INTRODUCTION
Breast cancer is the leading cause of death in women and the most incident
globally, with a rate of 2.1 million new cases in 2018 and a percentage of 6.6%
of total deaths from all types of diseases1. Considering the Brazilian incidence, after non-melanoma
skin tumors, breast cancer is also the most common among women and the leading
cause of death from cancer in the population, representing 16.5% of all deaths
in 2014- 20202. In addition,
66,280 new cases were estimated for 2020, indicating an incidence of 43.74 cases
per 100,000 women3.
Mastectomy, which removes one or two breasts through a surgical procedure, is
performed when other treatments such as chemotherapy and radiotherapy are not
effective, either because of the advanced stage of the tumor or its location. It
is a milestone for women who need to undergo it due to the consequences in these
women’s lives4,
affecting their femininity and self-image, as the breast symbolizes the feminine
sphere. These impacts affect the patient’s entire social life, from
romantic relationships to professionals, as many women become ashamed of their
own bodies. The surgery impacts not only aesthetic and physical, but also
emotional, self-esteem, and sex life4.
Due to the large recurrence of late breast cancer diagnosis and the delay in
accessing appointments, exams, biopsy and treatment, approximately 70% of
diagnosed patients will need to have their breast removed5. According to Law 11,664/2008,
the Brazilian Unified Health System (SUS - Sistema Único de
Saúde - in portuguese) should ensure that all women, from 40
years of age, undergo mammography as a way of preventing and detecting neoplasia
in its initial form since the incidence and mortality of this pathology tends to
grow progressively in this age group6. However, it is observed that such examination is performed
in the SUS, only in ages between 50 and 69, under the guidance of the Ministry
of Health7. It is important to
note that under the age of 40, there are fewer than 10 deaths per 100,000 women,
while in the age group over 60 years, the risk is 10 times greater, thus showing
the importance of early diagnosis3.
With the progression of cancer or even cancer treatment, some women may suffer
some mutilations in the breast. As a way of restoring the esthetic standard,
they are assured of immediate reconstructive plastic surgery8. The purpose of reconstructive
plastic surgery is to reestablish the region’s regular anatomy and
restore the self-esteem lost by some women during surgical treatment9. However, some problems can be
observed in this process, such as cases of breast seroma, hematomas, necrosis,
dehiscence, asymmetry and late venous thrombosis, which in some cases can lead
to the patient’s death10. Other problems are intrinsically related to SUS support
for patients, such as the lack of trained doctors and the structure to carry out
the necessary procedures11.
SUS neglected the right to surgery reparatory until 1999 when it became their
right. Despite this achievement, it was only in 2013 that the surgery had a
deadline to be performed, which should occur soon after the mastectomy or as
soon as the woman presents conditions for it8. Furthermore, in 2018, the right to surgery on both
breasts was approved to ensure symmetry10. Thus, this article seeks to answer the major impacts
caused by mastectomy in women in Brazil. Therefore, the study’s objective
was to highlight the importance of performing plastic surgery for women with
mastectomies and to elucidate the rights of these patients guaranteed by SUS in
Brazil during the process.
METHODS
This study has a qualitative approach, with a descriptive and exploratory
purpose, having used the bibliographic review of the integrative type as a data
collection technique.
The Scientific Electronic Library Online (SciELO), PubMed and Latin American and
Caribbean Health Sciences Literature (LILACS) platforms were used for data
collection. Google Scholar platform was used for further research. The search
was performed using the Boolean descriptors and operators: “plastic
surgery” OR “reconstructive surgery” AND
“neoplasm” OR “breast carcinoma in situ” OR
“unilateral breast cancer” OR “mastectomy” AND
“unique health system” OR “legislation.” In
addition, the resolutions of the Legislation Portal (http://www4.planalto.gov.br/legislacao/)x addressed
women’s rights concerning breast reconstruction surgery in the SUS were
consulted.
As exclusion criteria, articles before 2010 that addressed non-mammary neoplasms,
dissertations on surgical techniques and the diagnosis of tumors, as well as
studies carried out in patients in countries other than Brazil, were
disregarded. Studies that described the benefits reported by patients, or by the
literature itself, of performing post-mastectomy breast reconstruction, in
addition to articles that addressed the role of the SUS in reconstructive
surgery in terms of management and epidemiology. There was no language
restriction.
The results of the articles were evaluated through thematic content analysis. The
themes most discussed by the patients were counted when reporting their
perception during the mastectomy process and after reconstructive surgery. This
type of analysis allows for quantifying the frequency of the most discussed
topics, whose results were processed using Excel 2010 software.
