INTRODUCTION
Trauma injuries to the hand are a frequent reason for emergency room visits. Dislocations
of the metacarpophalangeal joint (MCP) of the long fingers are rare and serious injuries,
given the connective tissue support present around this joint and its basal position
in the hand1,2. Joint stability is enhanced by bilateral attachments of the deep, transverse metacarpal
ligaments, which unite and stabilize the palmar plate. This intimate relationship
provides stability but is also responsible for the irreducibility of the lesion. The
index and little fingers do not have this bilateral support and, therefore, are more
prone to injuries3.
Dislocations are classified as simple when closed reduction is possible, with the
volar plate remaining fixed to the proximal phalanx in these cases and the finger
being highly hyperextended in the resting position (60 to 90º); or complex when reduction
by closed methods is not possible due to the interposition of periarticular structures,
and its clinical presentation is even rarer4. Most authors agree that the volar plate is the reason for the impossibility of closed
reduction of these lesions5,6.
Clinically, they present with the metacarpophalangeal joint slightly hyperextended
(30-40º) and the interphalangeal joints slightly flexed, adding to palpation of the
metacarpal head (MTP) at the volar level and decreased range of motion of the MCP.
It is important to distinguish between a simple and a complex dislocation because
their approach and treatment are different.
Simple dislocations (or subluxations) can be treated non-surgically by closed reduction,
while attempts at a closed reduction in complex dislocations are often unsuccessful
and often lead to additional complications. Open surgical reduction is the method
of choice in these injuries, allowing joint anatomical recovery with the lowest risk
of complications.
Adequate treatment and knowledge of hand injuries are extremely important, conditioning
the patient’s functional prognosis and limiting the impact and health costs of a long
absence from work. It is essential to determine the best treatment to achieve full
hand functionality recovery and return to work as soon as possible, emphasizing that
this type of injury occurs, in its vast majority, in the working population.
OBJECTIVE
The present study aims to update the clinical and therapeutic approach, analyzing
the advantages and disadvantages of the different surgical techniques used in treating
complex dislocations based on a clinical case operated by the author.
METHODS
A narrative review of the literature on dorsal metacarpophalangeal dislocation of
the long fingers of the hand was performed. The search was performed in Medline (Pubmed
interface), SciELO and Google Scholar databases. The keywords were used: “metacarpophalangeal
joint,” “dislocation,” “open reduction,” and “volar plate.”
Abstracts of articles from the first search were analyzed by the authors, selecting
publications that met the following inclusion criteria: clinical trials, case series,
case reports and literature reviews that included patients diagnosed with dorsal metacarpophalangeal
dislocation of long fingers, articles published in English, Spanish and Portuguese
and no restrictions were established regarding the time of publication.
Exclusion criteria were: metacarpophalangeal dislocation of the first finger and publications
without an identifiable scientific article format.
A clinical case operated by the author is presented, which was evaluated in the emergency
department of the Hospital de Clínicas de Montevideo - Uruguay, from June to December
2020.
This work is carried out following the guidelines of the Ethics Committee of Hospital
de Clínicas, approval number 32. The images of patients in this publication have informed
consent.
CLINICAL CASE
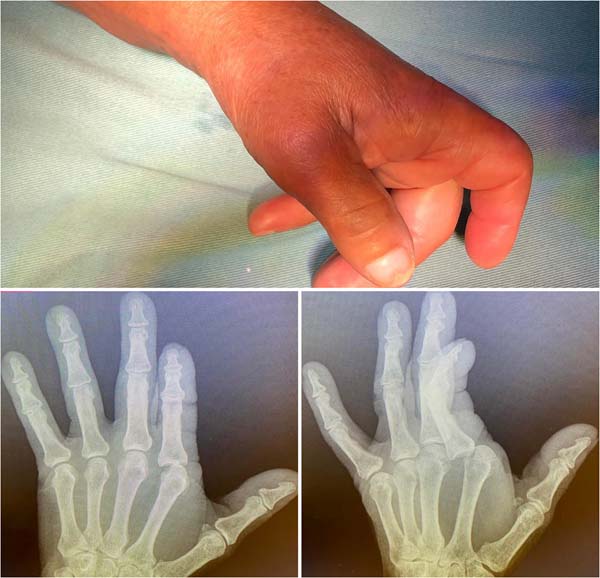
Female patient, 52 years old, right-handed, presented a fall from her height on her
left hand in extension. She consulted the emergency room 12 hours after the trauma.
