INTRODUCTION
Currently, Brazil ranks second in the world ranking of plastic surgeries and
first in non-surgical procedures, according to the latest statistic from the
International Society of Aesthetic Plastic Surgery (ISAPS), in 2019. In the last
census carried out by the Brazilian Society of Plastic Surgery (SBCP -
Sociedade Brasileira de Cirurgia Plástica) from
20181, we found that
the most performed procedures are breast augmentation in the first place,
representing 18.8% of surgeries, followed by liposuction with 16.1%, abdominal
dermolipectomy with 15.9%, mastopexy with 11.3% and breast reduction with 9.9%
of procedures; equating with the reference of statistics worldwide.
Mammoplasty is an aesthetic and functional procedure aimed at replacing the
nipple-areola complex, reducing the size of the breasts, and improving its shape
with minimal scarring. However, there is no consensus on an ideal
technique2-5, justifying the diversity of
techniques described.
Patients who seek a mammoplasty do it intending to relieve physical and emotional
discomfort, according to Sabino Neto et al. (2008)6. When choosing the technique for successful
breast surgery, we must reflect between the shape and the final scar3-5 and consider several important points in the assessment:
the type of breast, shape, size and degree of ptosis. Decide on the type of
areolopapillary pedicle (superior, inferior, lateral, medial, or central) in
gland resection (medial, lateral, superior, inferior or peripheral). Analyze the
final scar whether inverted “T,” periareolar, vertical or
L5. Think about combined treatments with or without the inclusion
of prostheses, lipotransfer or use of laser, as well as considering skin and
scar care (drug delivery).
Instruments that assess patients’ satisfaction and quality of life are
increasingly used in breast surgeries, both aesthetic and reconstructive. The
PRO measures (patient-reported outcomes) offer the possibility of objectively
quantifying the results from the patient’s point of view.
Breast-QTM is a PRO-designed instrument, a questionnaire
considered to be an internationally known tool developed to assess the results
of breast surgeries, specifically to measure the quality of life and
satisfaction of patients undergoing this surgery7,8.
Spear et al. (2004)4 report that
after an analysis of 6 years in their practice, their indexes showed
post-surgical revisions in 54% of patients, for various reasons, the most common
being the desire for higher breasts.
Liposuction is the second most performed procedure globally, liposculpture that
remodels specific areas of the body, removing excess and often replacing fat in
areas of depression or restoring the convexity of a region. The objective of
liposuction is to leave the body harmonious (concave and convex), sometimes
following the musculature or eliminating shadow triangles (accumulations) and
leaving the light (convexity).
In the last three decades, new technologies such as ultrasound and laser were
developed to improve liposuction and used to increase the effectiveness, safety,
and reduce the time of the procedure, benefiting patients and surgeons without
neglecting the contour result.
In the literature, laser-assisted liposuction (LAL) was first described by
Dressed (1990) apud Apfelberg et al. (1994)9. Shortly after that, Apfelberg
et al. (1994, 1996)9,10 reported using a 1,064nm light
source during liposuction in 51 patients.
LAL photothermal energy melts fat11, making this procedure ideal for technically difficult
cases, such as fibrous areas in the breast, abdomen, back, male flanks10, and surgical revisions, where
the tissue is difficult to access or access presents irregularities12,13.
Compared with traditional liposuction (LT), LAL can reduce postoperative pain and
edema and hematomas14-18 due to thrombosis of blood
vessels and laser-induced closure of lymphatic channels18. Several studies demonstrate
the use of LAL, with good aesthetic results described, with an important skin
retraction, less blood loss, decreased physician fatigue, justified by the easy
emulsification of fat, which allows quick, efficient and less efficient
time13,18.
Other studies claim important collagen production stimulated by the heating of
the deep dermis and the connective septa of the subcutaneous tissues, inducing
collagen denaturation (neo-synthesis) and protein production, followed by
vascular proliferation19,20.
Jean et al. (2015)20 suggest
potential advantages of LAL over LT, preserving nerve endings and better blood
vessel clotting with less blood loss and mild ecchymosis.
The coagulation-modified collagen observed in microscopy could explain the great
aesthetic benefit in skin retraction, increasing its tone and texture, with
considerable improvement in flaccidity16,21,22. This is the specific clinical
indication that makes LAL a superior choice compared to TL14,22. LAL can also be considered a complement and, by some
colleagues, a substitute for traditional liposuction15. Regarding the learning curve, it is
indisputable that there is more specific training with LAL when compared to
LT15. Wolfenson et al.
(2015)23 described the
various regions that can be treated with (LAL): flanks (31.5%), face/submental
(28%), abdomen (19.5%), breasts (male) (14%) and other regions (7%).
In the literature, the LAL technique has also been used to treat
gynecomastia24; in a
study carried out by Kwang et al. (2015),24, 13 patients with gynecomastia underwent LAL. Before
the procedure, chest circumference measurements were recorded, and breast
thickness was controlled with CT images. Twelve weeks later, the patients were
again reviewed using the same measurements, and both the mean chest
circumference and breast thickness decreased significantly24. This type of study opened the
range of indications for LAL in different body regions and among them the
breast, not only for the treatment of gynecomastia but also as a supporting
procedure in reconstructive and aesthetic breast surgery.