RESULTS
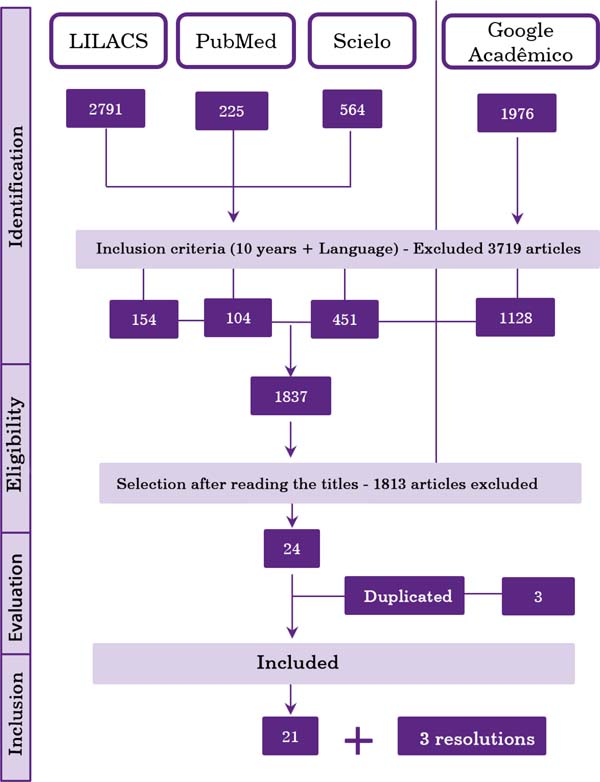
Five thousand five hundred fifty-six articles were found. After applying the
filters (articles with full text on the platform, published in the last ten
years) and an initial reading of the titles and abstracts, it resulted in 21
studies discussing the results. In addition, three resolutions were included,
found on the Legislation Portal, as shown in Figure 1.
Of the selected articles, 16 addressed mainly the relationship between the
performance of breast reconstructive surgery and the improvement of the
woman’s quality of life, 2 about the feeling of post-mastectomy women, 1
addressed the comparison of the emotions of women who underwent or not breast
reconstruction, and 2 discussed the role of SUS and public health about cosmetic
surgery. In addition, the years of publication with the most selected studies
were 2013, 2017 and 2019, with 4, 3 and 4 works, respectively. However, two
articles from 2010, 2012, 2016 and 2020 were still selected; and one from 2015
and 2018, as shown in Chart 1.
From the resolutions found on women’s rights regarding breast
reconstruction after mastectomy performed by SUS, Laws n° 9797, n°
12802 and n° 13.770 were selected, published respectively on May 6, 1999,
April 24, 2013, and December 19, 2018.
Profile of women with mastectomies
The analysis of 19 articles about women with mastectomies showed that, in
general, they have a profile between 41 and 60 years of age. In addition,
most articles show a predominance of white participants with complete
elementary education and Catholics (Chart 2).
Relationship between performing reconstructive surgery and the
woman’s perception of her body
Among the 16 studies analyzed, which mostly addressed the relationship
between performing breast repair surgery and improving the quality of life
of women, 42.1% said that women felt anxiety, followed by feelings such as
fear, depression and sadness (Table 1). In addition, some of the patients had decreased sexual desire,
avoiding any intimate contact.
Among the included studies, an analysis of satisfaction with the breast,
psychological and sexual well-being was presented by comparing 79 patients
who underwent augmentation mammoplasty and 64 who did not. Of these, it was
observed that patients undergoing reconstruction improved their self-image
and feeling of overcoming cancer12. In addition, comparing before and after the
reconstruction surgery, an increase in the patients’ physical and
mental well-being was observed13. Therefore, it is generally possible to see that
patients’ quality of life after breast reconstruction with breast
implants is superior concerning the period before the procedure.
In the study by Carneiro et al. (2020)14, the assessment of these women’s feelings
was also quite significant, with feelings of fear, shame, suffering,
depression, loss, dissatisfaction being reported before the aesthetic
procedure, which seem to decrease, or even disappear, after the surgery, as
you can see in the patients’ statements:
“[...] I was very satisfied with the plastic surgery for breast
reconstruction, it was as if I had been reborn, it’s another
condition of life! I came back to life!” (p. 47746)
“[...] Knowing Ora of joy, right! Because I imagined that I would have
that defect there, that we would look at, and see that thing without...
right! Small right, but it is always defective, right. There was that
emptiness, ugly thing there that I needed to do, so I resigned myself, but
always nervous. It’s a lot of suffering. After the surgery to redo
the breast, I dared to leave.” (p. 47746)
Chart 3 presents the main feelings
brought by the articles of the patients after reconstructive surgery. In
general, surgery is an option to reduce the negative emotions that are
caused by the disease and the treatment, to improve self-esteem by replacing
the “empty space” with a breast, facilitating clothing and
seeing oneself body, changing the feeling of mutilation to a sense of
renewed femininity and sensuality10. When comparing factors such as the age of the
patients, it is possible to highlight that in physical aspects, younger
women had better results, which indicates that it is associated with a lower
presence of comorbidities in this age group, as well as in mental aspects,
young women demonstrate a greater impact on self-esteem, which is expressed
by the greater attachment to the body and following the standards of beauty
imposed by society4.
The role of the SUS in the quality of life of women with
mastectomies
According to Law No. 9,797, it was decreed as mandatory to carry out breast
reconstructive plastic surgery by the network of units part of the SUS in
mutilation cases after cancer treatment15. Some changes arose in Article 2nd when
a new law was enacted, Law No. 12,802, adding two paragraphs. The
1st is to ensure that the reconstruction will be carried out
when technical conditions exist at the same surgical time. The
2nd addresses the case impossibility of immediate
reconstruction. The patient has the right to be referred for follow-up and
will be guaranteed to undergo surgery immediately after reaching the
necessary clinical conditions8.
Figure 1 - Flowchart of article collection in Latin American and Caribbean
Health Sciences Literature (LILACS), PubMed and Scientific
Electronic Library Online (SciELO) platforms. Using Google Scholar
as a complementary source. The arrows indicate the selection of
articles according to the inclusion and exclusion criteria set out
in the methodology.
Figure 1 - Flowchart of article collection in Latin American and Caribbean
Health Sciences Literature (LILACS), PubMed and Scientific
Electronic Library Online (SciELO) platforms. Using Google Scholar
as a complementary source. The arrows indicate the selection of
articles according to the inclusion and exclusion criteria set out
in the methodology.
Chart 1 - Data from selected articles for the study.
| Author |
Date |
Title |
Magazine |
Type |
Subject |
| Loyal et al.12 |
2010 |
The body,
cosmetic surgery and collective health: a case study.
|
Journal of
Science and Public Health
|
Case
study
|
Relationship of cosmetic surgery with collective health and
health promotion.
|
| Moura et al.13 |
2010 |
The feelings of post-mastectomized
women.
|
Anna Nery School of Nursing Magazine |
Descriptive Qualitative Study |
How women feel after mastectomy. |
| Cesnik and Santos14 |
2012 |
Mastectomy
and sexuality: an integrative review.
|
Psychology
Journal: Reflection and Criticism
|
Integrative
review
|
Impact of
cancer and mastectomy on women's sexuality.
|
| Majewski et al.15 |
2012 |
Quality of life in women who underwent
mastectomy compared to those who underwent conservative
surgery: a literature review.
|
Journal of Science and Public Health |
Literature review |
Comparison between women who underwent a
mastectomy and those who underwent conservative
treatment.
|
| Cosac et al.16 |
2013 |
Breast
reconstructions: a 10-year retrospective study.
|
Revista
Brasileira de Cirurgia Plástica
|
Case
study
|
Analysis of
post-mastectomy breast reconstruction cases for breast
cancer.
|
| Colombo17 |
2013 |
Assessment of the degree of satisfaction of
patients undergoing breast reconstruction.
|
Revista Brasileira de Cirurgia
Plástica |
Retrospective study |
Patient satisfaction after breast
reconstruction.
|
| Furlan et al.4 |
2013 |
Quality of
life and self-esteem of mastectomized patients undergoing or
not breast reconstruction.
|
Revista
Brasileira de Cirurgia Plástica
|
exploratory
qualitative study
|
Quality of
life of mastectomized patients undergoing or not breast
reconstruction.
|
| Gomes and Silva18 |
2013 |
Self-esteem assessment of women undergoing
breast cancer surgery.
|
Text and Context Nursing |
Cross-sectional observational study |
Self-esteem of women after cancer
surgery.
|
| Guimarães et al.19 |
2015 |
Sexuality
after augmentation mammoplasty.
|
Revista Brasileira de Cirurgia
Plástica |
Case
study
|
Assess
sexuality after augmentation mammoplasty.
|
| Braga et al.9 |
2016 |
Breast reconstruction process in
mastectomized women.
|
Interdisciplinary Magazine |
Literature review |
Process involved from mastectomy to breast
reconstruction.
|
| Thais Rodrigues Guedes20 |
2016 |
Body image
of women undergoing treatment for breast cancer.
|
|
Masters
dissertation
|
Self-esteem
of cancer patients
|
| Alves, VL et al.21 |
2017 |
Early assessment of the quality of life and
self-esteem of mastectomized patients undergoing or not
breast reconstruction.
|
Revista Brasileira de Cirurgia
Plástica |
Cross-sectional, comparative and analytical
observational study
|
Make a comparison about the self-esteem of
mastectomized patients undergoing reconstruction and those
who did not undergo plastic surgery.
|
| Martins, et al.22 |
2017 |
Immediate
breast reconstruction versus no post-mastectomy
reconstruction: a study on quality of life, pain and
functionality.
|
Physiotherapy and Research Journal |
Cross-sectional descriptive study |
Comparison
between immediate breast reconstruction versus no
post-mastectomy reconstruction.
|
| Villar et al.23 |
2017 |
Quality of life and anxiety in women with
breast cancer before and after treatment.
|
Latin American Journal of Nursing |
Prospective observational study |
Before x after women being treated for breast
cancer.
|
| Casassola et al.24 |
2018 |
Satisfaction with breast cancer surgery: Comparison between
mastectomized patients with and without breast
reconstruction.
|
International Exhibition of Teaching, Research and
Extension
|
Qualitative
study
|
Comparison
between women with mastectomies who underwent plastic
surgery and those who did not.
|
| Archangel et al.25 |
2019 |
Sexuality, depression and body image after
breast reconstruction.
|
Clinics |
Case study |
Quality of life after breast
reconstruction.
|
| Cammarota et al.10 |
2019 |
Quality of
life and aesthetic result after mastectomy and breast
reconstruction.
|
Revista Brasileira de Cirurgia
Plástica |
Case
study
|
Quality of
life of women undergoing breast reconstruction after cancer
treatment.
|
| Cosac et al.26 |
2019 |
Breast reconstructions: a 16-year
retrospective study.
|
Revista Brasileira de Cirurgia
Plástica |
Case study |
Analysis of post-mastectomy breast
reconstruction cases for breast cancer.
|
| Volkmer et al.27 |
2019 |
Breast
reconstruction from the perspective of women undergoing
mastectomy: a meta-ethnography.
|
Text and
Context Nursing
|
Literature
review
|
What do
women undergoing mastectomy think about breast
reconstruction?
|
| Carneiro et al.28 |
2020 |
Psychological repercussions of plastic
surgery in mastectomized women.
|
Brazilian Journal of Development |
Literature review |
Quality of life of women who underwent
mastectomies after plastic surgery.
|
| Mollinar et al.11 |
2020 |
Oncoplastic
and reconstructive surgery of the breast: analysis of the
patient's rights within the scope of the SUS.
|
Brazilian
Journal of Development
|
Literature
review
|
Rights of
SUS patients for mastectomy and breast reconstruction.
|
Chart 1 - Data from selected articles for the study.
On December 19, 2018, Law No. 13.770 was created, in which three paragraphs
were added to Article 1st, with the 1st paragraph to
ensure that the breast reconstruction will be carried out during the
surgical time of the mutilation when technical conditions exist, the
paragraph 2nd in the event of the impossibility of immediate
reconstruction, the patient will be referred for follow-up and will have the
right to undergo surgery immediately after having the necessary clinical
conditions, and paragraph 3rd guarantees that the procedures will
symmetrize the contralateral breast and reconstruct the nipple-areola
complex integrate reconstructive plastic surgery16.
DISCUSSION
The age group in the literature for mastectomized patients was a little lower
than the Ministry of Health recommended starting performing breast cancer
screening (50 to 69 years). It is possibly due to excessive exam requests
resulting in unnecessary treatments and earlier exposure to ionizing radiation
in women, implying more risks than benefits with advancing age17.
The most prevalent age can be explained by the epidemiology of the disease, being
more common in women at the end of their childbearing lives. Menopause is the
main risk factor for the disease, even more determinant than lifestyle habits
and genetics11. As for family
income, it is common for screening and the search for the health system to
happen early in women who are part of a socioeconomic population with higher
income, as this population has easier access to the private health system,
health insurance, as well as greater access to information about the pathology
and its clinical course18. In
addition to the lower search for disease tracking, women with lower income, less
education, and housewives are more likely to affect mental health, developing
pathologies such as anxiety and eating disorders, making them even more prone to
worse psychic progression after mastectomy.19
Breast cancer has a high prevalence and causes a great impact on women’s
lives, affecting both their physical and psychological aspects20. Since the diagnosis is
confirmed, the female identity starts to be questioned by the patient; after
all, the breasts are considered a symbol of femininity and body beauty21. Therefore, breast
reconstruction surgery has caused great satisfaction in post-mastectomized
patients, as it is a good alternative to improve their self-esteem.
Chart 2 - Epidemiological profile of women who underwent mastectomy according
to the chosen articles.
| Variables |
Observed
profile
|
| Age
group
|
More than 60%
of women aged 41-60 years.
|
| Color |
It depends on the study's region, but it has a
greater predominance in white women.
|
| Education |
More than 60%
of women have education (in years) from 1 to 9 years,
corresponding to complete primary education.
|
| Family income |
Family income is around 1 to 3 minimum
wages.
|
| Religion |
It follows the
regional pattern, tending to follow the national average, with
more than half Catholic.
|
Chart 2 - Epidemiological profile of women who underwent mastectomy according
to the chosen articles.
Table 1 - Feeling about mastectomy. The percentage corresponds to the number of
articles that cited each feeling concerning the total of 16.
| Feelings |
% of
articles
|
| Anxiety |
42.1 |
| Fear |
31.5 |
| Depression |
21.0 |
| Sadness |
15.7 |
| Fault |
10.5 |
| Anguish |
10.5 |
| Insecurity |
10.5 |
| Conformism |
5.2 |
| Defensive posture |
5.2 |
| Shame |
5.2 |
| Worry |
5.2 |
| Inferiority |
5.2 |
| Feeling of worthlessness |
5.2 |
Table 1 - Feeling about mastectomy. The percentage corresponds to the number of
articles that cited each feeling concerning the total of 16.
Thus, mastectomy can cause emotional and psychological distress, with significant
improvements after breast reconstruction22. Still, it is important to emphasize that women have a
higher rate of depression than men, which may highlight some biopsychosocial
factors, such as educational and historical issues, and face losses as possible
explanations for this indicator23.
The changes suffered in the body generate difficulty for women undergoing
treatment for breast cancer, mainly due to prejudice and stigma associated with
this disease21. This is
related to the side effects of the treatment, the main ones being menopause and
alteration in the production of sex hormones9. These hormonal changes can also cause problems such as
vaginal dryness, dyspareunia, even vaginal atrophy, which brings another
psychological shock to the woman, making healthy sexual intercourse a
challenge24.
Chart 3 - Main factors observed in the change in the quality of life after
breast reconstruction after analyzing the articles by Monteiro et al.
(2015)x, Furlan et al. (2013)4, Ng et al. (2016)12 and Zhong et al.
(2013)13.
| Main
changes after breast lift
|
| Sexuality |
Sexuality increased significantly, in addition to the
improvement in sexual satisfaction, showing no significant
difference between patients who were or were not in a stable
relationship.
|
| Self-esteem |
The improvement in self-esteem appears
to be directly related to the patient's age, and the younger she
is, the greater the result in her emotional function.
|
| Psychosocial well-being |
Patients are more self-confident, more accepting of their own
bodies, strengthened in social environments and emotionally
healthy.
|
| Physical well-being |
Few or almost no complaints of
unbearable pain in the area of the breasts after surgery were
observed, with only the increased sensitivity in the area
standing out.
|
Chart 3 - Main factors observed in the change in the quality of life after
breast reconstruction after analyzing the articles by Monteiro et al.
(2015)x, Furlan et al. (2013)4, Ng et al. (2016)12 and Zhong et al.
(2013)13.
A study carried out with 47 patients resulted in a great improvement in the
sexuality of women undergoing mammoplasty surgery, showing an improvement in
sexual satisfaction and arousal25. In addition to this, other studies have shown that there
is a great benefit in performing breast reconstruction for post-mastectomized
patients, reporting that patients who have not undergone this procedure have
greater emotional fragility4.
Faced with so many negative impacts on the lives of women undergoing treatment
for breast cancer, there is still certain negligence on the part of
professionals about feminine emotionality, which is unacceptable since body and
mind are in common26.
Therefore, health professionals must support these patients, clarifying possible
doubts, providing emotional support and managing the case in the best possible
way to have the least likely impact on the woman’s life27.
Based on the review of the articles, it is possible to observe the importance of
aesthetic procedures in the physical and psychological recovery of women who
underwent a procedure as aggressive as mastectomy10. Surgical intervention through mastectomy can
be performed with conservative methods such as quadrantectomy and nodulectomy or
more radical methods that consist of total ablation of the breast and muscles.
It is known that the emotionality of these women undergoing these procedures is
affected throughout the treatment stage. However, it is mainly at the end of the
treatment that difficulties in adaptation, restrictions and even negative
repercussions in their sexual life arise20.
The complications of cosmetic surgery for breast repair and reconstruction are
difficult to resolve, as they are inherent in any medical procedure, whether it
is of low or high complexity. However, the surgeon must pay attention to risk
factors such as obesity and smoking, as these contribute to complications and
are essential to carry out a good preoperative period and strict follow-up after
surgery28. The risk of
performing this cosmetic surgery, being minimal, is offset by so many benefits
provided to women, the main ones being an improvement in self-esteem and a
feeling of greater femininity29.
Concerning the cost of surgery problems and others mentioned above, such as
possible complications, it is difficult to propose solutions to establish a more
beneficial scenario for both the system and the individual. A possible solution
would be to improve the active screening of the target population since, in the
early diagnosis, the number of procedures, mortality, and the cost of operations
decreases significantly compared to the spontaneous search for
patients11.
Thus, the right that women won, in 1999, to perform the procedure through the
SUS, associated with the fact that this procedure is performed soon after the
mastectomy, were important milestones in the fight for a better quality of life
for women victims of breast cancer11. Despite this achievement, it was only in 2018 that it was
possible to win the right to carry out bilateral repairs to maintain the
symmetry of the breasts through an update to the 1999 law, ensuring a better
aesthetic result and with good impacts on their quality of life11,30.
CONCLUSION
The present study showed that performing plastic surgery in women with
mastectomies greatly impacts several psychological, sexual, affective, and
social pillars of their lives. Despite having won several rights that address
mastectomy and its consequences, there are still adversities that could be
overcome with greater investment in secondary prevention, with more effective
active screening.
This measure would be important to reduce treatment costs since the early stages
of cancer require fewer interventions and less costly and less invasive
procedures.
As for the psychological impacts of the consequences of the surgery and
treatment, the preparation of professionals is essential to answer this
patient’s doubts and welcome her concerns and concerns. Therefore, the
naturalization of the suffering of these patients cannot occur, as it often
leads to negligence in care. And, an important part of this care, humanization
and dignification of women already takes place in the reconstruction surgery,
which aims to return a physical symbol of female sensuality and pride.
REFERENCES
1. World Health Organization (WHO). Global Cancer Observatory (GCO).
Estimated age-standardized mortality rates (world) in 2018, worldwide, female,
all ages [Internet]. Lyon: Cancer Today/WHO; 2018; [acesso em 2020 Nov 29].
Disponível em: https://gco.iarc.fr/today/online-analysis-multi-bars?v=2020&mode=cancer&mode_population=countries&population=900&populations=900&key=asr&sex=0&
2. Instituto Nacional de Câncer (INCA). Mortalidade proporcional
não ajustada por todas as neoplasias, mulheres, Brasil, entre 2014 e 2018
[Internet]. Rio de Janeiro: INCA; 2018; [acesso em 2020 Nov 29].
Disponível em: https://mortalidade.inca.gov.br/MortalidadeWeb/pages/Modelo01/consultar.xhtml#panelResultado
3. Instituto Nacional de Câncer (INCA). Estimativa 2020:
incidência de câncer no Brasil [Internet]. Rio de Janeiro: INCA;
2020; [acesso em 2020 Nov 29]. Disponível em: https://www.inca.gov.br/publicacoes/livros/estimativa-2020-incidencia-de-cancer-no-brasil
4. Furlan VLA, Neto MS, Abla LEF, Oliveira CJR, Lima AC, Ruiz BFO, et
al. Qualidade de vida e autoestima de pacientes mastectomizadas submetidas ou
não a reconstrução de mama. Rev Bras Cir Plást. 2013
Jun;28(2): 264-9.
5. Correio Brasiliense (BR). Demora no diagnóstico de
câncer leva à mastectomia em 70% dos casos [Internet].
Brasília (DF): Correio Brasiliense; 2018; [acesso em 2020 Nov 29].
Disponível em: https://www.correiobraziliense.com.br/app/noticia/ciencia-e-saude/2018/05/06/interna_ciencia_saude,678759/demora-no-diagnostico-de-cancer-leva-a-mastectomia-em-70-dos-casos.shtml
6. Lei no 11.664, de 29 de abril de 2008 (BR). Dispõe
sobre a efetivação de ações de saúde que
assegurem a prevenção, a detecção, o tratamento e o
seguimento dos cânceres do colo uterino e de mama, no âmbito do
Sistema Único de Saúde - SUS. Diário Oficial da
União, Brasília (DF), 29 abr 2008; Seção 1:
1.
7. Federação Brasileira de Instituições
Filantrópicas de Apoio à Saúde da Mama (FEMAMA). O
câncer de mama em números [Internet]. Porto Alegre: FEMAMA; 2019;
[acesso em 2020 Nov 29]. Disponível em: https://www.femama.org.br/site/br/noticia/o-cancer-de-mama-em-numeros
8. Lei no 12.802, de 24 de abril de 2013 (BR). Altera a Lei
nº 9.797, de 6 de maio de 1999, que “dispõe sobre a
obrigatoriedade da cirurgia plástica reparadora da mama pela rede de
unidades integrantes do Sistema Único de Saúde - SUS nos casos de
mutilação decorrentes de tratamento de câncer”, para
dispor sobre o momento da reconstrução mamária.
Diário Oficial da União, Brasília (DF), 24 abr
2013.
9. Braga AKG, Santos TLC, Magalhães MAV. Processo de
reconstrução mamária em mulheres mastectomizadas. Rev
Interd. 2016;9(1):216-23.
10. Cammarota MC, Campos AC, Faria CADC, Santos GC, Barcelos LDP, Dias
RCS, et al. Qualidade de vida e resultado estético após
mastectomia e reconstrução mamária. Rev Bras Cir
Plást. 2019;34(1):45-57.
11. Mollinar ABP, Pereira IPC, Araújo JSF, Smith JSR, Guerra MCA,
Real Junior MMF, et al. Cirurgia oncoplástica e reconstrutiva da mama:
análise acerca dos direitos do paciente no âmbito do SUS. Braz J
Develop. 2020;6(8):54485-503.
12. Leal VCLV, Catrib AMF, Amorim RF, Montagner MA . O corpo, a cirurgia
estética e a Saúde Coletiva: um estudo de caso. Ciência
& Saúde Coletiva. 2010; 15 (1): 77-86.
13. Moura FMJSP, Silva MG, Oliveira SC, Moura LJSP. Os sentimentos das
mulheres pós-mastectomizadas. Esc Anna Nery. 2010; 14(3):
477-84.
14. Cesnik VM, Santos MA. Mastectomia e sexualidade: uma revisão
integrativa. Psicologia: Reflexões e Crítica. 2012; 25(2):
339-49.
15. Majewski JM, Lopes ADF, Davoglio T, Leite JCDC. Qualidade de vida em
mulheres submetidas à mastectomia comparada com aquelas que se submeteram
à cirurgia conservadora: uma revisão de literatura. Ciência
& Saúde Coletiva. 2012; 17(3): 707-16.
16. Cosac OM, Filho JPPC, Barros APGSH, Borgatto MS, Esteves BP, Curado
DMC, et al. Reconstruções mamárias: estudo retrospectivo de
10 anos. Rev Bras Cir Plást. 2013;28(1):59-64.
17. Colombo FG. Avaliação do grau de
satisfação de pacientes submetidas a reconstrução
mamária. Rev Bras Cir Plast. 2013; 28(3): 355-60.
18. Gomes NS, Silva SR. Avaliação da autoestima de
mulheres submetidas à cirurgia oncológica mamária. Texto
Contexto Enferm. 2013; 22(2): 509-16.
19. Guimarães PAMP, Neto MS, Abla LEF, Veiga DF, Lage FC,
Ferreira LM. Sexualidade após mamoplastia de aumento. Rev Bras Cir Plast.
2015; 30(4): 552-559.
20. Guedes TSR. Imagem Corporal de Mulheres Submetidas Ao Tratamento Do
Câncer De Mama. Natal. Tese [Mestrado em Saúde Coletiva] -
Universidade Federal do Rio Grande do Norte; 2016
21. Alves VL, Sabino Neto M, Abla LEF, Oliveira CJR, Ferreira LM.
Avaliação precoce da qualidade de vida e autoestima de pacientes
mastectomizadas submetidas ou não à reconstrução
mamária. Revista Brasileira de Cirurgia Plástica.
2017;32(2):208-17
22. Martins TNDO, Santos LFD, Petter GDN, Ethur JNDS, Braz MM, Pivetta
HMF. Reconstrução mamária imediata versus não
reconstrução pós-mastectomia: estudo sobre qualidade de
vida, dor e funcionalidade. Fisioter. Pesqui. 2017; 24(4):
412-19.
23. Villar RR, Fernandez SP, Garea CC, Pillado MTS, Barreiro VB, Martin
CG. Qualidade de vida e ansiedade em mulheres com câncer de mama antes e
depois do tratamento. Rev Latino-Am Emfermagem. 2017; 25:
e2958.
24. Casassola GM, Stallbaum JH, Pivetta HMF. Satisfação
com cirurgia oncológica da mama: Comparação entre pacientes
mastectomizadas com e sem reconstrução mamária. SIEPE
[Internet]. 14º de fevereiro de 2020 [citado 20º de novembro de
2020];10(3). Disponível em: https://periodicos.unipampa.edu.br/index.php/SIEPE/article/view/87256
25. Archangelo SDCV, Neto MS, Veiga DF, Garcia EB, Ferreira LM.
Sexuality, depression and body image after breast reconstruction. Clinics. 2019;
74:e883.
26. Cosac OM, Campos AC, Dias RCS, Costa RSC, Da-Silva SV, Damasio AA,
et al. Reconstrução mamária: estudo retrospectivo de 16
anos. Rev Bras Cir Plast. 2019; 34(2): 210-7.
27. Volkmer C, Santos EKA, Erdmann AL Sperandio FR, Backes MTS,
Honório GTS. Reconstrução mamária sob a ótica
de mulheres submetidas à mastectomia: uma metaetnografia. Texto &
Contexto Enfermagem. 2019; 28: e20160442.
28. Carneiro MSF, Pinheiro CPO, Feitosa FVV, Soares MN, Rabelo IV, Lebre
P, et al. Repercussões psicológicas da cirurgia plástica em
mulheres mastectomizadas. Braz J of Develop. 2020; 6(7):
47743-51.
29. Ng SK, Hare RM, Kuang RJ, Smith KM, Brown BJ, Hunter-Smith DJ.
Breast Reconstruction Post Mastectomy: Patient Satisfaction and Decision Making.
Ann Plast Surg. 2016; 76(6): 640-4.
30. Zhong T, Temple-Oberle C, Hofer S, Beber B, Semple J, Brown M, et
al.; MCCAT Study Group. The Multi Centre Canadian Acellular Dermal Matrix Trial
(MCCAT): study protocol for a randomized controlled trial in implant-based
breast reconstruction. Trials 2013, 14: 356.
31. Brasil. Lei n. 9.797, de 06 de maio de 1999. Dispõe sobre a
obrigatoriedade da cirurgia plástica reparadora da mama pela rede de
unidades integrantes do Sistema Único de Saúde - SUS nos casos de
mutilação decorrentes de tratamento de câncer.
Diário Oficial da União. 06 mai 1999.
32. Brasil. Lei n. 13.770, de 19 de dezembro de 2018. Altera as Leis n
º 9.656, de 3 de junho de 1998, e 9.797, de 6 de maio de 1999, para
dispor sobre a cirurgia plástica reconstrutiva da mama em casos de
mutilação decorrente de tratamento de câncer. Diário
Oficial da União. 19 dez 2018.
33. Instituto Nacional de Câncer (INCA). Câncer de mama:
vamos falar sobre isso?[site]. Rio de Janeiro: INCA; 2019 [acesso em 29 nov
2020]. Disponível em: https://www.inca.gov.br/campanhas/outubro-rosa/2015/cancer-de-mama-vamos-falar-sobre-isso
34. Crippa CG, Hallal ALC, Dellagiustina AR, Traebert EE, Gondin G,
Pereira C. Perfil clínico e epidemiológico do câncer de
mama em mulheres jovens. Arquivos Catarinenses de Medicina. 2003; 32(3):
50-8.
35. Santos LS, Diniz, GRS. Saúde mental de mulheres donas de
casa: um olhar feminista-fenomenológico-existencial. Psicologia
Clínica, 2018, 30(1): 37-59.
36. Correia KML, Borloti E. Mulher e Depressão: Uma
Análise Comportamental-Contextual. Acta comport., 2011; 19(3):
359-73.
37. Oliveira JO, Peruch MH, Gonçalves S, Haas P. Padrão
hormonal feminino: menopausa e terapia de reposição. Revista
Brasileira de Análises Clínicas, 2016; 48(3):
198-210.
38. Brasil. Parecer técnico Nº 23/GEAS/GGRAS/DIPRO/2018.
Cobertura: procedimentos diversos - mama e sistema linfático
(mastectomia/ mastoplastia). Agência Nacional de Saúde
Suplementar. 2018.
1. Dynamic College of Vale Do Piranga, Ponte Nova,
MG, Brazil.
Corresponding author: Lúcia Meirelles
Lobão, Rua G, nº 205, Paraíso, Ponte Nova, MG,
Brasil, Zip Code 35430-302, E-mail:
lucia.fadip@gmail.com
Article received: April 09, 2021.
Article accepted: July 14, 2021.
Conflicts of interest: none.
Institution: Dynamic Faculty of Vale do Piranga, Ponte Nova, MG, Brazil.