic review
Complicações em lipoaspiração: revisão sistemática
ABSTRACT
Liposuction is among the most performed plastic surgery procedures in Brazil. According to data from the International Society of Aesthetic Plastic Surgery (ISAPS), 231,604 liposuctions were performed, 15.5% of all aesthetic procedures in the country in 2019. Adopting liposuction as a single procedure or adjunct to other cosmetic procedures stimulated its technical evolution from simple fat aspiration to more sophisticated body shaping. Thus, this review aimed to systematically evaluate the published data regarding the complications found in liposuction. A review was conducted using PubMed, SciELO, LILACS, Cochrane Library, SCOPUS, Web of Science, and gray literature databases, published between 2016 and 2021, using the descriptors "Liposuction" and "Complications." A total of 187 articles were found in the searched databases, of which 16 were selected according to the outcome "to assess safety through the prevalence of complications in liposuction as a single procedure and associated with other procedures such as abdominoplasty and fat grafting." We found a mortality rate ranging from 0 to 0.06 among all procedures and a predominance of venous thromboembolism, hematoma, seroma, and hyperpigmentation concerning all complications, being more common when liposuction is associated with other procedures. Therefore, through this review, it was possible to verify that liposuction as a single procedure has lower complication rates when compared to liposuction combined with other procedures.
Keywords: Lipoabdominoplasty; Lipectomy; Adipose tissue; Postoperative complications; Intraoperative complications
RESUMO
A lipoaspiração está entre os procedimentos da cirurgia plástica mais realizados no Brasil. Segundo dados da International Society of Aesthetic Plastic Surgery (ISAPS), foram totalizadas 231.604 lipoaspirações, 15,5% dentre todos os procedimentos estéticos realizados no país em 2019. A adoção da lipoaspiração como procedimento único ou coadjuvante a outros procedimentos cosméticos estimulou sua evolução técnica da simples aspiração de gordura para uma modelagem corporal mais sofisticada. Desse modo, esta revisão objetivou avaliar sistematicamente os dados publicados em relação às complicações encontradas na lipoaspiração. Foi realizada uma revisão utilizando os bancos de dados PubMed, SciELO, LILACS, Cochrane Library, SCOPUS, Web of Science e grey literature, publicados entre os anos de 2016 e 2021, através dos descritores "Liposuction" and "Complications". Foram encontrados 187 artigos nas bases de dados pesquisadas, dos quais 16 foram selecionados de acordo com o desfecho "avaliar a segurança através da prevalência de complicações na lipoaspiração como procedimento único e a associada a outros procedimentos como abdominoplastia e lipoenxertia". Encontramos uma taxa de mortalidade que varia de 0 a 0,06 dentre todos os procedimentos e um predomínio de tromboembolismo venoso, hematoma, seroma e hiperpigmentação em relação a todas as complicações, sendo mais encontradas quando a lipoaspiração é associada a outros procedimentos. Logo, por meio desta revisão foi possível constatar que a lipoaspiração como procedimento único apresenta menores taxas de complicações quando comparada à lipoaspiração combinada com outros procedimentos.
Palavras-chave: Lipoabdominoplastia; Lipectomia; Tecido adiposo; Complicações pós-operatórias; Complicações intraoperatórias
INTRODUCTION
Liposuction is among plastic surgery’s most common aesthetic procedures and is increasingly combined with other procedures1,2. Introduced by Illouz in the early 1980s, the liposuction technique underwent a major transformation to reach its current state3. In Brazil, according to data from the International Society of Aesthetic Plastic Surgery (ISAPS)4, this is the most performed aesthetic surgical procedure, totaling 231,604 (15.5%) among all procedures in 2019.
Adopting liposuction as a single procedure or adjunct to other cosmetic procedures stimulated its technical evolution from simple fat aspiration to more sophisticated body shaping5. In line with the growing demand for safety standards for cosmetic treatments, medical societies have developed guidelines and consensus to guide decisions and define safety criteria for procedures. Therefore, the discussion about liposuction, one of the most performed procedures, is at the forefront 6,7.
Regarding the risk factors that can trigger complications related to liposuction, it was observed that errors in patient selection are key factors in the outcome, pointing to prior evaluation as one of the pillars of the success of the procedure, contraindicating liposuction in patients with cardiovascular disease and severe pulmonary disorders, severe coagulation disorders, including thrombophilias, and during pregnancy, in addition to patients with diabetes and smoking 8,9.
Concerning complications, the incidence after liposuction ranges from 0% to 10%, even with inconsistent data reported between different specialties, such as Plastic Surgery and Dermatology, making the accurate assessment of the risk profile of liposuction a challenge10. Regarding mortality, a study of 25 years of experience with 26,259 patients11 observed a rate of 0.01%. Accordingly, ISAPS published a survey in which a mortality rate of 19.1 was reported for every 100,000 liposuctions4.
In line with the growing demand for safety standards for cosmetic treatments, medical societies have developed guidelines and consensus to guide decisions and define safety criteria for procedures. Therefore, this article addresses an update of knowledge about liposuction and its complications and compares the surgery with other procedures such as abdominoplasty and fat grafting.
OBJECTIVE
This review aimed to systematically review the data published in the last 5 years regarding the complications encountered in liposuction as a single and combined procedure.
METHOD
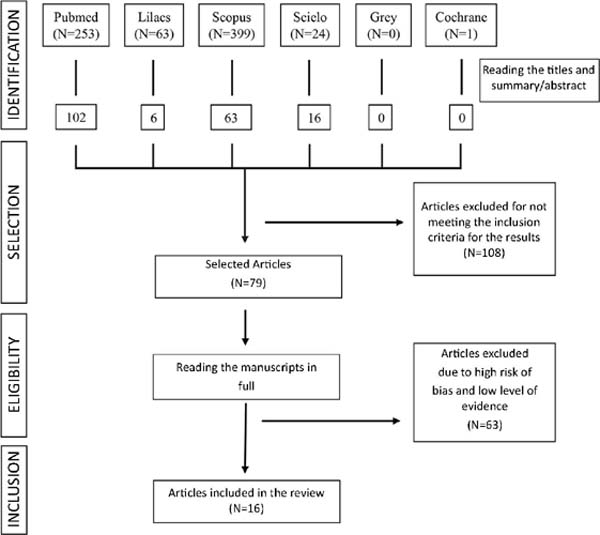
This is a systematic, descriptive literature review based on the search for accessible studies, using the PRISMA12 guideline, in which the following strategy was adopted: 1) elaboration of a guiding research question for the search strategy; 2) variety of sources for the location of studies; 3) definition of inclusion and exclusion criteria and 4) evaluation of the methodological quality of the included articles.
The survey of articles was carried out in May 2021 using the databases: PubMed (US National Library of Medicine/National Institute of Health), SciELO (Scientific Electronic Library Online), LILACS (Latin American and Caribbean Information Center in Health Sciences), Cochrane Library, SCOPUS, Web of Science and gray literature, published between 2016 and 2021.
Using the PICO strategy, which represents an acronym for Patient, Intervention, Comparison, and “Outcomes” (outcome), the following guiding question, “What are the complications of the liposuction procedure?” was elaborated. The descriptors related to the investigated themes were crossed after searching for synonyms using the MeSH (Medical Subject Headings) and DeCS (Health Sciences Descriptors) tools, so the descriptors were defined: ((“Liposuction” OR “Lipectomies” OR “Aspiration Lipectomies” OR “Lipectomies, Aspiration” OR “Lipectomy, Aspiration” OR “Aspiration Lipolysis” OR “Lipolysis, Aspiration” OR “Lipectomy, Suction” OR “Lipectomy, Suction” OR “Suction Lipectomies” OR “Lipolysis, Suction” OR “Liposuctions” OR “Lipoplasties” OR “lipectomy” OR “Aspiration Lipectomy” OR “Suction Lipectomy” OR “Lipoplasty” OR “Suction Lipolysis”) AND (“Postoperative Complications” OR “Complication, Postoperative” OR “Complications, Postoperative” OR “Postoperative Complication” OR “Intraoperative Complications” OR “Perioperative Complication” OR “Surgical Injury”).