LAL is based purely on a thermal effect13,17,23,25,26, the
following properties should be considered when determining the effectiveness of
laser lipolysis: the wavelength used and the energy released17, as well as the time applied
to the tissue. The laser light energy is converted into thermal energy inside
the adipose tissue; it diffuses to the dermis and probably to the skin surface,
reaching 48°C - 50°C to induce collagen contraction and
strengthening of the cutaneous tissue16,22. This
shrinkage effect is continuous and can be identified for up to 3 to 6 months
after the procedure12,22; therefore, continuous thermal
monitoring is necessary, as the damage directly depends on the applied
energy21,27.
According to Badin et al. (2005)12, in their study, 3,000 joules of energy per area resulted
in significant irreversible damage compared to an area treated with lower power
(1,000J). In other publications, adipocyte liquefaction, tissue carbonization
and epidermal damage were observed with higher energy settings22,27-29.
Seeking better results in the treatment of breasts and their recurrences, a
combination of considerations, adaptations and new technologies is acceptable.
The mirror “D” mammoplasty technique described by the
authors30,31, originally indicated for
primary mastopexy and inclusion of silicone implants in hypoplastic breasts
associated with moderate to severe ptosis. In this paper, we will present our
experience of a systematic procedure in all our breast surgeries to treat
primary and secondary mastopexies without implants, in association with LAL with
maintenance and satisfaction of results, and validation with the
Breast-QTM questionnaire.
OBJECTIVES
To present a reduction mammoplasty technique with the procedure’s
systematization, use of LAL, and maintenance of results validated with
Breast-QTM.
METHODS
We performed the lipomammoplasty technique using the mirrored
“D”7,8 and laser in 46 female patients,
without exclusion by race, aged between 20 and 66 years, operated by the authors
between January 2017 and March 2020. The authors performed the procedures at the
Hospital Antoninho da Rocha Marmo - São José dos Campos (CEP:
005/ADM/ARM/2020). The main complaint was breast ptosis. We used proper marking
to determine the areas of decortication, skin resection, medial bipartite flap,
assembly with crossed flaps and resection of the excess lateral flap to achieve
breast harmonization—the flap with medial pedicle and vertical scar as
the final result.
In all patients, to infiltrate and remove the emulsified fat, we used the
technique of vibrolipoaspiration with a device branded vibrolipoTM
registered by Anvisa.
Since 2015, in our In practice, we introduced the use of the DeligthTM
brand laser registered at Anvisa, which has two wavelengths that we use
according to the purpose of the treatment.
The laser at 915nm (for lipolysis) has selectivity on adipocytes, making the
converted heat absorbed by the fat, causing its emulsification and subsequent
excretion by the body.
In the laser at 980nm (for skin retraction), the selectivity is given by water,
whose intense heating causes the retraction of collagen and elastin fibers,
stimulating their regeneration and returning the tissue to a firm and delineated
appearance, a key effect for the treatment of flaccidity.
The infiltration must be carried out in the same region to be aspirated, always
in the intermediate subcutaneous layer (between the lamellar and areolar
layers).
All patients were evaluated weekly during the first month, monthly until the
sixth month and every three months until completing one year postoperatively
(PO). After that, every six months until completing 24 months PO. The
Brest-QTM questionnaire was applied preoperatively, at 12 months
and 24 months.
Surgical technique
1. Marking
Mirrored “D” technique
The marking of the patient is performed in the supine position and
arms close to the trunk. There is a difference of up to 1cm in the
breast crease when compared to the crease marked in the standing
position, which, in our experience, is reflected in a more
appropriate and natural shape in the final result. In this position,
the breasts naturally assume a symmetrical spatial adjustment,
easily visualized in the positioning of the nipple-areola plate
(NAP), canceling out the visible asymmetries in the orthostatic
position, justified by the action of the volume and gravity
binomial, which facilitates marking, resulting in naturally
occurring breasts symmetrical.
With the patient in the supine position, a midline is marked from the
sternal notch to the umbilical scar and the submammary crease,
formed naturally by the positioning of the breasts in decubitus
(Figure 1):
Figure 1 - Patient lying down with arms close to the body, marking
the midsternal line, submammary and ABCD points. Point A:
10cm from the inframammary fold and 9cm from the midsternal
line at the intersection of these lines, mark A. Point B:
10cm from the midsternal line in the submammary fold. Point
C: 3cm from Point A, on the straight line between A and B.
Point D: with bidigital maneuver considering maximum skin
resection and arch closure.
Figure 1 - Patient lying down with arms close to the body, marking
the midsternal line, submammary and ABCD points. Point A:
10cm from the inframammary fold and 9cm from the midsternal
line at the intersection of these lines, mark A. Point B:
10cm from the midsternal line in the submammary fold. Point
C: 3cm from Point A, on the straight line between A and B.
Point D: with bidigital maneuver considering maximum skin
resection and arch closure.
POINT A: This point is marked 10cm from the inframammary
crease and 9cm from the midsternal line; the place of the
intersection of these lines, we call point A.
POINT B: Considering the submammary crease naturally
formed in the decubitus, point B is marked at 10cm from the
midsternal line.
The union of points A and B determines the straight part of the
“D” design.
POINT C: Point C is marked 3cm from point A on the
straight-line joining A and B.
POINT D: With a bidigital block maneuver, point D
corresponding to the maximum point of skin resection is marked.
DRAWING of the “D”: The mirrored
“D” closure occurs by joining in a straight line
between points A and B, and an arc laterally, from point A to point
B, passing through D, including the areola superiorly, wherever it
is located and respecting the limit of point D for the lower
continuation of the arc.
The junction of points C and D at the end of the surgery will
coincide with the lower edge of the new positioning of the areola.
