INTRODUCTION
Rhinoplasty is the surgery indicated for performing aesthetic repairs in the
nose, being functional when it aims to improve respiratory function. Its first
report was described in India, around 500 BC, by Sushruta, considered the father
of plastic surgery, who used various reconstructive techniques on individuals
who had their nose cut off. From this report, the techniques were improving more
and more, and publications about this procedure became common. In the late
1500s, Professor Gaspare Tagliacozzi showed the possibility of nasal
reconstruction using an arm flap; in the mid-1800s, Johann Friedrich
Dieffenbach’s textbook entitled “Operative surgery”
described techniques for reducing the size of the nose. Since then, rhinoplasty
has become increasingly refined based on theoretical and practical training
provided by trained professionals1.
Today, rhinoplasty is a widespread procedure. The evaluation of its results is
based on improving the quality of life and patient satisfaction, which also
depends on factors such as preoperative appearance, expectations and the
doctor-patient relationship, and adequate training2. According to Oni et al. (2011)3, more than half of the residency
program directors evaluated did not feel confident in the residents’
ability to perform rhinoplasty. Much of this is due to the absence of early
exposure and little training time4. Despite this, several techniques were introduced, such as
educational videos, simulations, studies on cadavers and clinical skills
laboratories, but the training base remains the master-apprentice relationship
in surgical procedures, which limits the resident’s development5. It is essential to emphasize
that many alternative educational tools involve high financial costs and
training in patients may face restrictions due to the lack of hospital structure
and resources for the procedure.
Rhinoplasty is considered the most difficult of all cosmetic surgeries, as the
nasal anatomy is highly variable, the procedure must correct form and function,
and the result must meet the expectations of patients6. Therefore, it is necessary to reinforce
surgical learners’ anatomical knowledge and technical skills, using
strategies to increase training time and tools that, preferably, are low-cost
and easily accessible.
OBJECTIVE
This article aims to present a synthetic, novel and practical model for training
in rhinoplasty techniques, developed to be easy to perform and low cost.
METHODS
The study was carried out at the University of Fortaleza (UNIFOR), in
Fortaleza/CE, from September 2020 to December 2020. All ethical aspects of the
research were followed and respected.
Figure 1 - Materials needed for making the model.
Figure 1 - Materials needed for making the model.
To assemble the proposed model, the following materials were used: hot glue,
basin, water, detergent, epoxy putty, spatulas for crafts, nose mold (Carnival
mask), suture threads and white acetic silicone (Figure 1). To color the parts of skin and cartilage, it is necessary
to use dye and a disposable cup and spoon.
The construction of the model was done in three stages
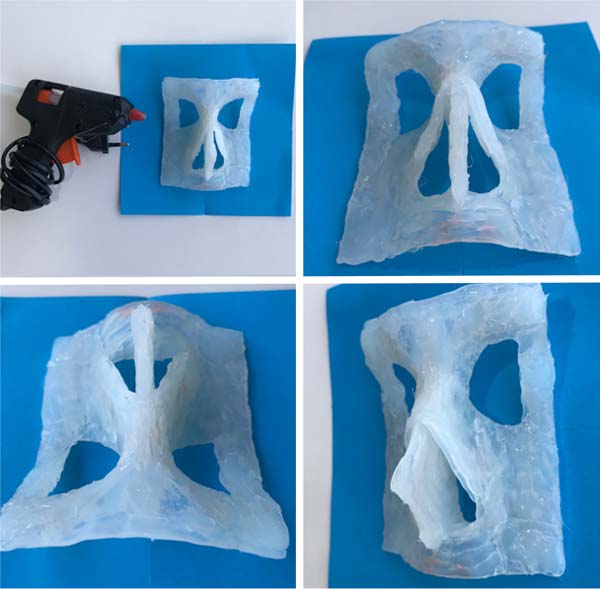
The bone structure of the face:
With hot glue, the structure was made in layers and molded while still hot in
the mask to replicate the bone structures of the face (Figure 2). The first nasal structure to be made was the
septum, followed by the nasal bones themselves.