At this point in the search, broader terms were intentionally used to identify more productions, preventing any important study from being excluded from the survey. Afterward, the title and abstract were analyzed to select studies evaluating the population, the intervention of interest, and at least one defined outcome. Case reports and case series were removed due to their low level of evidence. In addition, duplicate articles and studies not written in English, Spanish, or Portuguese were excluded.
Therefore, regarding eligibility, the articles were read in full, and studies with a high risk of methodological bias were excluded, using the Risk Of Bias 2 (RoB 2) tool, a revised tool to assess the risk of bias in randomized studies. The outcomes defined for this research were: To assess the degree of safety through the prevalence of complications in liposuction in a single procedure and combined with other procedures such as abdominoplasty and fat grafting (Figure 1).
RESULTS
Types of study
A total of 187 articles were found in the researched databases, of which 16 were selected for data use, with their interpretation and synthesis. Among the 16 studies, five were literature reviews, seven were cohort studies, and four were cross-sectional.
In addition, regarding the outcome of the articles included in the study, four analyzed the complications of liposuction as a single procedure, eight discussed the complications of liposuction combined with other procedures such as abdominoplasty and fat grafting, and four studies developed a comparison between safety and the level of complications in isolated and combined liposuction (Table 1).
| Systemic and local complications in (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Technique | Number of patients | Mortal age | Venous Thromboembolism (VTE) | Blood loss | Surgical site infection | Seroma | Hyperpigmentation | Irregular Contour | Bruise | Others | |
| Xia et al., 20191 | Isolated and combined liposuction | 14,061 | - | 0.2 | Infection, dehiscence wound and | fat necrosis: 5.6 | 4.1 | 0.7 | 0.8 | |||
| Halk et al., 2019*6 | Isolated liposuction | - | up to 0.05% every 1000 surgeries | - | - | - | - | - | - | - | Combined procedures had an almost 5 times greater risk of serious adverse events than isolated procedures, especially for VTE and infection. | |
| Wu et al., 2020*14 | Isolated and combined liposuction | - | 0.01 in 26,259 patients | 0.03% in 1,000 patients | - | - | 2% in 451 patients | - | 9% in 11,016 patients | - | - | |
| Sozer et al., 201815 | Combined liposuction | 1,000 | 0.01 | 1.5 | - | 1.5 | 19 | - | - | 0.40 | - | |
| Vieira et al., 201816 | Combined liposuction | 9,638 | 0.06 | 0.46 | 0.24 | 1.83 | 3.6 | - | - | 0.84 | - | |
| Montrief et al., 2020*17 | Isolated and combined liposuction | - | - | The incidence of deep vein thrombosis (DVT) and pulmonary embolism (PE) in liposuction is less than 1%. However, there is a marked increase in the incidence of DVT when liposuction is performed, combined with abdominoplasty | - | - | - | - | - | 3-15 | Visceral perforation: 0.00014 | |
| Kaoutzanis et al.,201718 | Isolated and combined liposuction | 31,010 Isolated liposuction (11,490-37.1%) and combined (19.520 -62.9%) | 0.06 isolated 0.6 combined | - | 0.1 isolated 0.7 combined | - | - | - | 0.15 isolated 0.60 combined | Pulmonary disorders: 0.1 isolated 0.2 combined | ||
| Campos et al., 201819 | Isolated and combined liposuction | 30 | - | - | Drop in hemoglobin between 2 - 6g/dl, with an average of 3.0lg/dl corresponding to 22.16% of the preoperative hematocrit operative | - | - | - | - | - | 50% had dizziness, dyspnea, tachycardia, orthostatic hypotension | |
| Vend ramin et al., 201920 | Combined liposuction | 16 | - | - | Post-surgical Hb values between 8.92 g/dL and 10.4 g/dL. The percentage reduction in Hb between the beginning and the end of the surgery averaged 19.7% | - | - | - | - | - | - | |
| Restifo 201921 | Combined liposuction | 304 | - | - | - | 4.27 | 14.38 | - | - | 0.9 | 5.92 of the patients had fat necrosis | |
| Al Dujaili et al., 201822 | Isolated liposuction | 15,336 | - | 0.34-0.6 | - | - | 0.17 - 1.6 | 0.02 | 0.26-2.1 | - | - | |
| Husain et al., 201923 | Isolated liposuction | 50 | - | - | - | - | 10 | two | 12 | - | - | |
| Gould et al., 201824 | Combined liposuction | 619 | - | - | - | - | 2.16 with drain 9.17 without drain | - | - | - | - | |
| Massignan 201925 | Combined liposuction | 76 | - | - | - | - | - | 2.67 | - | - | - | |
| Weissler et al., 202126 | Isolated liposuction | 120 | - | - | - | - | - | - | - | Hematomas in patients who received ATX were significantly smaller than in patients who did not (1.6 / 10 vs. 2.3/10) | - | |
| Bertheuil et al., 201727 | Isolated liposuction | 25 | - | - | - | 8 | - | - | - | - | 40% presented dehiscence of the surgical wound, and 8% had some degree of necrosis of fat | |
* In the studies by Wu, Halk, and Montrief, there were no specifications about the number of patients undergoing the procedures. N°., number; Hb. Hemoglobin; ATX, Trenaxamic Acid; VTE, Venous Thromboembolism; g/dL, grams per deciliter.
Risk factors
Regarding the procedure’s risks, patients with cardiovascular, pulmonary, diabetic, and vascular diseases face a higher risk. In addition to these comorbidities, smoking is a risk factor for surgical complications13,14.
Mortality
Among the included studies regarding liposuction as a single procedure, the review by Wu et al. in 202014 indicated a mortality rate of 0.01% in approximately 26,000 patients. In another review, Halk et al., in 20196, demonstrated a variation of 0 to 0.55 deaths per 1000 procedures. On the other hand, when we look at liposuction combined with abdominoplasty, two observational studies in 201815,16 indicated 0.01% of deaths in 1,000 and 0.06% in 9,638 patients, respectively.
Venous thromboembolism (VTE)
There is an agreement in the articles published by Montrief et al.17 and Wu et al.14 that venous thromboembolism is the main cause of death after combined or isolated liposuction, responsible for up to 21% of postoperative deaths17.
In the liposuction procedure combined with other techniques, the mean chance of VTE was 0.56%, numbers that ranged from 0.2% in 1,406 patients, found by Xia et al.1, and 0.46%, in 9,638 patients evaluated by Vieira et al.16, to 1.50% patients undergoing abdominoplasty with liposuction by Sozer et al.15. Concerning liposuction as a single procedure, the number of patients with VTE is five times lower, 0.06%, as indicated by Kaoutzanis et al.18, in 31,010 patients, of which 37.1% underwent only liposuction and 62.9% combined with other procedures.
Blood loss and anemia
In a prospective study of 30 post-surgical liposuction patients conducted by Campos in 201819, a drop in hemoglobin (Hb) between 2 and 6g/dl was observed, with a mean of 3.01g/dl, corresponding to 22.16 % of preoperative hematocrit, in which 15 patients complained of symptoms such as dizziness, dyspnea, tachycardia, and orthostatic hypotension. In addition to this study, Vendramin et al.20 observed Hb in 16 patients at the end of surgery and at hospital discharge, with values of 10.4g/dl and 8.92g/dl, respectively. The percentage reduction in Hb between the beginning and the end of the surgery averaged 19.7%, and in none of the cases observed, did the patients require a blood transfusion in the postoperative period.
Surgical site infection
Restifo21 reported infection in 13 of 304 patients (4.27%) who associated abdominoplasty with liposuction. Sozer et al.15 and Vieira et al.16 also analyzed the two associated procedures and described 1.5% of surgical site infections in 1,000 procedures and 1.83% in 9,638 patients, respectively. Kaoutzanis et al.18 showed inferior results: in 19,520, only 0.7% of patients had this complication.
Regarding isolated liposuction, the literature review by Al Dujaili et al.22 points to values that vary between 0.34% and 0.6% in approximately 15 thousand procedures. In addition to this study, Kaoutzanis et al.18 compared liposuction versus lipoabdominoplasty and reported infection rates of 0.1% in 11,490 and 0.7% in 19,520 procedures; finally, Xia et al., in 20191, combined the results of surgical wound infection, wound dehiscence, and fat necrosis, finding a rate of 5.6% in 14.61 patients.
Seroma
According to Vieira et al.16, 3.6% of 9,638 patients had this complication when undergoing lipoabdominoplasty, whereas Restifo, in 201921, found 14.38% of 723 patients undergoing abdominoplasty associated with sub-Scarpa lipectomy. The study by Sozer et al.15 associated abdominoplasties with circumferential liposuction and pointed out that seroma was presented by 190 out of 1000 patients. The meta-analysis by Xia et al.1 showed the occurrence of seroma in 4.1% of 14,000 patients undergoing lipoabdominoplasty. In the review by Wu et al.14, a 2% prevalence of seroma in liposuctions was observed; the cohort by Husain et al.23, with 50 patients, inferred a 10% rate of appearance of seroma in patients undergoing liposuction. Gould et al., in 201824, indicated in 619 lipoabdominoplasties the appearance of 2.16% of seromas in procedures using a drain and 9.17% when there was no use of a drain in the surgery.
Hyperpigmentation
Complications are described in only two analyzed articles. The review by Al Dujaili et al.22 found 0.02% of this complaint in approximately 15,000 patients who underwent liposuction as a single procedure; in a prospective study by Massignan25, in which liposuction associated with VASER (Vibration Amplification of Sound Energy at Resonance) was performed in 76 patients, two (2.67%) had skin hyperpigmentation, and one (1.31%) presented a thermal lesion at the insertion site of the device.
Irregular outline
Three literature reviews described irregular outlines. Wu et al.14 pointed out that contour irregularity is the most common complication of liposuction. Up to 9% of patients may report soft tissue depressions or elevations, skin panicles, folds, or wrinkles. Accordingly, Husain et al.23 indicate that the least severe and most prevalent complication was irregular contour, observed in 12% of 50 patients who underwent liposuction with a “six-pack” abdomen design (“abdominal etching”).
The review by Al Dujaili et al.22 does not indicate the number of patients with this complication; however, it demonstrates that surface irregularities, such as depressions or skin undulations, can be caused by excessive liposuction, superficial suction, pre-existing adhesions, redundant skin or inadequate compression. Patients with pre-existing cellulitis, poor skin elasticity, and scarring are more likely to have surface irregularities. Preventive measures include setting the maximum vacuum pressure to 250 to 400mmHg and aspirating the surface layer under low pressure21.
Bruise
Hematoma was one of the most common complications in the literature related to liposuction and its combinations. The cohort carried out by Kaoutzanis et al., in 201718, with 31,000 patients, compared single and combined procedures, finding a prevalence of 0.15% in 11,490 liposuctions and 0.60% in 19,520 liposuctions combined with other procedures.