The beginning of the final vertical scar, which will be
approximately 6 to 7 cm in length to the inframammary fold, being
the point B is the end of the vertical scar, which provides
symmetrical parallel vertical scars due to the 1cm difference in the
marking between points A and B (Figure 1).
The mirror marking of the “D” on the other side is done
in the same way. The “D” arch is different in most
cases, depending on the asymmetry of the breasts.
Laser-Assisted Liposuction (LAL) technical
marking
We divided the breast into four quadrants and marked the excess fat
in the breast extension (anterior axillary line to posterior
axillary line), including the axillary region (Figure 2).
Figure 2 - Lipolaser breast marking - marking the quadrants
according to
Tables 2
and
3. A 36-year-old
patient with results after six weeks of lipomammoplasty,
with the “D” technique + lipoadominoplasty
with LAL.
Figure 2 - Lipolaser breast marking - marking the quadrants
according to
Tables 2
and
3. A 36-year-old
patient with results after six weeks of lipomammoplasty,
with the “D” technique + lipoadominoplasty
with LAL.
2. Infiltration used
We infiltrate with the vibrolipo with a Klein 4mm cannula; we always
recommend that it is wet with a solution of 1,000ml of saline solution +
4 ampoules of adrenaline (1:250,000).
3. Laser-Assisted Liposuction (LAL)
It is important to emphasize that we never aspire to the superior
interior quadrant. We applied lipolaser in the superior and inferior
external and inferior interior quadrants (Tables 1 and 2). In contrast, the vibrolipo is performed in the superior
and inferior exterior quadrants, respecting the inferior interior.
Table 1 - Laser application: 915nm (lipolysis).
| Region |
Power |
| Superior exterior quadrant |
2000J |
| Inferior exterior |
1000J |
| Inferior interior |
1000J |
| Breast extension |
1000J |
| Total energy used 915nm 25W of power |
5000J |
Table 1 - Laser application: 915nm (lipolysis).
Table 2 - Application of laser: 980nm (skin retraction).
| Region |
Power |
| Superior exterior quadrant + exterior
inferior
|
3000J |
| Inferior interior |
500J |
| Breast extension |
1000J |
| Total energy used 980nm 25W of
potency
|
4500J |
Table 2 - Application of laser: 980nm (skin retraction).
Procedure steps and care
a. We use skin protectors.
b. The fiber must always be introduced into the fat tissue in the
intermediate plane, tunneling the tissue (Figure 3). If the fiber is superficial, there
is a risk of burning, and if it is too deep, in addition to losing
the plane, it may have the risk of affecting organs. In
inexperienced hands, it is very easy to transfix the fascia or the
pleura in the thoracic region.
c. Always follow the fiber light(Figure 3). When the light is barely visible, it is in a
deep plane; if it is very strong, it is in a superficial plane.
Figure 3 - Quadrant liposuction with LAL following the light for
plan treatment.
Figure 3 - Quadrant liposuction with LAL following the light for
plan treatment.
d. The fiber should always be parallel to the skin tissue.
e. The infiltration needs to be moist; we do not recommend tumescent,
as it could lose the result of skin retraction.
f. Infiltration plan: infiltrate in the intermediate plan, which is
the same plan we apply LAL.
g. At any sign of vascular alteration of the tissue, take the
following measures: we use moist compresses and apply a cream with
flavonoids in the affected region, helping the tissue flow (linfa
creamTM registered at Anvisa), improving edema, pain
and hyperchromic stains, in case of hematomas due to hemosiderin
accumulation. We also prescribe for home use. We use this product in
all our surgical procedures in the immediate postoperative period
(dressing).
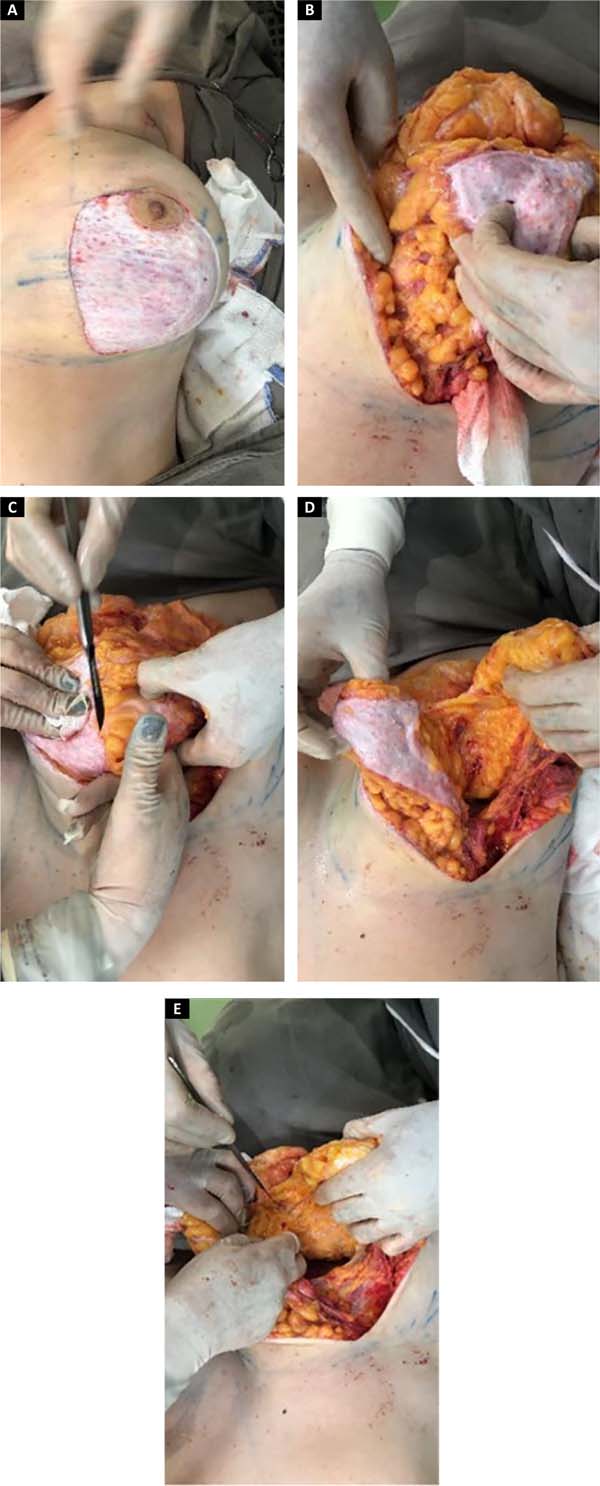
4. Technique in “D”: procedure
Schwartzman Maneuver:
The surgery begins with marking the areola with a 4cm areolotome,
followed by decortication of the skin over the tissue, in the
extension of the marking of the “D” (Figure 4A).
Making the flap p. medial:
The medial flap is marked with a 5cm base and at least 1cm around the
areola. The tissue is detached, maintaining a thickness of +2cm from
the lateral edge to the base of the flap (Figure 4B).
Split flaps:
It starts with the demarcation from the “D” to the
subcutaneous tissue and subsequent detachment of the skin with a
dermofat flap of approximately 2cm, following a plane below the
lipolaser and close to the breast parenchyma to the anterior
axillary line and medially to the parasternal line. We continued
with constructing a subglandular pocket, preserving the parenchyma
implantation at point B and following the AB line to the second
costal arch superiorly, avoiding wide detachment and thus creating
only a central tunnel, maintaining the medial implantation of the
breast. After gland release, we started making bipartite flaps,
using the “D” arch to define the beginning of the
perpendicular dissection up to the muscle fascia, thus preserving
the “D” arch and decorticated in the medial flap
(Figures 4C, D and E).
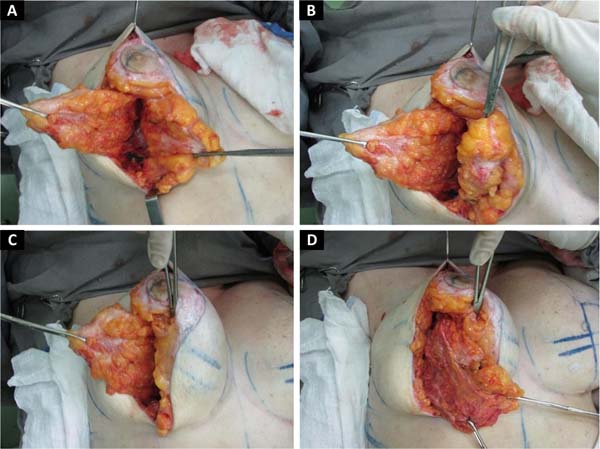
Mounting:
The medial flap is folded over itself, supero medially. Keeping the
insertion of the parenchyma at point B (Figures 5A,5B and 5C). The
lateral flap is pulled medially inferiorly, towards the xiphoid
appendix (Figure 5D). All
parenchyma beyond the AB line is resected; we continue with the
inferolateral resection, thus creating the new inframammary
fold.
Figure 4 - A: Schwartzman Maneuver; B:
Making a medial flap; C, D, and E:
Internal flap release in the “D” arch and flap
splitting preserving the parenchymal insertion at point B,
going to the second intercostal arch, and tunneling the
dissection.
Figure 4 - A: Schwartzman Maneuver; B:
Making a medial flap; C, D, and E:
Internal flap release in the “D” arch and flap
splitting preserving the parenchymal insertion at point B,
going to the second intercostal arch, and tunneling the
dissection.
Figure 5 - A: Bipartite lateral (external) and medial
(internal) flaps; B: With an Allys forceps, we
rotate the medial flap on itself superomedial.
C: Medial flap maintaining its insertion in
the parenchyma coinciding with point B; D:
Inferomedial tractioned lateral flap prepared for
resection.
Figure 5 - A: Bipartite lateral (external) and medial
(internal) flaps; B: With an Allys forceps, we
rotate the medial flap on itself superomedial.
C: Medial flap maintaining its insertion in
the parenchyma coinciding with point B; D:
Inferomedial tractioned lateral flap prepared for
resection.
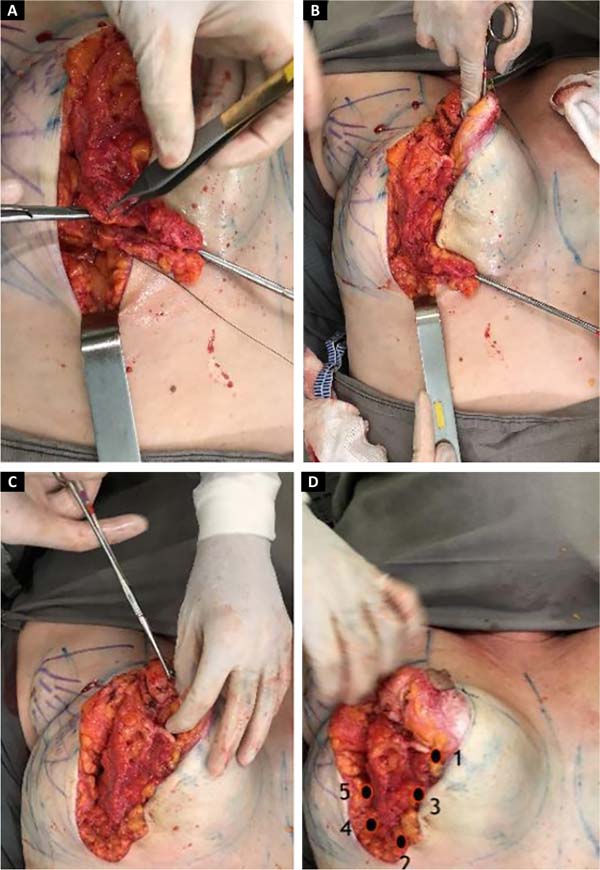
The medial flap will be the same on both sides, and the lateral flap
will vary upon resection, depending on previous breast asymmetry;
resected in bands (Figures 6A
and 6B).
Sutures with five fixation points:
Suture of the breast parenchyma is performed with 2.0 mononylon
thread, joining the stitches with inferomedial traction of the
lateral portion for medialization of the same:
First point: approaching the medial pillars and lateral at the
junction of points CD, (beginning of the column);
Second point: keeping the medial traction, joining the parenchyma
with the fascia of the m. serratus at point B level coinciding with
the beginning of the inframammary fold (end of the spine);
Third point: performed on the middle of the AB line between the first
and second points, used for lateral support of the spine;
Fourth and fifth points: fixing the lateral parenchyma with the
muscle fascia, defining the end of the new inframammary fold (Figure 6).
After fixation, closure is continued by planes, mononylon 3.0
superficial parenchyma, colorless mononylon 4.0 subcutaneous and,
finally, intradermal with 4.0 monocryl (Figure 7).
Areola marking:
The junction of points C and D will coincide with the lower edge of
the new positioning of the areola and the beginning of the vertical
scar (Figure 8).
Figure 6 - A: The lateral flap is pulled and resected
in bands, placing the fixation points between the lateral
and medial flap, which is already in rotation, point 1
brings the pillars closer to the CD marking, point 2 at the
level of point B tractioning the end of the spine;
B: Point 3 in the middle of AB between the
first and second point; points 4 and 5 to define the
submammary fold, performed in the lateral parenchyma in the
muscle fascia; C: Removal of Allys from the
medial flap that remains fixed; D: Conical
harmonic shape with good upper pole contour after assembly
as described in point numbering.
Figure 6 - A: The lateral flap is pulled and resected
in bands, placing the fixation points between the lateral
and medial flap, which is already in rotation, point 1
brings the pillars closer to the CD marking, point 2 at the
level of point B tractioning the end of the spine;
B: Point 3 in the middle of AB between the
first and second point; points 4 and 5 to define the
submammary fold, performed in the lateral parenchyma in the
muscle fascia; C: Removal of Allys from the
medial flap that remains fixed; D: Conical
harmonic shape with good upper pole contour after assembly
as described in point numbering.
Figure 7 - Final skin closure, nipple-areola marking.
Figure 7 - Final skin closure, nipple-areola marking.
Areola suture in two planes, subcutaneous with mononylon 4-0
colorless and intradermal with monocryl 4.0.
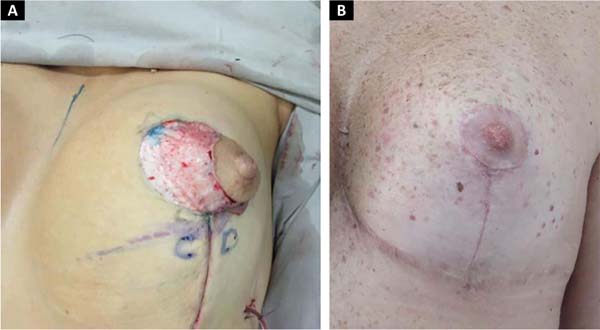
Figure 8 - A: Vertical closure and nipple-areola
complex marking that coincides on the CD of the initial
marking, B: Final areola and vertical
healing.
Figure 8 - A: Vertical closure and nipple-areola
complex marking that coincides on the CD of the initial
marking, B: Final areola and vertical
healing.
Drain:
Portovac 3.2, introduced in the midaxillary line, below the new
inframammary fold, is located between the parenchyma and the
dermofat flap and removed on the second postoperative day.
Dressing:
Dry, performed with X-shaped crisscross micropore strips, directly
over the scar, maintained for seven days.
RESULTS
Surgical revision was not required in any of the cases presented. There was no
occurrence of post-surgical infection or necrosis of the papillary areolar
plaque and the scar.
There were 5 cases of epidermolysis of the papillary areolar plaque, successfully
treated with flavonoids and horse chestnut (linfa cream -
Claremom), without sequelae.
The average resection of the parenchyma was 477.1g ranging from 80 to 1100g.
The amount of liposuction (LAL) was on average 438.6ml between 150 to 790ml.
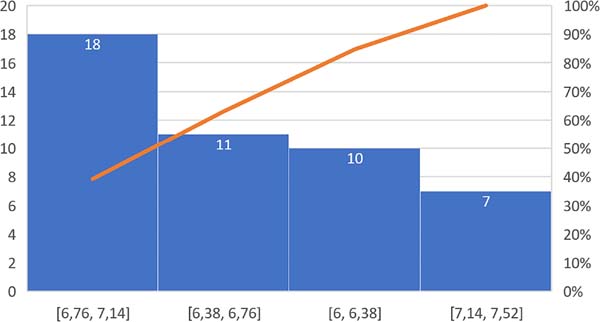
The length of the vertical scar was stable at an average of 6.7 cm (between
6.1-7.5) after two years (Figure 9).
The results with this technique were considered satisfactory, validated with the
Breast-QTM questionnaire, reduction/mastopexy module (pre and
postoperative), the evaluation percentages were described in Table 3.
Currently, the combination with laser is used in all our breast procedures and
body treatment (abdomen, buttocks, arms, thighs and face/submental). Its
combination brought us greater benefits in terms of surgical time and results
(Figures 2, 10 and 11).
Figure 9 - Study group with age of patients and final vertical scar.
Figure 9 - Study group with age of patients and final vertical scar.
Table 3 - Summary of the Breast-QTM questionnaire in the 46 patients
studied.
| Postoperative module |
Very
satisfied
|
88% |
| Result of your surgery |
I totally agree |
72% |
| How
do you feel after surgery
|
All
the time
|
82% |
| How often do you feel |
Most of the time |
83% |
| Last
two weeks
|
in no
time
|
96% |
| Information obtained from your
surgeon
|
Very satisfied |
74% |
| Satisfaction |
Very
satisfied
|
86% |
| About your plastic surgeon |
Completely agree |
73% |
| About
the medical team
|
Completely agree |
92% |
| Office professionals |
Completely agree |
92% |
Table 3 - Summary of the Breast-QTM questionnaire in the 46 patients
studied.
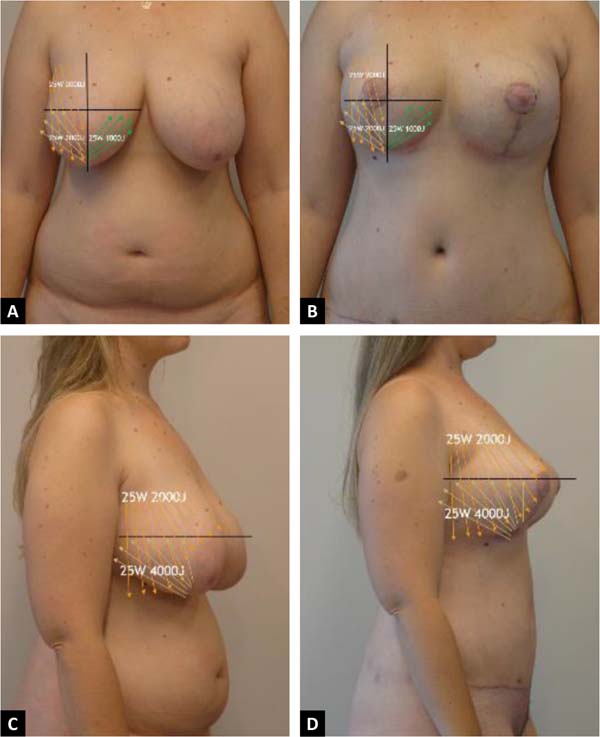
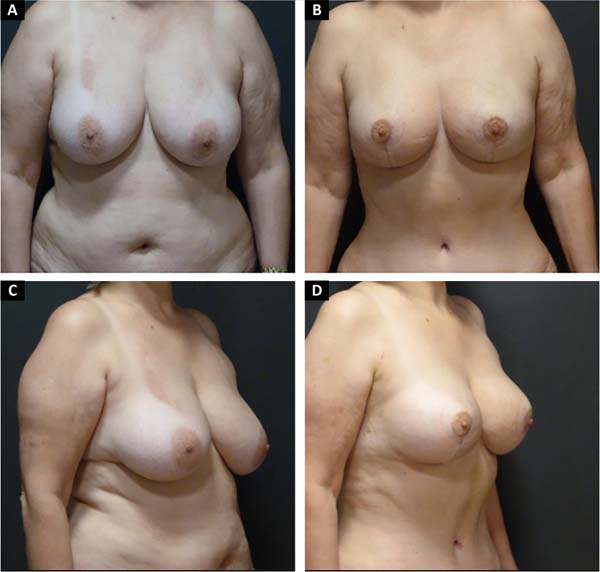
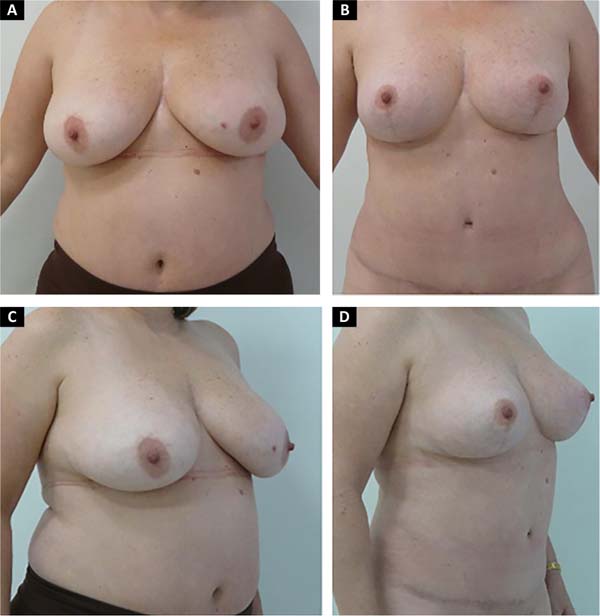
Figure 10 - A. 60-year-old patient preoperatively after lipomammoplasty with LAL
and mirrored “D” technique + abdominoplasty anterior view;
B. 1 year of PO; C. Preoperative - side view;D. with one year of
PO.
Figure 10 - A. 60-year-old patient preoperatively after lipomammoplasty with LAL
and mirrored “D” technique + abdominoplasty anterior view;
B. 1 year of PO; C. Preoperative - side view;D. with one year of
PO.
Figure 11 - A.48-year-old patient preoperatively after lipomammoplasty with LAL
and “D” technique mirrored anterior view; B. 2-year
postoperative period;C. Preoperative - side view; D. 2-year
postoperative period - lateral view.
Figure 11 - A.48-year-old patient preoperatively after lipomammoplasty with LAL
and “D” technique mirrored anterior view; B. 2-year
postoperative period;C. Preoperative - side view; D. 2-year
postoperative period - lateral view.
DISCUSSION
The mirrored “D” technique has been used for 15 years, showing
benefits such as reducing the tension of the papillary areolar plate (PAP) and,
mainly, parallel vertical scars7,8. With the
association of laser liposuction since 2015, with an improvement in the
definition of the inframammary fold and a reduction in breast changes.
Its aesthetic results with smaller scars regardless of breast size, with an
average final vertical scar of 6.7cm after two years of follow-up, and a
reduction in breast ptosis recurrences, strengthen what has been described in
the literature.
The degree of patient satisfaction was an important benefit for the advancement
of the technique, especially concerning harmony, homogeneous skin retraction and
better breast contour. The maintenance of the results was longer lasting when
compared to the results obtained with other vertical scar techniques previously
performed in our service, with a degree of satisfaction of very satisfied,
representing 86% in the questionnaire applied (Breast-QTM).
Statistically combined surgeries present greater complications compared to
isolated surgeries, which is a controversy among authors. With the mirrored
“D” technique, we found a significant reduction in complications,
especially in surgical revision, compared to 54% found in the
literature4, an
important factor that favored the evolution, maintenance and indication of the
technique.
The amount of energy applied in the wrong way in the same place can produce
direct damage to the fat and skin tissue. In our experience, we recommend not
using more than 4000J per region. The poor clinical indication of energy (LAL)
in the different areas and the surgeon’s lack of experience and learning
in performing the laser could bring serious complications, which can be
prevented. And it is also important to have a good evaluation of the fat tissue,
its diameter, and the quality and type of skin in the region to be treated.
CONCLUSION
The mirrored “D” technique proved to be a good surgical option due
to its versatility in different mammoplasty scenarios.
Its ease of execution has increased its indications for all types of breast
ptosis, primary or secondary mammoplasty, with or without implants.
The combination of the mirrored “D” technique with laser-assisted
liposuction is a procedure that is considered routine in our surgical planning
every day—resulting in significant homogeneous skin retraction, favoring
the conical shape of the breast, and maintaining the validated results.
REFERENCES
1. Sociedade Brasileira de Cirurgia Plástica (SBCP). Censo 2018
- Análise comparativa das pesquisas 2014, 2016 e 2018 [Internet].
São Paulo: SBCP; 2018. Disponível em: http://www2.cirurgiaplastica.org.br/wp-content/uploads/2019/08/Apresentac%CC%A7a%CC%83o-Censo-2018_V3.pdf
2. Souza Pinto EB, Erazo I, Muniz AC, Prado Filho FS, Alves MA, Salazar
GH. Breast reduction: shortening scars with liposuction. Aesthetic Plast Surg.
1996 Nov/Dez;20(6):481-8.
3. Spear SL. Augmentation/mastopexy: surgeon, beware. Plast Reconstr
Surg. 2006;118(Supl 7):133S-5S.
4. Spear SL, Pelletiere CV, Menon N. One-stage augmentation combined
with mastopexy: aesthetic results and patient satisfaction. Aesthetic Plast
Surg. 2004 Set/Out;28(5):259-67.
5. Cárdenas-Camarena L, Ramírez-Macías R.
Augmentation/mastopexy: how to select and perform the proper technique.
Aesthetic Plast Surg. 2006 Jan/Fev;30(1):21-33.
6. Sabino Neto M, Demattê MF, Freire MAMS, Garcia EB, Quaresma
M, Ferreira LM. Self-esteem and functional capacity outcomes following reduction
mammaplasty. Aesthet Surg J. 2008;28(4):417-20.
7. Sbalchiero JC, Cordanto-Nopoulos FR, Silva CHD, Caiado Neto BR,
Derchain S. Tradução do questionário Breast-Q para a
língua portuguesa e sua aplicação em mulheres com
câncer de mama. Rev Bras Cir Plást.
2013;28(4):549-52.
8. Andrade AC. Breast-Q® na avaliação de
resultados da mamoplastia redutora [dissertação]. São Paulo
(SP): Universidade Federal de São Paulo (USP) - Escola Paulista de
Medicina; 2015.
9. Apfelberg DB, Rosenthal S, Hunstad JP, Achauer B, Fodor PB. Progress
report on multicenter study of laser-assisted liposuction. Aesthetic Plast Surg.
1994;18(3):259-64.
10. Apfelberg DB. Results of multicenter study of laser-assisted
liposuction. Clin Plast Surg. 1996 Out;23(4):713-9.
11. Katz B, McBean J. Laser-assisted lipolysis: a report on
complications. J Cosmet Laser Ther. 2008 Dez;10(4):231-3.
12. Badin AZED, Gondek LBE, Garcia MJ, Garcia MJ, Valle LC, Flizikowski
FBZ, et al. Analysis of laser lipolysis effects on human tissue samples obtained
from liposuction. Aesthetic Plast Surg. 2005;29:281-6.
13. Goldman A. Submental Nd:YAG laser-assisted liposuction. Lasers Surg
Med. 2006 Mar;38(3):181-4.
14. Goldman A, Gotkin RH. Laser-assisted liposuction. Clin Plast Surg.
2009 Abr;36(2):241-53.
15. Badin AZD, Moraes LM, Gondek L, Chiaratti MG, Canta L. Laser
lipolysis: flaccidity under control. Aesthetic Plast Surg. 2002
Set/Out;26(5):335-9.
16. Parlette EC, Kaminer ME. Laser-assisted liposuction: here’s
the skinny. Semin Cutan Med Surg. 2008 Dez;27(4):259-63.
17. Sun Y, Wu SF, Yan S, Shi HY, Chen D, Chen Y. Laser lipolysis used to
treat localized adiposis: a preliminary report on experience with Asian
patients. Aesthetic Plast Surg. 2009 Set;33(5):701-5.
18. Reynaud JP, Skibinski M, Wassmer B, Rochon P, Mordon S. Lipolysis
using a 980nm diode laser: a retrospective analysis of 534 procedures. Aesthetic
Plast Surg. 2009 Jan;33(1):28-36.
19. Rocha RP, Pinto EBS, Saldanha OR, Rocha ELP, Missel J. Estudo
histológico da derme humana de interesse para a
lipoaspiração. Rev Bras Cir Plást.
2005;20(1):17-21.
20. Jecan CR, Hernic AD, Tianu EC, Florescu IP, Lascar I. Histological
differences between laser-assisted and suction-as- sisted lipoplasty
aspirates—a comparative study. Rom J Morphol Embryol. 2015;56(Supl
2):S797-S801.
21. Kim KH, Geronemus RG. Laser lipolysis using a novel 1064 nm Nd:YAG
laser. Dermatol Surg. 2006 Fev;32(2):241-8.
22. DiBernardo BE, Reyes J, Chen B. Evaluation of tissue termal effects
from 1064;1320-n laser assisted lipolysis and its clinical implications. J
Cosmet Laser Ther 2009;11(2):62-9.
23. Wolfenson M, Hochman B, Ferreira LM. Laser lipolysis: skin
tightening in lipoplasty using a diode laser. Plast Reconstr Surg. 2015
Mai;135:1369-77.
24. Yoo KW, Bae JM, Won CY, Chung YS, Goo B, Rho YK, et al.
Laser-assisted liposuction using the novel 1,444-nm Nd:YAG laser for the
treatment of gynecomastia: a pilot study. Dermatology. 2015;231(3):224-30. DOI:
https://doi.org/10.1159/000430494:2015
25. Mordon S, Blanchemaison PH. Histologic evaluation of interstitial
lipolysis comparing a 1064, 1320 and 2100 nm laser in an ex vivo model. Lasers
Surg Med. 2008 Out;40(8):519.
26. Reszko AE, Magro CM, Diktaban T, Sadick NS. Histological comparison
of 1064 nm Nd:YAG and 1320 nm Nd:YAG laser lipolysis using an ex vivo model. J
Drugs Dermatol. 2009 Abr;8(4):377-82.
27. Mordon S, Eymard-Maurin AF, Wassmer B, Ringot J. Histologic
evaluation of laser lipolysis: pulsed 1064-nm Nd:YAG laser versus CW 980-nm
diode laser. Aesthetic Surg J. 2007;27(3):263-8.
28. Khoury JG, Saluja R, Keel D, Detwiler S, Goldman MP. Histologic
evaluation of interstitial lipolysis comparing a 1064, 1320, and 2100 nm laser
in an ex vivo model. Lasers Surg Med. 2008 Ago;40(6):402-6.
29. Ichikawa K, Miyasaka M, Tanaka R, Tanino R, Mizukami K, Wakaki M.
Histologic evaluation of the pulsed Nd:YAG laser for laser lipolysis. Lasers
Surg Med. 2005 Jan;36(1):43-6.
30. Sanchéz J, Carvalho AC, Erazo P. Mastoplasty with prosthesis:
the mirror D technique. Rev Bras Cir Plást.
2008;23(3):200-6.
31. López JCS, Erazo P. Secondary mastopexy with exchange of
prosthesis: mirror “D” technique. Rev Bras Cir Plást.
2018;33(3):324-32.
1. Juan Sánchez Clinic, São
José dos Campos, SP, Brazil.
2. Plastic Surgery Clinic Dr. Patricia J. Erazo,
Santos, SP, Brazil.
Corresponding author: Patricia Jacqueline
Erazo, Rua Santa Clara nº 1035, Vila adyana, São
José dos Campos, SP, Brasil, Zip Code 12243 630, E-mail:
p.erazo@uol.com.br
Article received: April 22, 2020.
Article accepted: July 14, 2021.
Conflicts of interest: none.
Institution: Hospital Antoninho da Rocha Marmo, São José dos
Campos, SP, Brazil.