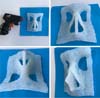
Cartilages
Cartilage construction was made from acetic silicone and an epoxy mass mold
(Figure 3). This mold was
handcrafted, simulating the shape of the upper and lower lateral cartilages
(Figure 4).
The epoxy putty was prepared and allowed to rest for 10 minutes to gain
sufficient consistency to be carved with the craft spatulas. After the mass
had dried, the silicone was poured into the mold and kept until it hardened.
Then, it was removed from the mold and placed in a ventilated place for
complete drying and reduction of the intense odor (Figure 5).
Figure 2 - Bone part made with hot glue.
Figure 2 - Bone part made with hot glue.
Figure 3 - Silicone cartilages and the material for their
manufacture.
Figure 3 - Silicone cartilages and the material for their
manufacture.
Figure 4 - Cartilage molds made of epoxy putty using a craft
spatula.
Figure 4 - Cartilage molds made of epoxy putty using a craft
spatula.
Figure 5 - Inferior lateral cartilages ready.
Figure 5 - Inferior lateral cartilages ready.
Skin
For confection, the dye was added to white acetic silicone in a disposable
container. Then, the mixture was placed in a basin with water and neutral
detergent, being kneaded and rolled by hand until, after a few minutes, a
slight hardening of the mass was observed (Figure 6).
Figure 6 - Ready-made leather and the materials needed for its
construction.
Figure 6 - Ready-made leather and the materials needed for its
construction.
The most consistent silicone was placed in a plastic mold similar to a nose
greased with oil and left to dry. Silicone has a powerful smell and, in
contact with the skin, can cause dry hands. So, protection with gloves and a
mask is essential.
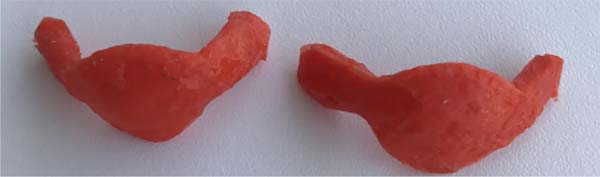
With the cartilages adequately dried, they were fixed to the bone structure
with suture threads (Figure 7). After
that, the skin was used to cover the structure and fixed with a suture to
remain immobile (Figure 8).
The skin was made to provide a better visual appearance to the model, as its
construction will not significantly influence the training period.
Figure 7 - Cartilages attached to the bone structure.
Figure 7 - Cartilages attached to the bone structure.
Figure 8 - Fixed skin covering the structure.
Figure 8 - Fixed skin covering the structure.
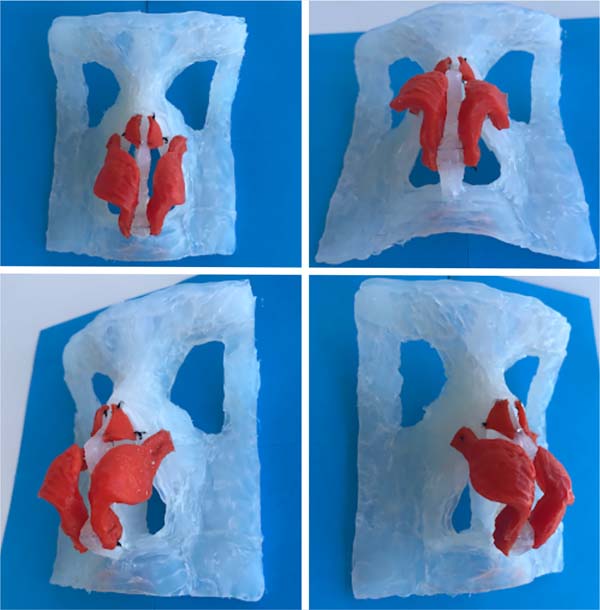
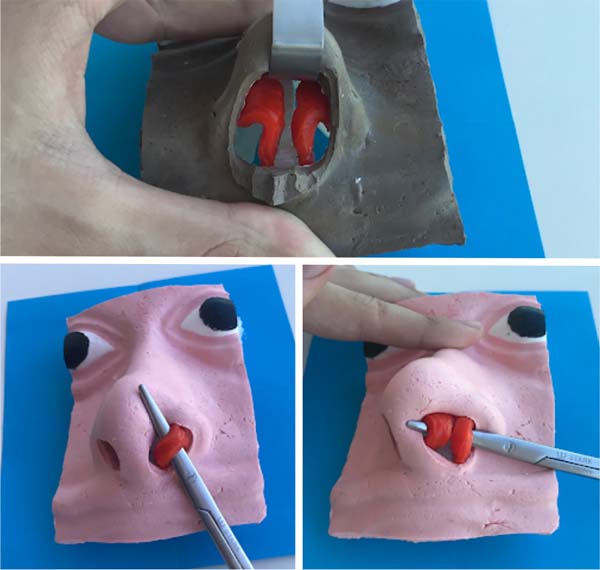
Figure 9 - Cartilage exposure using open and semi-open techniques.
Figure 9 - Cartilage exposure using open and semi-open techniques.
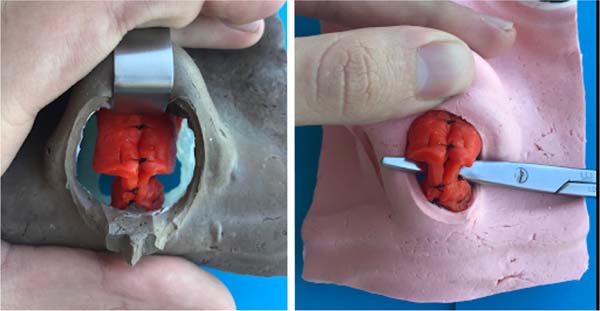
Figure 10 - Completion of the simulation using open and semi-open
techniques.
Figure 10 - Completion of the simulation using open and semi-open
techniques.
RESULTS
A format similar to the real one was obtained regarding the bone and
cartilaginous structure, as shown in the following images. In addition, color
differentiation between cartilages and nasal bones helps identify each structure
(Figure 9).
The complete structure allows for a very real rhinoplasty simulation, making it
possible to perform a columellar incision for open access and perform maneuvers
on the nasal tip and the back, such as the execution of sutures and the eventual
placement of grafts (Figure 10).
DISCUSSION
Surgical training involves complex practical and theoretical concepts, mainly
related to the surgical technique and its fundamental bases, among which the
development of skills is considered essential. In general, psychomotor skills
are acquired through the observational model, known as “see, do and
repeat”7.
In order to expand skills training beyond operating rooms, it is essential to
develop viable options with as much similarity as possible to the
patient’s tissue. An obvious option would be to study fresh cadavers, but
due to legal obstacles that make it challenging to obtain this material in
Brazil, it is still scarcely available8.
Some experimental models for training surgical skills related to rhinoplasty have
already been published, such as the animal model proposed by Dini et al.
(2012)8, which revealed
great applicability. However, the use of a non-human material also presents
several ethical and bureaucratic complications and does not show complete
similarity. Furthermore, there is a conflict with modern concepts of animal
welfare. Students’ misinformation about ethics and the use of animals,
associated with the obligation to participate in educational activities that use
this teaching method, without the legal right to conscientious objection or the
option of alternatives, have been related as a cause of desensitization
professionals9.
Therefore, the current diversity and complexity of medical-surgical knowledge
require a new direction in teaching through innovative strategies. Several
alternative precepts, also called “substitutives,” have been
exercised to ensure the acquisition of skills, seeking to fulfill the
educational/scientific function without harming the animals. The intention
should be to disseminate, at the ideal time, the knowledge necessary for
adequate professional training, enhancing learning and reducing or abolishing
the use of animals7.
The new synthetic model developed allows for excellent identification of
structures, adequate mobilization of nasal cartilages and easy handling of the
overlying synthetic skin, with consistency, texture and resistance similar to
the real thing. Allows good simulation of some steps of the open and semi-open
techniques of rhinoplasty. The upper and lower lateral cartilages made with
silicone, when sutured, provide a tactile sensation close to that of this
surgical stage in patients. Synthetic skin has a certain elasticity, like what
is observed when performing an open rhinoplasty. It should be noted that this
model has already been used in a hands-on course, at the XV North-Northeast
Congress of Otorhinolaryngology, in August 2019, when several surgeons were able
to learn about the model and realize its similarity to the real one.
In addition to all these technical characteristics of the model, it should be
noted that it does not raise ethical or legal questions that animal models or
training in fresh human corpses inevitably impose due to its synthetic nature.
In addition, another strong point is its low cost, which favors its replication
in medical schools. In this way, it can provide more time and training options
for apprentices in this refined surgery.
On the other hand, the main limitation of this model is that it requires
relatively complex manual skills for its construction. In addition, some steps,
for example, making the bone structure with hot glue, require some abstraction
capacity for construction, as there is no sketch of the three-dimensional shapes
of the face.
Finally, with the presentation of this model, the authors hope to make a relevant
contribution to medical education and, at the same time, encourage the emergence
of new models that improve it, based above all on the creative use of simple,
easily accessible materials and low cost.
CONCLUSION
The exposed model has the potential to positively impact the rhinoplasty learning
process, revealing itself as an accessible and helpful tool for training in the
various stages of the technique of this complex surgery.
REFERENCES
1. Lalwani AK. Otorrinolaringologia, cirurgia de cabeça e
pescoço: diagnóstico e tratamento. 3ª ed. São Paulo:
Artmed; 2013.
2. Esteves SS, Ferreira MG, Almeida JC, Abrunhosa J, Sousa CA.
Evaluation of aesthetic and functional outcomes in rhinoplasty surgery: a
prospective study. Braz J Otorhinolaryngol. 2017
Set/Out;83(5):552-7.
3. Oni G, Ahmad J, Zins JE, Kenkel JM. Cosmetic surgery training in
plastic surgery residency programs in the United States: how have we progressed
in the last three years?. Aesthet Surg J. 2011
Mai;31(4):445-55.
4. Wright EJ, Khosla RK, Howell L, Lee GK. Rhinoplasty education using
a standardized patient encounter. Arch Plast Surg. 2016
Set;43(5):451.
5. Dokuzlar U, Miman MC, Denizoğlu İİ,
Eğrilmez M. Opinions of otorhinolaryngology residents about their
education process. Turkish Arch Otorhinolaryngol. 2010
Set;53(3):100-7.
6. Daniel RK. Aesthetic reconstructive rhinoplasty. In: Daniel RK, ed.
Mastering rhinoplasty. Berlin: Springer Heidelberg; 2010. p.
407-40.
7. Martins Filho EF, Daleck CR, Costa Neto JM. Métodos
alternativos no ensino da técnica cirúrgica veterinária.
São Paulo: Universidade Estadual Paulista (UNESP); 2015.
8. Dini GM, Gonella HA, Fregadolli L, Nunes B, Gozzano R. Novo modelo
animal para treinamento de rinoplastia. Rev Bras Cir Plást.
2012;27(2):201-5.
9. Greif S, Tréz T. A verdadeira face da
experimentação animal: a sua saúde em perigo. Rio de
Janeiro: Sociedade Educacional Fala Bicho; 2000.
1. University of Fortaleza, Fortaleza, CE,
Brazil.
Corresponding author: Arthur Antunes Coimbra
Pinheiro Pacífico, Rua Mariana Furtado Leite 1250, apto 1201
torre 1 - Eng. Luciano Cavalcante, Fortaleza, CE, Brazil, Zip Code 60811-030,
E-mail: arthurh.pacifico@gmail.com
Article received: February 15, 2021.
Article accepted: April 19, 2021.
Conflicts of interest: none.
Institution: University of Fortaleza, Fortaleza, CE, Brazil.