The energetic hyperextension determined a complex dorsal dislocation of the metacarpophalangeal
joint of the second finger of the left hand, presenting in the emergency with a pathological
attitude, with the MCP joint in 30º of extension and the interphalangeal joints slightly
flexed, with the impossibility of joint mobilization of the second ray (Figure 1).
Figure 1 - Clinical presentation in the emergency. A) Clinical presentation in the emergency
room: metacarpophalangeal joint (MCP) hyperextended to 30º and slightly flexed interphalangeal
joint. B and C) Plain radiographs: anteroposterior view showing ulnar displacement
of the proximal phalanx and enlargement of the joint space. Oblique radiography confirms
dorsal displacement of the proximal phalanx.
Figure 1 - Clinical presentation in the emergency. A) Clinical presentation in the emergency
room: metacarpophalangeal joint (MCP) hyperextended to 30º and slightly flexed interphalangeal
joint. B and C) Plain radiographs: anteroposterior view showing ulnar displacement
of the proximal phalanx and enlargement of the joint space. Oblique radiography confirms
dorsal displacement of the proximal phalanx.
Hand radiographs confirmed the dislocation described without showing the presence
of an interposed sesamoid (Figure 2).
Figure 2 - Intraoperative images. Classic appearance in volar exposure: the metacarpal head (MTP)
is observed with the flexor tendon towards the ulnar and lumbricals towards the radial.
The A1 (A1) pulley is observed in the ulnar and distal sectors before its necessary
cut for reduction. The radial digital nerve (RN) is radially reclined from the metacarpal
head.
Figure 2 - Intraoperative images. Classic appearance in volar exposure: the metacarpal head (MTP)
is observed with the flexor tendon towards the ulnar and lumbricals towards the radial.
The A1 (A1) pulley is observed in the ulnar and distal sectors before its necessary
cut for reduction. The radial digital nerve (RN) is radially reclined from the metacarpal
head.
A closed reduction attempt was made under a regional wrist block without therapeutic
success, so open reduction was coordinated in the operating room under general anesthesia.
It was performed in a closed field with a pneumatic cuff, volar approach through sinusoidal
insertion centered on the head of the second metacarpal. The characteristic findings
of these lesions were identified: disinserted proximal volar plate, interposed and
blocking the joint, radial collateral nerve in close relationship with the metacarpal
head, which was identified and protected during surgery, and displacement of the flexor
to ulnar and lumbrical towards the radial, producing a loop around the head of the
second MTP. Longitudinal sectioning of the A1 pulley and volar plate was performed
to restore normal joint anatomy. Figure 3 shows the normal attitude of the hand after reduction. There were no intra or postoperative
complications.
Figure 3 - Immediate postoperative period. Clinical presentation in front and profile. Correction
of the typical pathological attitude of these lesions is seen.
Figure 3 - Immediate postoperative period. Clinical presentation in front and profile. Correction
of the typical pathological attitude of these lesions is seen.
Immobilization was performed with a locked dorsal brachydigital splint for two weeks,
followed by rehabilitation by occupational therapy consisting of passive and active
range of motion exercises and complementary therapies to control edema and optimize
the healing process. The patient had a good evolution, recovering to the full range
of motion at eight weeks.
DISCUSSION
The pathogenesis and anatomy of these lesions were initially reported by Kaplan7 in 1957, who described that the various structures involved contribute to the irreducibility
of dislocation by closed methods. In 1876, Farabeuf described its management and treatment
based on the description of MCP dislocations of the thumb8.
Dorsal metacarpophalangeal dislocations of the long fingers usually occur in patients
with a history of trauma from a fall with an outstretched hand with the finger in
hyperextension. They can occur in all MCP joints, being more frequent in the external
fingers2,4 due to their greater vulnerability to trauma and the lack of stabilization by the
adjacent deep, transverse metacarpal ligaments. Most of the reports found in the literature
are from the index finger; among these, less than 10% are open9.
Dislocations are classified as simple when closed reduction is possible; in these
cases, the volar plate remains fixed in the proximal phalanx, and the finger is highly
hyperextended in the resting position (60 to 90º); or complex when reduction by closed
methods is not possible, due to the interposition of periarticular structures, and
its clinical presentation is less frequent2,4.
It is important to distinguish between a simple and a complex dislocation because
their approach and treatment are different. Simple dislocations (or subluxations)
can be treated non-surgically by closed reduction. The maneuver is performed by gently
flexing the wrist to relax the flexor tendons and then applying gradual dorsal-to-volar
pressure on the dorsal base of the proximal phalanx, flexing the MCP10 joint. Longitudinal traction instead of force applied based on the first phalanx
can transform a simple displacement into a complex one, making it irreducible and
injuring adjacent structures, which can lead to degenerative arthritis, with a decrease
in the final range of motion8,10-12.
Complex dislocations are those cases in which the volar plate detaches from its junction
with the metacarpal and is interposed between the proximal phalanx and this phalanx2,4,13. It has been reported that the metacarpal head can become trapped between adjacent
tendon structures. In the case of the index finger, the flexors move ulnarly, and
the lumbricals move radially; in the fifth finger, the abductor tendon and the flexor
brevis of the fifth finger move ulnarly and the lumbricals move radially2,4. The swimming ligament can move dorsally, and the superficial transverse metacarpal
ligament proximally7.
Clinically, they present with the metacarpophalangeal joint slightly hyperextended
(30-40º) and the interphalangeal joints slightly flexed secondary to the dorsal displacement
of the proximal phalanx, palpation of the MTP head at the volar level and decreased
range of motion of the MCP11. It can also be accompanied by a slight deviation in the anteroposterior plane, in
the case of the index finger, towards the ulnar14. The wrinkling of the palmar skin on the metacarpal head is recognized as a pathognomonic
sign, which can also associate skin wounds with exposure to the metacarpal head5.
At the time of trauma, the hyperextension force determines the rupture of the weakest
membranous portion of the palmar plate at its insertion into the metacarpal, which
determines its displacement to be stuck in the joint2.
Regarding the paraclinical, frontal, lateral and oblique radiographs should be requested.
An anteroposterior radiograph usually shows an increase in joint space and a displacement
of the base of the phalanx in an ulnar direction. The presence of an interposed sesamoid
within the joint, usually moving distally and ulnarly from the joint, is a characteristic
finding in the diagnosis of volar plate entrapment and seals the closed irreducibility
of these lesions.
Generally, they are better visualized in the oblique approach8,11,14,15. In these cases, Kaplan defined the treatment as “triple release,” adding the extraction
of the volar plate from the joint with the sesamoid. These bones are present in approximately
70% of the population; they appear to cover the MTP head at 12 years of age. Generally,
they are single on the second and third MTP and can be bent on the first, fourth and
fifth rays14.
In the lateral approach to radiography, the base of the proximal phalanx is dorsal
to the metacarpal head and may or may not associate osteochondral fractures in the
dorsal head of the same.
Complex dislocations require surgical treatment through an approach that can be volar,
dorsal, lateral or combined16.
The need for surgical reduction is due to the region’s anatomy, which contributes
to its complexity and difficulty.
Kaplan described the structures responsible for the irreducible nature of the dislocation,
such as the superficial and deep, transverse metacarpal ligaments, the swimming ligament,
the flexor and the lumbrical tendons3,7.
The deep, transverse metacarpal ligament plays a key role in MCP joint stability.
They are closely linked to the volar plate, and together they constitute the most
relevant structures in irreducibility8,15,17. This ligament, which is tense on the dorsum of the dislocated metacarpal head, acts
as a mechanical block, holding the joint in place and making it impossible to reduce.
Gerrand & Shearer15, in their review of the case, proposed a reduction to release the remaining union
of the volar plate with the transverse metacarpal ligament, preserving its distal
insertion in the neck of the proximal phalanx.
As a characteristic finding, the metacarpal head is trapped between adjacent structures:
flexors and lumbricals, and the volar plate detach from its proximal insertion in
the neck of the MTP. It is systematically displaced to be searched in the dorsal joint
space in the MTP head, which acts as a mechanical obstruction in closed reduction2,14.
The closed reduction maneuver in these cases employing traction is usually insufficient
and generates a loop for the metacarpal head, producing more trauma to the adjacent
tissues. Some authors recommend, even after the diagnosis of dislocation, avoiding
closed maneuvers and opting for open reduction as the first treatment option5,14,15.
In their systematic review, Diaz Abele et al.1 recommended reducing closed reduction attempts in the preoperative period and performing
open reduction with minimal delay. Previous attempts at reduction are potentially
traumatic and can lead to further damage to the joint surfaces and even the creation
of a cord around the metacarpal head due to excessive traction. Surgery usually requires
a volar plate cut, and the authors recommend repair with figure-eight stitches and
subsequent immobilization with a dorsal block splint for two weeks, followed by rehabilitation
by the occupational therapy team.
Open reduction is performed in a surgical center under regional or general anesthesia,
with a bloodless field, under a pneumatic cuff that allows for a correct balance of
the lesion and the correct identification of injured structures. Currently, the safety
of using local anesthesia with epinephrine in hand surgery is well known, which provides
anesthesia and a bloodless field through vasoconstriction, eliminating the need for
a pneumatic tourniquet and general anesthesia18.
There are controversies regarding the most appropriate surgical approach for reduction.
In his initial description, Kaplan defends the volar approach, like other authors2,5,9,15. This approach allows direct access to the lesion and subsequent anatomical restoration
of the joint, possibly repairing the volar plate. This may be related to a lower risk
of late instability2.
It is performed through a zigzag or sinusoidal skin incision, which allows distal
and proximal extension over the MCP joint11,15. Care must be taken with the radial collateral nerve and artery in injuries to the
second and third fingers and with the ulnar collateral nerve and artery in injuries
to the fourth and fifth fingers2,15. Neurovascular damage can be avoided by careful dissection and more atraumatic tissue
management.
For reduction, some authors3 refer to the need to section the remaining union of the deep, transverse ligament
attached to the palmar plate and incise the superficial and transverse swimming ligaments.
Releasing the A1 pulley decreases the tension of the loop around the metacarpal. The
proximal phalanx and volar plate can usually be repositioned into their anatomical
positions by relieving tension on the tendon.
If necessary, the palmar plate5,7 can also be released and minimal traction applied to the flexor tendons to perform
the reduction maneuver by moving the MTP head dorsally and making a slight flexion
of the joint from ulnar to radial, flexing the phalanx proximal.
Some authors1,2,14,15 repair the palmar plate with figure-eight stitches with non-absorbable sutures after
the maneuver, and others do not, justifying that the periarticular structures limit
the risk of posterior instability6.
In their review, Diaz Abele et al.1 reported better results when repairing it, having the greatest active metacarpophalangeal
range of motion in these cases. In cases where bone fixation of the palmar plate was
performed, a worse result was obtained regarding the joint range of motion in the
postoperative period. Gerrand & Shearer15, in their review of the case, performed the suture of the volar plate to the periosteum
of the metacarpal in the proximal direction.
The authors who defend the dorsal approach17,19,20 among its advantages highlight the good exposure of the volar plate and the low risk
of injury to the digital nerves. This approach is also useful in those dislocations
associated with osteochondral fractures of the metacarpal head that may require fixation
or excision of the fragment depending on its size. The main disadvantage is that the
volar plate, which is split longitudinally for reduction, cannot be repaired by this
approach.
O’Neill et al.21, in their case report published in 2021, used a dorsal approach, obtaining good results
with an early functional return one month after the injury, despite the delay in definitive
treatment. A centralized incision is made over the joint, and the extensor tendon
and joint capsule must be sectioned longitudinally. The volar plate that appears immediately
interposed is also sectioned longitudinally to subsequently perform reduction by flexing
the wrist and finger.
Barry et al.17, in their study combining their clinical experience with the dissection of anatomical
samples from cadaver hands, compared the volar and dorsal approaches. In cadaveric
dissection, the vulnerability of the radial neurovascular bundle concerning the metacarpal
head of the second toe is highlighted. The advantage of the dorsal approach is highlighted,
as it is simpler and has no risk of injuring vital structures, with the advantage
of being able to address any osteochondral fracture associated with the head of the
MTP. There was no apparent difference in stability after reduction by either approach.
They also emphasize that in all dissections, reduction necessarily required partial
or total release of the deep, transverse ligament, while sectioning of the superficial
and swimming transverse ligaments was only necessary for better exposure. The volar
approach allowed for anatomic restoration of the joint and access to volar plate repair;
this author did not find studies that evaluated its relationship with long-term instability.
Barry et al.17 recommend a volar approach for more experienced hand surgeons and a dorsal approach
for those starting surgery.
Pereira et al.22 reported a case of dislocation of the MCP of the index finger in which an open reduction
was performed via a lateral approach, finding the interposition of the volar plate
and an osteochondral fragment that blocked the reduction.
A straight longitudinal incision was made on the lateral aspect of the MCP joint;
the joint capsule was sectioned longitudinally above the collateral ligament, and
the volar neurovascular bundle and the dorsal nerve branches were identified and protected.
This approach gained access to the dorsal and volar structures, and the intervening
volar plate was reduced and reinserted with a 4.0 Vycril suture. An osteochondral
fragment was identified and fixed with a 1.7mm screw.
Regarding complications, one of the most encountered early is loss of joint amplitude,
which is more frequently manifested in lesions with a delayed surgical resolution,
severe joint infections associated with exposed dislocations, and damage to the digital
collateral nerve2. Among the late complications, osteoarthrosis of the joint and osteonecrosis have
been described, also associated with repeated failed attempts at closed reduction,
open dislocations and prolonged immobilization.
Postoperative immobilization is a controversial issue. Rubin et al.13, in their case series, performed immediately protected mobilization and used immobilization
in one patient for three days.
In their systematic review, Diaz Abele et al.1 suggest immobilization with a locked dorsal splint for two weeks followed by rehabilitation
by occupational therapy, which consists of passive and active range-of-motion exercises,
and complementary therapies to control edema and optimize the healing process23.
McLaughlin10, in his work, reports a less satisfactory range of motion in complex dislocations
immobilized for more than two weeks.
Durakbasa & Guneri2, on the other hand, performed immobilizations in their series of seven cases for
an average of three weeks, with a mean follow-up of 91 months, reporting excellent
functional results in all their patients, standing out as important data in the result
that five of them correspond to the pediatric age. Recovery with a normal range of
motion is generally expected within 6 weeks.
CONCLUSIONS
Complex dislocations of the metacarpophalangeal joint are rare lesions diagnosed by
clinical findings with a slightly hyperextended metacarpophalangeal joint, mild ulnar
deviation of the involved finger, volar palpation of the MCP head, and the presence
of dimples in the palmar skin.
Attempts at closed reduction of complex dislocations are often unsuccessful, and repeated
attempts often lead to additional complications. Open surgical reduction is the method
of choice for treating these injuries, allowing the joint anatomy to recover with
the lowest risk of complications.
Even after diagnosing complex dislocation, it is recommended to avoid closed maneuvers
and opt for open reduction as the first treatment option.
There are several approaches described. The volar approach allows direct access to
the lesion and anatomical restoration of the joint with the possibility of repairing
the volar plate, which may be related to a lower risk of late instability. The dorsal
approach also offers good exposure to the lesion, with a lower risk of injury to the
digital nerves, and also provides good access in cases that associate MCP osteochondral
fractures.
Immobilization with a dorsal locking splint for two weeks is recommended, followed
by rehabilitation and therapy to control edema and optimize the healing process.
As emergency physicians evaluate these patients, knowledge of this injury, proper
diagnosis and prompt referral to hand surgeons for surgical treatment are essential
and determine the functional prognosis of these injuries.
REFERENCES
1. Diaz Abele J, Thibaudeau S, Luc M. Open metacarpophalangeal dislocations: literature
review and case report. Hand (N Y). 2015;10(2):333-7. DOI: 10.1007/s11552-014-9646-6
2. Durakbasa O, Guneri B. The volar surgical approach in complex dorsal metacarpophalangeal
dislocations. Injury. 2009;40(6):657-9. DOI: 10.1016/j.injury.2008.10.027
3. Nussbaum R, Sadler AH. An isolated, closed, complex dislocation of the metacarpophalangeal
joint of the long finger: a unique case. J Hand Surg Am. 1986;11(4):558-61. DOI: 10.1016/S0363-5023(86)80198-8
4. Stiles BM, Drake DB, Gear AJ, Watkins FH, Edlich RF. Metacarpophalangeal joint dislocation:
indications for open surgical reduction. J Emerg Med. 1997;15(5):669-71.
5. Mudgal CS, Mudgal S. Volar open reduction of complex metacarpophalangeal dislocation
of the index finger: a pictorial essay. Tech Hand Up Extrem Surg. 2006;10(1):31-6.
DOI: 10.1097/00130911-200603000-00006
6. Wright CS. Compound dislocations of four metacarpophalangeal joints. J Hand Surg Br.
1985;10(2):233-5. DOI: 10.1016/0266-7681(85)90025-7
7. Kaplan EB. Dorsal dislocation of the metacarpophalangeal joint of the index finger.
J Bone Joint Surg Am. 1957;39-A(5):1081-6.
8. Green DP, Terry GC. Complex dislocation of the metacarpophalangeal joint. Correlative
pathological anatomy. J Bone Joint Surg Am. 1973;55(7):1480-6.
9. Imbriglia JE, Sciulli R. Open complex metacarpophalangeal joint dislocation. Two cases:
index finger and long finger. J Hand Surg Am. 1979;4(1):72-5. DOI: 10.1016/S0363-5023(79)80108-2
10. McLaughlin HL. Complex “locked” dislocation of the metacarpophalangeal joints. J Trauma.
1965;5(6):683-8.
11. Elghoul N, Bouya A, Jalal Y, Zaddoug O, Benchakroun M, Jaafar A. Complex metacarpophalangeal
joint dislocation of the litter finger: A sesamoid bone seen within joint. What does
it mean? Trauma Case Rep. 2019;23:100225. DOI: 10.1016/j.tcr.2019.100225
12. An MT, Kelley JP, Fahrenkopf MP, Kelpin JP, Adams NS, Do V. Complex Metacarpophalangeal
Dislocation. Eplasty. 2020;20:ic3.
13. Rubin G, Orbach H, Rinott M, Rozen N. Complex Dorsal Metacarpophalangeal Dislocation:
Long-Term Follow-Up. J Hand Surg Am. 2016;41(8):e229-33. DOI: 10.1016/j.jhsa.2016.05.010
14. Silberman WW. Clear view of the index sesamoid: a sign of irreducible metacarpophalangeal
joint dislocation. JACEP. 1979;8(9):371-3. DOI: 10.1016/S0361-1124(79)80262-2
15. Gerrand CH, Shearer H. Complex dislocation of the metacarpophalangeal joint of the
index finger with sesamoid entrapment. Injury. 1995;26(8):574-5. DOI: 10.1016/0020-1383(95)98148-C
16. Becton JL, Christian JD Jr, Goodwin HN, Jackson JG 3rd. A simplified technique for
treating the complex dislocation of the index metacarpophalangeal joint. J Bone Joint
Surg Am. 1975;57(5):698-700.
17. Barry K, McGee H, Curtin J. Complex dislocation of the metacarpo-phalangeal joint
of the index finger: a comparison of the surgical approaches. J Hand Surg Br. 1988;13(4):466-8.
DOI: 10.1016/0266-7681(88)90182-9
18. Lalonde DH, Martin A. Epinephrine in local anesthesia in finger and hand surgery:
the case for wide-awake anesthesia. J Am Acad Orthop Surg. 2013;21(8):443-7.
19. Bohart PG, Gelberman RH, Vandell RF, Salamon PB. Complex dislocations of the metacarpophalangeal
joint. Clin Orthop Relat Res. 1982;(164):208-10.
20. Yadav SK, Nayak B, Mittal S. New approach to second metacarpophalangeal joint dislocation
management: the SKY needling technique. Eur J Orthop Surg Traumatol. 2021;31(1):189-92.
DOI: 10.1007/s00590-020-02728-w
21. O’Neill ES, Qin MM, Chen KJ, Hansdorfer MA, Doscher ME. Dislocation of the metacarpophalangeal
joint of the index finger requiring open reduction due to the presence of an intra-articular
sesamoid bone. SAGE Open Med Case Rep. 2021;9:2050313X211021180. DOI: 10.1177/2050313X211021180
22. Pereira JM, Quesado M, Silva M, Carvalho JDD, Nogueira H, Alves J. The Lateral Approach
in the Surgical Treatment of a Complex Dorsal Metacarpophalangeal Joint Dislocation
of the Index Finger. Case Rep Orthop. 2019;2019:1063829. DOI: 10.1155/2019/1063829
23. Afifi AM, Medoro A, Salas C, Taha MR, Cheema T. A cadaver model that investigates
irreducible metacarpophalangeal joint dislocation. J Hand Surg Am. 2009;34(8):1506-11.
DOI: 10.1016/j.jhsa.2009.06.001
1. Hospital de Clínicas Dr. Manuel Quintela, Cátedra de Cirugía Plástica, Reparadora
y Estética, Montevidéu, Uruguai
Corresponding author: Victoria Hernández Sosa Mac Eachen, 1302, Montevidéu, Uruguai. Zip code: 11300, E-mail: victoria.hernandezsosa@gmail.com
Article received: October 22, 2021.
Article accepted: April 7, 2022.
Conflicts of interest: none.