Hematoma as a complication of lipoabdominoplasty was described by Sozer et al.15, Vieira et al.16, and Xia et al.1, resulting in 0.40% in 1,000, 0.90% in 1,500 and 0.8% in 14,000 procedures, respectively. Furthermore, in work by Weissler et al., in 202126, with 120 patients divided into two equal groups, there was a chance of bruising of 2.3/10 among patients who did not use tranexamic acid infiltration during the procedure and of 1.6/10 in which there was infiltration, showing a statistically significant difference. In the literature review by Montrief et al.17, a prevalence variation of 3 to 15% of this complication in lipoabdominoplasty was observed.
Other complications
Bertheuil et al.27 indicated that in 25 lipo body-lift procedures, there were 10 cases of surgical wound dehiscence treated with secondary intention healing and two cases of fat necrosis. The study carried out by Restifo21 evaluated 304 sub-Scarpa lipectomies that indicated approximately 5% of cases of fat necrosis. The literature review by Montrief et al.17 indicated visceral perforation as the second most common cause of mortality after liposuction, with ileal perforation being the most common site, followed by perforation of the jejunum, spleen, cecum, transverse colon, and sigmoid. It is important to emphasize that risk factors for visceral perforation during liposuction are: morbid obesity, previous surgical scars, and abdominal wall hernias.
DISCUSSION
According to the results obtained, we found evidence that liposuction as an isolated procedure tends to demonstrate a lower chance of complications when compared to procedures combined with liposuction and abdominoplasty or liposculpture.
In addition, the evidence found demonstrated that complications with higher incidence rates, such as hematomas, seromas, and contour irregularities, have less serious repercussions for patients. On the other hand, more serious complications that require hospitalization for treatment, for example, VTE, visceral perforation, and surgical site infections, are less common.
Likewise, a review carried out in 2016 byAlmutairiet al.28 showed the same early complications found in the present study, also with a low percentage of prevalence (5-15%), with emphasis on surgical wound dehiscence and late healing of the wound, as the most common, followed by the formation of seromas, hematomas, and wound infections. This finding suggests that there have been no major variations in liposuction complications over the past 10 years; on the contrary, maintaining safety and optimizing patient outcomes.
Some limitations must be considered. Not all liposuction safety factors have been reviewed, for example, the type of anesthesia used, immediate postoperative follow-up by a multidisciplinary team, the ideal composition of the humectant solution, time before starting liposuction, details about techniques such as the exact type of cannula, depth and body location of liposuction, and patient selection criteria. Furthermore, the meta-analysis could not be conducted due to heterogeneity between studies to meet all interest criteria.
Certain points about combined liposuction or not still require further clarification, such as the amount of liposuctioned content and its possible relationships with more serious complications in patients, in addition to understanding the importance of the multidisciplinary team in the immediate postoperative period and its impact on the appearance of intraoperative and postoperative complications.
CONCLUSION
Liposuction is a safe procedure with a low rate of complications. Liposuction as a single surgery has lower rates of complications than liposuction combined with other procedures, such as lipoabdominoplasty and fat grafting. The wide range of methods to aspirate subcutaneous fat allows for an optimal individual treatment plan, considering the correct indications. Thorough surgeon training and in-depth knowledge of possible complications are essential, as although liposuction is often offered as a minor, harmless surgery, it is a complex procedure. Therefore, more long-term studies should be carried out to consolidate the procedure’s understanding and safety further.
1. Universidade Do Estado do Pará, Departamento de Cirurgia, Belém, Pará, Brazil
2. Universidade Federal do Amapá, Departamento de Cirurgia, Macapá, Amapá, Brazil
3. Centro Universitário Metropolitano da Amazônia, Departamento de Cirurgia, Belém,
Pará, Brazil
4. Universidade Federal do Pará, Departamento de Cirurgia, Belém, Pará, Brazil
Corresponding author: Luiz Fernando Lima Barros Rua Municipalidade 985, sala 2005. Ed Mirai Office, Umarizal, Belém, PA, Brazil. Zip code: 66055-200 E-mail: lfbcirurgiaplastica@gmail.com





 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter