

Original Article - Year 2023 - Volume 38 -
Frailty syndrome, feelings of impotence and functional capacity in elderly patients with venous ulcers
Síndrome de fragilidade, sentimento de impotência e capacidade funcional em idosos portadores de úlcera venosa
ABSTRACT
Introduction: Chronic venous ulcers have a negative impact on the physical, psychic, and social domains, affecting the quality of life of patients, especially the elderly. This study aimed to assess frailty, functional capacity, and feelings of helplessness in older people with venous ulcers.
Method: 112 older people were divided into two groups according to the presence or absence of venous ulcers. All patients were interviewed using the Edmonton Frail Scale (EFS), Health Assessment Questionnaire-20 (HAQ-20), and the Impotence Feelings Measurement Instrument (IMSI) from May 2017 to August 2018.
Results: Regarding the EFS score, 76.8% of patients with venous ulcers were classified as vulnerable and frail, compared to 28.6% of patients in the group without ulcers. Scores on the HAQ-20 showed statistically significant differences between groups in all categories of the instrument, indicating that older people with venous ulcers had reduced general functional capacity compared to older people without ulcers. The mean IMSI score was 41.2 for the group with venous ulcers and 33.4 for the group without ulcers.
Conclusion: Venous ulcers had a negative impact on functional capacity and increased frailty and feelings of powerlessness in the elderly.
Keywords: Aged; Frail elderly; Aging; Varicose ulcer; Quality of life
RESUMO
Introdução: Úlceras venosas crônicas exercem impacto negativo nos domínios físico, psíquico e social, afetando a qualidade de vida de pacientes, especialmente os idosos. O objetivo deste estudo foi avaliar o nível de fragilidade, capacidade funcional e sentimento de impotência em idosos com úlcera venosa.
Método: Um total de 112 idosos foram distribuídos em dois grupos de acordo com a presença ou ausência úlcera venosa. Todos os pacientes foram entrevistados utilizando-se os questionários Edmonton Frail Scale (EFS), Health Assessment Questionnaire-20 (HAQ-20) e o Instrumento de Medida de Sentimento de Impotência (IMSI) no período de maio de 2017 a agosto de 2018.
Resultados: Em relação à pontuação na EFS, 76,8% dos pacientes com úlcera venosa foram classificados como vulneráveis e frágeis, em comparação a 28,6% dos pacientes do grupo sem úlcera. Pontuações no HAQ-20 mostraram diferenças estatisticamente significantes entre os grupos em todas as categorias do instrumento, indicando que idosos com úlcera venosa apresentavam redução da capacidade funcional geral em comparação aos idosos sem úlcera. A pontuação média para o IMSI foi de 41,2 para o grupo com úlcera venosa e 33,4 para o grupo sem úlcera.
Conclusão: Úlceras venosas causaram impacto negativo na capacidade funcional e aumento de fragilidade e sentimento de impotência nos idosos.
Palavras-chave: Idoso; Idoso fragilizado; Envelhecimento; Úlcera varicosa; Qualidade de vida
INTRODUCTION
Since the middle of the last century, significant changes have been taking place in the demographic and health patterns of the world’s population, leading to significant growth in the elderly population, many of whom have some chronic diseases. It is estimated that, in 2025, Brazil will have the sixth largest elderly population in the world, around 32 million people1,2,3,4.
The negative impact of chronic venous ulcers on quality of life is particularly reported concerning pain, physical function, and mobility domains5,6,7,8. Depression and social isolation are also reported as manifestations resulting from the presence of venous ulcers7,8,9,10,11.
Most older people with venous ulcers feel frustrated, impotent, lose faith in the treatment and feel vulnerable, unable to carry out daily activities8,12,13,14,15, culminating in growing dependence, whose evolution can change and even be prevented or reduced if there is adequate environment and assistance11,16. Dependence can also be considered as a state in which people find themselves lacking or losing autonomy (physical, psychological, social) and needing help to carry out basic activities. It is a serious health problem that interferes with the quality of life of the elderly and their caregivers14,17.
When evaluating the functional capacity of older people with venous ulcers, it is observed that patients have a reduced capacity for self-care and meeting basic needs6,9,12. Functional capacity or limitation can be defined as the individual’s ability to maintain physical and mental capacities in basic and instrumental activities15,16.
The frailty in the elderly with venous ulcers becomes chronic, resulting in a feeling of impotence, low self-esteem, and self-image16,17,18,19.
Most studies about the frailty syndrome and elderly individuals with chronic diseases are justified because this condition makes this population more prone to progressive reduction in functional capacity, repeated hospitalizations, and greater demand for health services at different levels17,18,20,21,22,23,24.
In this sense, the frailty syndrome acquires importance as a target for investigations and interventions because of the impact on elderly individuals, especially those with venous ulcers, their families, and society as a whole. No national or international literature studies evaluated the frailty syndrome and its consequences (decreased functional capacity in activities of daily living and instrumental activities of daily living, feelings of impotence and its consequences) in elderly patients with venous ulcers and who also consider pre-frail individuals.
OBJECTIVE
Assess the level of frailty, feelings of powerlessness, and functional capacity in older people with venous ulcers.
METHOD
Analytical, cross-sectional, descriptive, controlled study, approved by the Institutional Ethics Committee, on opinion: 2,939,899, whose data were collected at the Federal University of São Paulo from March 2017 to August 2018.
Two groups of participants over 60 were established: with venous ulcer and without ulcer, each group with 56 patients.
The inclusion criteria for both groups were: 60 years or older and being literate, adding an ankle/arm index between 1.0 and 1.4 for the group with venous ulcers. The non-inclusion criteria for both groups were: mixed or arterial ulcer, sequelae of stroke, or lower limb amputation.
Data were collected through interviews using self-administered and public domain questionnaires, including a form for collecting demographic data, the Edmonton Frail Scale (EFS) instrument18, the Health Assessment Questionnaire-20 (HAQ-20)21, and the Instrument for Measuring Feelings of Powerlessness (IMSI)15.
The EFS was chosen to assess whether individuals in both groups were frail or pre-frail. This instrument assesses the level of frailty in nine domains represented by 11 items, including cognition, general health status and health description, functional independence, social support, medication use, nutrition, mood, continence, and functional performance. The scoring ranges for frailty level analysis are 0-4, no frailty; 5-6, apparently vulnerable; 7-8, mild frailty; 9-10, moderate frailty; 11 or more, severe frailty, with a maximum score of 1718.
The HAQ-20 consists of 20 questions divided into eight categories representing functional activities – getting dressed, getting up, eating, walking, hygiene, reaching, gripping, and other activities. The patient’s responses are measured on a scale ranging from zero (no difficulty) to three (unable to do). The final score is calculated by the sum of the components divided by 8 and can be classified as HAQ-20 from 0 to 1, mild deficiency; HAQ-20 >1 to 2, moderate deficiency; and HAQ-20 >2 to 3, severe deficiency21.
The IMSI consists of 12 Likert-type questions with a five-point frequency ranging from “never” to “always.” In this scale, the following scores are assigned to items that mean the presence of a feeling of powerlessness: 1 = never; 2 = rarely; 3 = sometimes, 4 = often, and 5 = always, totaling a maximum of 60 points. The 12 questions are divided into three domains: the ability to perform a behavior (Cronbach’s alpha = 0.845), the perceived ability to make decisions (Cronbach’s alpha = 0.834), and the emotional response to controlling situations (Cronbach’s alpha = 0.578). The scores are added by domain and total score; the higher the score, the more intense the feeling of powerlessness15.
Data were entered and analyzed using the SPSS-8.0 statistical program (SPSS Inc., Chicago, IL, USA). Pearson’s chi-square test was used to assess the homogeneity of responses, comparing the two study groups, with a significance level equal to 0.05 (p<0.05). Comparison between groups was performed using the Mann-Whitney test. Spearman’s correlation test was applied to assess the correlation of continuous variables with semicontinuous variables.
RESULTS
The sample consisted of 112 patients with the following sociodemographic characteristics: 68 (60.7%) were female, 56 (50.0%) had venous ulcers, 64 (57.1%) were 70 years old or older, 43 (38.4%) could read, and write; 88 (78.6%) were retired; 45 (40.2%) were married, 40 (35.7%) lived with family members, 100 (89.3%) used medication, 60 (53.6%) had an adequate body mass index (BMI), 76 (67.9%) did not practice physical activity, and 84 (75.0%) suffered a fall in the 30 days prior to the interview.
According to the mean overall EFS score by group (Table 1), patients with venous ulcers were considered vulnerable (mean EFS = 6.46) in contrast to patients without ulcers who were identified as not vulnerable (mean EFS = 3.38), with a statistically significant difference between groups (p=0.001).
| Group | EFS - Overall Score | p-Value | |||
|---|---|---|---|---|---|
| n | Mean | Median | SD | ||
| With ulcer | 56 | 6.46 | 6.0 | 3,086 | |
| No ulcer | 56 | 3.38 | 3.0 | 2,253 | 0.001* |
| Total | 112 | 4.92 | 5.0 | 3.105 | |
Regarding the EFS score by category, patients in the ulcer group were concentrated in the “apparently vulnerable” and “mildly frail” categories, while the group without ulcers was concentrated in the “non-frail” category. Table 2 indicates that 76.8% (n=43) of patients with venous ulcers were classified as vulnerable and fragile, compared to 28.6% (n=16) of patients in the group without ulcers, with a statistically significant difference between groups (p=0.001).
| Level of Fragility | Group | p-Value | |||||
|---|---|---|---|---|---|---|---|
| With ulcer | Without ulcer | Total | |||||
| n | % | n | % | n | % | ||
| Does not present Fragility | 13 | 23.2 | 40 | 71.4 | 53 | 47.3 | |
| Apparently Vulnerable | 16 | 28.6 | 11 | 19.6 | 27 | 24.1 | 0.001* |
| Mild frailty | 12 | 21.4 | 4 | 7.1 | 16 | 14.3 | |
| Moderate frailty | 11 | 19.6 | 0 | 0.0 | 11 | 9.8 | |
| Severe frailty | 4 | 7.1 | 1 | 1.8 | 5 | 4.5 | |
| Total | 56 | 100 | 56 | 100 | 112 | 100 | |
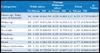
Table 3 shows that patients with venous ulcers had greater difficulty performing activities of daily living (mean overall HAQ-20 = 1.08) compared to patients without ulcers (mean overall HAQ-20 = 0.37), with a difference statistically significant between groups (p=0.002).
| Categories | Group | p-Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| With ulcer | Without ulcer | Total | ||||||||
| No | Mean | SD | n | Mean | SD | n | Mean | SD | ||
| Dress up/ Take care of himself | 56 | 0.86 | 0.841 | 56 | 0.20 | 0.401 | 112 | 0.53 | 0.735 | 0.001* |
| Wake up | 56 | 1.07 | 0.912 | 56 | 0.39 | 0.593 | 112 | 0.73 | 0.838 | 0.002* |
| Eat | 56 | 0.52 | 0.687 | 56 | 0.13 | 0.384 | 112 | 0.32 | 0.586 | 0.002* |
| To walk | 56 | 1.59 | 0.890 | 56 | 0.57 | 0.759 | 112 | 1.08 | 0.969 | 0.001* |
| Hygiene | 56 | 1.00 | 0.653 | 56 | 0.29 | 0.594 | 112 | 0.64 | 0.815 | 0.001* |
| Catch up | 56 | 1.13 | 0.974 | 56 | 0.61 | 0.679 | 112 | 0.87 | 0.875 | 0.001* |
| Hold | 56 | 1.18 | 1.081 | 56 | 0.36 | 0.616 | 112 | 0.77 | 0.968 | 0.001* |
| Others Activities | 56 | 1.32 | 0.917 | 56 | 0.43 | 0.599 | 112 | 0.87 | 0.892 | 0.001* |
| General | 56 | 1.08 | 0.729 | 56 | 0.37 | 0.407 | 112 | 0.73 | 0.686 | 0.002* |
Patients with venous ulcers had a stronger feeling of powerlessness than those without it. It is observed in Table 4 that the average score for the IMSI was 41.2 for the group with venous ulcer and 33.4 for the group without ulcer, with a statistically significant difference between groups (p=0.001).
| Domains | Group | p-Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| With ulcer | Without ulcer | Total | ||||||||
| n | Mean | SD | n | Mean | SD | n | Mean | SD | ||
| Ability to perform Behavior | 56 | 15.59 | 2,130 | 56 | 9.04 | 3.063 | 112 | 12.31 | 4.211 | 0.001* |
| Ability to take instructions | 56 | 11.96 | 2,607 | 56 | 13.95 | 3,272 | 112 | 12.96 | 3.109 | 0.001* |
| Emotional response to control situations | 56 | 13.54 | 2,565 | 56 | 10.57 | 3.173 | 112 | 12.05 | 3.235 | 0.001* |
| General | 56 | 41.21 | 4,853 | 56 | 33.41 | 7.081 | 112 | 37.31 | 7.202 | 0.001* |
DISCUSSION
When the older person acquires a wound, he may find it difficult to carry out various activities in his daily life. Often, these changes in activities of daily living can cause emotional, psychological, and biological suffering in individuals, leading to changes in style and quality of life and sleep, making it impossible for them to carry out their social activities, perform self-care, and participate in leisure and family life, in addition to causing absenteeism at work and even loss of work functions in the productive age group. These factors can make the elderly feel fragile22,23,24,25,26.
In this study, most older people without ulcers were not frail, while most older people with venous ulcers were vulnerable.
Being frail was related to higher incidences of hospitalization during follow-up. Results were shared with other scientific evidence, especially when there was a prevalence ranging from 50% to 80% of frail among hospitalized elderly25,26,27,28,29.
In a study in which the authors verified the levels of frailty and functional independence in instrumental activities of daily living among the elderly identified as frail, it was found: 29.8% with minimal dependence/ supervision and 81.9% with partial dependence for instrumental activities of daily living30. The authors showed greater dependence on activities in frail older people, with females having a higher prevalence of frailty30.
In this research, the means of the total score of elderly patients with venous ulcers in the HAQ-20 and IMSI instruments were high, indicating that these individuals have difficulties performing some daily living activities.
Deficits in functional, cognitive, and psychic capacity are the main causes of loss of independence13,15, leading the elderly to need greater care to carry out activities of daily living.
This issue has become a challenge to be faced by elderly patients with venous ulcers since the population’s life expectancy has increased, leading to a consequent growth in the number of older people with chronic disease and functional disabilities.
Bearing in mind that the functional capacity of human beings declines with age, it is necessary to plan strategies that improve the lifestyle of these individuals with or without wounds, especially concerning programs that promote and improve muscle and joint strength, with social integration inside and outside the family context. These actions would make it possible to minimize the dependence of these individuals on family, social, leisure, and daily activities28,29.
This research reinforces the need to direct the health care of elderly patients with venous ulcers, seeking to identify, in the daily routine of health services, whether in hospitals, outpatient clinics, the Family Health Program, and others, the presence of reduced functional capacity and increase in fragility and a feeling of powerlessness among patients who live with the wound in their daily lives, the main care needs of this population and the caregiver’s knowledge to deal with the assisted person’s disabilities. Furthermore, given the needs that have arisen in recent decades with the increase in chronic diseases and patients with wounds, it is imperative that the academic training and qualification of health professionals value the content and care practice.
CONCLUSION
Venous ulcers negatively impact functional capacity and increase frailty and feelings of powerlessness in the elderly.
1. Universidade Federal de São Paulo, Programa de Pós-graduação em Cirurgia Translacional,
São Paulo, SP, Brazil
Corresponding author: Eliana Gonçalves Aguiar Disciplina de Cirurgia Plástica. Rua Botucatu 740, 2o andar, Vila Clementino, São Paulo, SP, Brazil. Zip code: 04023-062 E-mail: eaguiar@unifesp.br






 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter