INTRODUCTION
Tissue repair and wound healing are complex processes involving dynamic events, including
coagulation, inflammation, granulation tissue formation, wound contraction and tissue
remodeling1,2. The need to care for patients with wound healing difficulties is a growing challenge
and requires innovative strategies. One approach that stands out in treating these
lesions is low-level laser therapy3. Thus, in recent decades, numerous studies and research have been conducted to investigate
the use of laser therapy in favor of tissue repair1,2.
Low-Level Laser Therapy (LLLT) is conducted at low irradiation intensities, and its
biological effects are secondary to the direct effects of photonic radiation without
thermal reactions. LLLT was first introduced by the work of Mester et al.4 and is known to deliver direct biostimulating light energy to the body’s cells, thereby
enhancing normal cell function and tissue repair4,5.
Therapeutic or low-power lasers are used to accelerate tissue repair processes due
to their biomodulatory effects on cells. They activate or inhibit physiological, biochemical
and metabolic processes through photophysical or photochemical effects. These biomodulatory
phenomena promote the therapeutic effects of morphodifferentiation and cell proliferation,
tissue neoformation, revascularization, reduced edema, greater cell regeneration,
and increased local microcirculation and vascular permeability6.
Many benefits are associated with biomodulation with LLLT. According to Belkin & Schwartz7, the effects require a threshold of exposure to irradiation; depending on the desired
effect, the required fluency, or energy dose, is calculated. The threshold is specific,
and each tissue responds differently to a given wavelength (l).
The methodology is simple, low cost and can be integrated as an adjunct to therapy
for conventional treatments or used alone as an alternative method in some conditions.
The therapeutic effects are anti-inflammatory, analgesic and tissue repair inducer.
The substantial increase in interest in LLLT has been noted due to the significant
number of satisfactory results6.
Several parameters must be adjusted to apply LLLT, such as wavelength, light power,
light type, energy density, power, and total time. The effectiveness of treatment
also depends on many factors, such as the location and nature of the wound and the
patient’s physiological state8. Due to these diverse variables, using a protocol to guide LLLT is very important
in clinical practice.
This work aims to demonstrate the applicability of a low-level laser therapy protocol
in managing cutaneous wound healing. Report the protocol previously created in this
institution by nurses who are members of the skin cancer group (GOPE) and demonstrate
the results obtained in practice.
OBJECTIVE
This study aims to demonstrate the applicability and results of a low-level laser
therapy protocol in managing cutaneous wound healing.
METHODS
This is a retrospective case review study reporting the use of the low-level laser
therapy protocol in managing cutaneous wound healing in the ambulatory dressing service
of the A.C.Camargo Cancer Center. It covers patients who had a skin wound that did
not resolve with conventional treatment, the origin of the wounds being of various
causes, from skin necrosis due to extravasation of intravenous medication to dehiscence
of the surgical wound after tumor exeresis.
All reported cases are of skin wounds and occurred in the years 2016, 2017, 2018 and
2019. The protocol was previously created by nurses who are members of this institution’s
skin cancer group (GOPE), following safety standards for the patient, family and multi-professional
team. There was approval from the local Research Ethics Committee for this study,
number RC 100/21.
Inclusion criteria for using the laser therapy protocol were: patients with wounds
with bone/tendon exposure, necrosis, and chronic or complex wounds that did not respond
to conventional treatment. Exclusion criteria were: malignant neoplastic wound, pregnancy,
patient in serious health condition, metallic prosthesis at the wound site, black
skin, tattoo at the time of chemotherapy infusion, and patient using a cardiac pacemaker.
The characteristics and variables of the low-level laser are applied according to
the particularities of each lesion. In lesions with cutaneous involvement with partial
tissue loss, the variables were: type of light: red, energy density (DE): 80J/cm2, energy (E): 2.1J, power (P): 100mw, time per point: 22 seconds, technique: point,
mode: continuous. In lesions with necrotic tissue (coagulation/liquefaction) or contaminated
wound: type of light: red, DE: 220J/cm2, E: 6.1J, P: 100mw, application time per point: 2 minutes per point, technique: punctual,
mode: pulsed (100pps). In painful lesions: type of light: infrared/red, DE: 80J/cm2, E: 2.1J, P: 100mw, application time per point: 22 seconds, technique: punctual,
mode: continuous. The application of the laser is performed using the punctual technique,
observing a distance of 2 cm per point along the entire length of the wound.
Low-level laser application routine
Materials needed are a procedure mask, goggles, non-sterile procedure gloves, tip
shield, clear film, and polyhexamethylene biguanide (PHMB) solution for surface cleaning.
The outpatient nurse performs the application of the laser after evaluation, and a
conventional dressing is performed after the laser.
The procedure begins with the orientation of the patient and family about the procedure
and its purpose; positioning the patient comfortably according to the location of
the wound; removing the previous dressing, cleaning the wound efficiently, removing
any and all products existing in the lesion and peripheral area (ointments, secondary
dressings of any kind); offer protective eyewear to the patient, family member and
any other individual who remains in the room during laser application; protect the
laser tip with suitable plastic; protect the wound with a transparent film; proceed
with the application of the laser in the wound according to the type of lesion; punctual
application, with a distance of 2 cm from each application.
The application of low-level red or infrared laser does not cause discomfort to the
patient. Any pain complaint should be investigated before proceeding with the treatment.
The minimum interval time between applications of 48 hours must be respected. The
laser in black skin has an increased response; therefore, irradiate with lower doses.
RESULTS
We evaluated the results of implementing this low-level laser therapy protocol and
reported five cases of patients with skin wounds that did not improve with conventional
treatment. The lesions were located in different sites, with lesions on the trunk,
upper limbs and lower limbs. The lesions had an average healing time of 48 days.
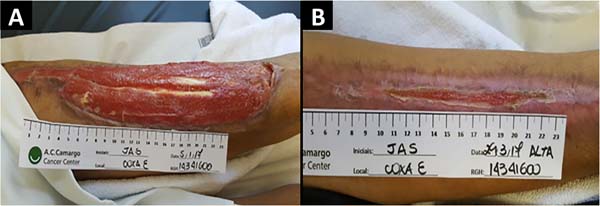
Case 1: female patient, 64 years old, smoker. She presented a dehiscence of the surgical
wound in the left thigh region. Thirteen sessions of low-level laser therapy were
performed; the initial lesion measuring 31x5.5cm in diameter evolved with 98% of the
wound’s healing, uniform appearance, and high-quality tensile strength of the scar.
Closure of the lesion at 83 days (Figure 1).
Figure 1 - (A) Skin lesion on the left thigh, with an initial diameter of 31x5.5 cm. (B) 13 laser
therapy sessions were performed, and wound closure in 83 days.
Figure 1 - (A) Skin lesion on the left thigh, with an initial diameter of 31x5.5 cm. (B) 13 laser
therapy sessions were performed, and wound closure in 83 days.
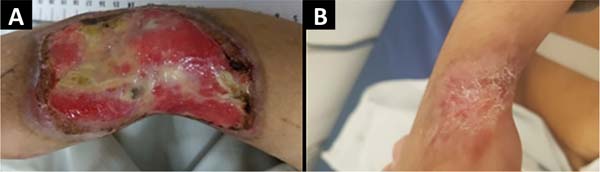
Case 2: male patient, 81 years old, with multiple skin carcinomas. He evolved with
total loss of the partial skin graft in the left thigh. Low-level laser therapy was
started once a week. Significant retraction of the lesion margins of up to 2 cm was
observed on one of the lateral edges of the wound. There was a progressive retraction
of the wound margins and complete healing in 60 days, completing 11 sessions of laser
applications (Figure 2).
Figure 2 - (A) Skin lesion on the left thigh, measuring approximately 17 cm in length. (B) 11
laser therapy sessions were performed, and the wound healed in 60 days.
Figure 2 - (A) Skin lesion on the left thigh, measuring approximately 17 cm in length. (B) 11
laser therapy sessions were performed, and the wound healed in 60 days.
Case 3: female patient, 35 years old, presented skin necrosis after extravasation
of intravenous medication in the dorsum region of the right hand with tendon exposure.
Patient submitted to surgical debridement and vacuum dressing; after 1 month of negative
pressure therapy, the lesion presented 80% of granulation tissue. Currently, 12 laser
therapy sessions are performed twice weekly, maintaining outpatient follow-up, with
complete skin wound healing in 30 days (Figure 3).
Figure 3 - (A) Injury on the back of the right hand after medication extravasation. (B) Twelve
laser sessions were performed, with healing in 30 days.
Figure 3 - (A) Injury on the back of the right hand after medication extravasation. (B) Twelve
laser sessions were performed, with healing in 30 days.
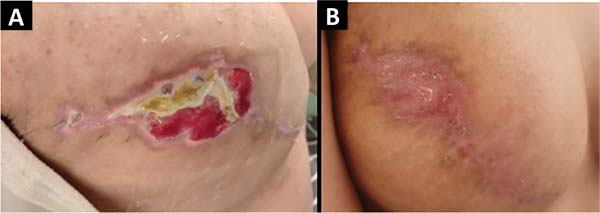
Case 4: The female patient, 34 years old, has surgical wound dehiscence in the right
breast. Eighteen sessions of laser therapy were performed twice a week, initial lesion
measuring 4.5x2.5cm in diameter - resolution of the skin wound in 45 days (Figure 4).
Figure 4 - (A): Right breast lesion measuring approximately 4.5x2.5cm in diameter. (B) 18 laser
sessions were performed, with total healing in 45 days.
Figure 4 - (A): Right breast lesion measuring approximately 4.5x2.5cm in diameter. (B) 18 laser
sessions were performed, with total healing in 45 days.
Case 5: female patient, 39 years old, evolved in the postoperative period with necrosis
in the region of the nipple-areolar complex (NAC) of approximately 5 cm. After debridement
of skin necrosis at the dressing outpatient clinic, she underwent seven sessions of
low-level laser therapy, with wound healing in approximately 25 days of evolution
(Figure 5).
Figure 5 - (A) Lesion on the right breast, evolving with necrosis of the nipple-areolar complex
of approximately 5 cm. (B) After mechanical debridement. (C) She performed seven laser
therapy sessions, with wound healing in 25 days.
Figure 5 - (A) Lesion on the right breast, evolving with necrosis of the nipple-areolar complex
of approximately 5 cm. (B) After mechanical debridement. (C) She performed seven laser
therapy sessions, with wound healing in 25 days.
DISCUSSION
The pathophysiology of laser therapy on healing is a process not fully elucidated
so far. There are theories such as the absorption of light by specific proteins (porphyrins
and flavoproteins) in the respiratory chain, thus increasing the concentration of
intracellular oxygen and stimulating the synthesis of RNA (ribonucleic acid) and DNA
(deoxyribonucleic acid)9. Another possibility would be the photoexcitation of chromophores in the cytochrome
C oxidase molecule, leading to increased cellular metabolism and greater production
of factors related to healing. Despite the incomplete understanding of how the laser
affects the healing process, its modulating and pro-scarring effect is notably widespread
and reported in the scientific literature10.
Black skin is a contraindication to the use of laser therapy in the protocol mentioned
in this study. There is a dearth and limitation of information and research in the
literature on lasers on darker ethnic skin types. The reason for this is the increased
risk of transient and permanent side effects (e.g., blisters, depigmentation and scarring)11.
Through the institutional protocol created by nurses from the Skin Oncology Group
(GOPE) at Hospital AC Camargo, we discussed the results of five cases based on laser
therapy as the main form of treatment for cutaneous wounds, wounds that did not respond
well to treatments with conventional dressings.
The first and second cases are about dehiscence of a donor area in the lateral face
of the left lower limb, one being of a patient already with probable microcirculation
alteration due to smoking, and the second of an elderly patient with comorbidities
and associated atheromatous alteration in the risk factors. We noticed an important
contraction of the wound, associated with a process of delicate cell proliferation,
with a totally satisfactory result considering the extension and complexity of the
wound. The modulatory property of laser therapy is clearly present here, given that
extensive wounds, when not treated with tissue replacement such as grafts, tend to
end up with gross and limiting retractions, very commonly seen in large burns.
When the evaluation focuses on treating complex lesions in institutions with little
economic power, that is, the reality of the vast majority of Brazilian services, implementing
a device with low operational cost can work as an adjuvant to cases that would previously
only be solved with expensive maintenance dressings (such as the negative pressure
dressing) and a greater number of visits to the service, making laser therapy an option
to be observed with special appreciation by health managers12.
In the third case reported in the study, we found a lesion on the dorsal aspect of
the wrist and right hand. A lesion that, in addition to being extensive, presents
greater technical complexity of coverage with grafts due to the difficulty of keeping
the region immobile for adhesion and prolonged immobilization of the hand can lead
to joint impairment due to inactivity. Another point that stands out in case 3 is
the short time interval until the complete resolution of the wound, as well as the
wound’s quality not limiting the limb’s range of motion. The favorable characteristics
related to the patient’s pathological history probably potentiated the effectiveness
of the activation of the healing cascade by the laser and more sessions with shorter
intervals between them.
In the fourth and fifth cases reported, healing of the patient’s breasts occurs after
dehiscence and necrosis, respectively, with an abundance of fibrin, with the possibility
of reconstruction loss due to prosthesis exposure. Lesions with dehiscence and necrosis
are critical points in treating breast cancer, as they can delay the chain of adjuvant
procedures such as radiotherapy. In this case, laser therapy demonstrated a very satisfactory
healing potential, leading to the complete healing of an extensive and deep area relatively
quickly and simply.
An important point to be discussed is not performing laser therapy in potentially
malignant lesions. The laser seems to favor a greater substrate of genomically altered
cells, indirectly accelerating the gain of additional mutations in the natural process
of carcinogenesis13,14.
According to the study by Avci et al.15, low-level laser therapy is a rapidly growing technology used to treat a wide variety
of conditions requiring healing stimulation, relief of pain and inflammation, and
restoration of function.
Although the skin is the organ that is naturally exposed to light more than any other
organ, it still responds well to red and near-infrared wavelengths. Photons are absorbed
by mitochondrial chromophores in skin cells, with consequent transport of electrons,
adenosine triphosphate (ATP) release of nitric oxide, increase in blood flow. Stem
cells can be activated, allowing for increased tissue repair and healing15.
Pinto et al.16 conducted a study on a patient undergoing myocardial revascularization who developed
a dehiscence of the surgical wound in the lower limb on the 15th postoperative day (PO). Conventional treatment was initially performed in the outpatient
clinic without clinical improvement. On the 30th PO day, only laser therapy was applied around the wound edge punctually. The lesion
responded with granulation tissue, decreased inflammatory process and analgesia from
the first application. In this study, laser therapy was shown to play an important
role as a healing facilitator through a non-invasive, effective and safe therapy16.
CONCLUSION
It is concluded that low-level laser therapy, when applied to skin wounds, suggests
a beneficial, promising action and can potentially increase the therapeutic options
available to the surgeon; however, as we reported five cases, further studies are
needed to verify the efficiency of laser in wounds. The presence of a nursing staff
trained in low-level laser therapy is a cornerstone of the entire treatment.
REFERENCES
1. Gutknecht N, Eduardo CP. A odontologia e o laser: atuação do laser na especialidade
odontológica. São Paulo: Quintessence; 2004. p. 25-43.
2. Rodrigo SM, Cunha A, Pozza DH, Blaya DS, Moraes JF, Weber JB, et al. Analysis of the
systemic effect of red and infrared laser therapy on wound repair. Photomed Laser
Surg. 2009;27(6):929-35.
3. Chaves ME, Araújo AR, Piancastelli AC, Pinotti M. Effects of low-power light therapy
on wound healing: LASER x LED. An Bras Dermatol. 2014;89(4):616-23.
4. Mester E, Korényi-Both A, Spiry T, Tisza S. The effect of laser irradiation on the
regeneration of muscle fibers (preliminary report). Z Exp Chir. 1975;8(4):258-62.
5. Li S, Wang C, Wang B, Liu L, Tang L, Liu D, et al. Efficacy of low-level light therapy
for treatment of diabetic foot ulcer: A systematic review and meta-analysis of randomized
controlled trials. Diabetes Res Clin Pract. 2018;143:215-24.
6. Henriques ACG, Cazal C, Castro JFL. Ação da laserterapia no processo de proliferação
e diferenciação celular: revisão da literatura. Rev Col Bras Cir. 2010;37(4):295-302.
7. Belkin M, Schwartz M. New biological phenomena associated with laser radiation. Health
Phys. 1989;56(5):687-90.
8. Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR, et al. The nuts and bolts
of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516-33. DOI: 10.1007/s10439-011-0454-7
9. Kreisler M, Christoffers AB, Willershausen B, d’Hoedt B. Low-level 809 nm GaAlAs laser
irradiation increases the proliferation rate of human laryngeal carcinoma cells in
vitro. Lasers Med Sci. 2003;18(2):100-3.
10. Karu TI, Pyatibrat LV, Kalendo GS. Photobiological modulation of cell attachment via
cytochrome c oxidase. Photochem Photobiol Sci. 2004;3(2):211-6.
11. Battle EF Jr, Hobbs LM. Laser therapy on darker ethnic skin. Dermatol Clin. 2003;21(4):713-23.
12. Follador W, Secoli SR. A farmacoeconomia na visão dos profissionais da saúde. In:
Nita ME, Campino ACC, Secoli SR, Sarti FM, Nobre M, Costa AM, et al., eds. Avaliação
de tecnologias em saúde. Porto Alegre: Artmed; 2010. p. 248-68.
13. Pinheiro AL, Carneiro NS, Vieira AL, Brugnera A Jr, Zanin FA, Barros RA, et al. Effects
of low-level laser therapy on malignant cells: in vitro study. J Clin Laser Med Surg.
2002;20(1):23-6.
14. Mognato M, Squizzato F, Facchin F, Zaghetto L, Corti L. Cell growth modulation of
human cells irradiated in vitro with low-level laser therapy. Photomed Laser Surg.
2004;22(6):523-6.
15. Avci P, Gupta A, Sadasivam M, Vecchio D, Pam Z, Pam N, et al. Low-level laser (light)
therapy (LLLT) in skin: stimulating, healing, restoring. Semin Cutan Med Surg. 2013;32(1):41-52.
16. Pinto NC, Pereira MHC, Stolf NAG, Chavantes MC. Laser de baixa intensidade em deiscência
aguda de safenectomia: proposta terapêutica. Rev Bras Cir Cardiovasc. 2009;24(1):88-91.
1. A.C.Camargo Cancer Center, São Paulo, SP, Brasil
2. A.C.Camargo Cancer Center, Departamento Oncologia Cutânea, São Paulo, SP, Brasil
Corresponding author: Ana Carolina Vasconcellos Guedes Otsuka Av. da Aclimação, 314, São Paulo, SP, Brazil. Zip code: 01531-000, E-mail: ac.otsuka@gmail.com
Article received: 2021/10/6.
Article accepted: 2022/4/7.
Conflicts of interest: none.