INTRODUCTION
The breasts are probably the greatest symbol of femininity in the human race and
cause great discomfort to the social life of male transsexuals, who were born in
the female gender and identify themselves as the opposite gender, which we
conventionally diagnose as dysphoria1,2. The incidence
of transsexualism varies greatly depending on the sources, most ranging between
0.5% and 1.5%1,3.
With the dissemination of information among the patients themselves through the
internet and social media, there has been greater awareness of the topic, as
well as the demand for psychotherapy, hormone therapy and surgical treatments,
carried out by various professionals for social and psychological guidance,
masculinization of the characteristics primary and secondary sexual: plastic
surgeons, dermatologists, endocrinologists, gynecologists, urologists, breast
cancer specialists, psychologists, social workers, among others1.
The objectives of this surgical procedure are: to remove breast tissue and excess
skin, reduce and correctly reposition the CAP, try to minimize loss of
sensation, flatten the inframammary fold, minimize scars on the chest wall and
create an aesthetically pleasing male chest contour, preferably in a single
surgical time2,3.
OBJECTIVES
This paper presents the author’s experience with a technique of
masculinizing mastectomy (MM) performed in male transsexual patients (female to
male), called double incision associated with a free graft of papillary areolar
complex (DIEL-CAP).
METHODS
Study design
Retrospective cross-sectional study.
Casuistry
Between November 2013 and January 2018, 26 patients from his private clinic
in Sorocaba/SP. were submitted to masculinizing mastectomies (a total of 52
breasts), performed by the technique proposed by the author.
Six months was the minimum follow-up time to be included in this work.
Surgical procedure
The maximum hospital stay was thirty hours. All masculinizing mastectomies
were performed under general anesthesia.
1. Preoperative markings are performed with the patient’s trunk around
sixty degrees of inclination, starting with an inferior horizontal line
along the inframammary fold (Figure 1)
and the midclavicular line;
2. Next, the upper horizontal incision line is drawn on the skin above the
areola, evaluated using the pinch test. When the breast does not have enough
skin leftover for the complete descent of the upper flap, the marking of
this upper line is performed during the surgical procedure, which may
eventually evolve with a final inverted “T” scar, in smaller
breasts and with less flaccidity;
Figure 1 - Preoperative marking.
Figure 1 - Preoperative marking.
3. The surgical procedure is performed with the patient in horizontal dorsal
decubitus with open arms;
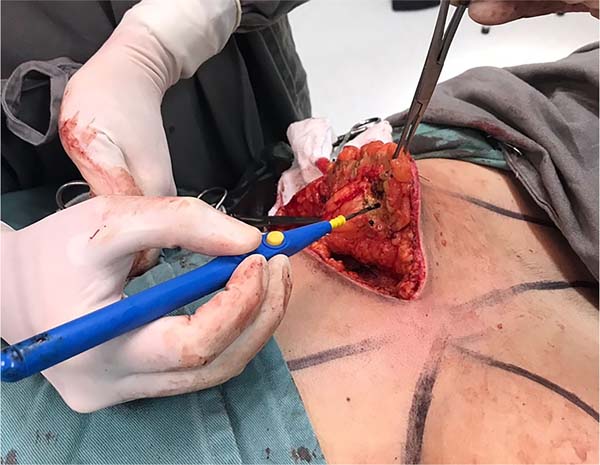
4. The operation begins with the collection of a full-thickness NAC graft
with a diameter of 2.5 cm, from the central region of the breast areola,
with a scalpel blade (Figure 2);
Figure 2 - APC collection for grafting.
Figure 2 - APC collection for grafting.
5. The incision begins in the inframammary fold and, later, in the upper
line, forming a final elliptical incision, whose surgical piece will be
removed in monobloc (Figure 3). When
there is no skin leftover for the descent of the superior flap, the
detachment of the mammary gland is preceded by the superior incision of the
ellipse in monobloc;
6. Afterwards, a detachment above the muscular plane is complemented in the
cranial direction. When the breast tissues are released (Figure 4), the transition between the
subcutaneous and glandular cell tissues is superficially incised,
maintaining the final skin thickness around 1.5 to 2.5 cm (Figure 5), depending on the thickness of
the adipose panicle. It is extremely important to preserve the adequate
thickness of the subcutaneous fat during the entire detachment and resection
of the glandular tissue (Figure 6). A
tubular vacuum drain is introduced on each side of the hemithorax;
Figure 3 - Horizontal incisions for monoblock removal.
Figure 3 - Horizontal incisions for monoblock removal.
Figure 4 - Supramuscular detachment of the parenchymal flap.
Figure 4 - Supramuscular detachment of the parenchymal flap.
Figure 5 - Detachment between the mammary gland and the subcutaneous cell
tissue.
Figure 5 - Detachment between the mammary gland and the subcutaneous cell
tissue.
Figure 6 - Pectoralis major muscle exposure for hemostasis.
Figure 6 - Pectoralis major muscle exposure for hemostasis.
7. The superior and inferior flaps are sutured in three planes (Figure 7);
8. The new position of the NAC is preferably marked 1.0 to 2.0 cm lateral to
the intersection of the midclavicular line and the original inframammary
fold. The vertical height is marked approximately 2.5 cm above the
inframammary suture line. Decortication is performed in the graft recipient
area;
9. The NAC is thinned with scissors, and the suture is made with twelve
simple mononylon stitches, like the hours of a clock, being interspersed
with longer threads to fix Brown’s dressing (Figure 8);
10. Medium compression dressing with a cotton swab and microporous tape
covers the entire chest. Compressive mesh or vest is not recommended to
prevent skin flap ischemia.
Figure 7 - Deep plane suture to assess skin tension.
Figure 7 - Deep plane suture to assess skin tension.
Figure 8 - Final result after skin suture by planes and CAP graft completed
+ Brown’s dressing.
Figure 8 - Final result after skin suture by planes and CAP graft completed
+ Brown’s dressing.
Post-operative care
Outpatient return is performed between three and seven days after the
surgical procedure to remove the drains, assess the scar and redress. A
second return visit takes place one week after the first and the third one
around twenty-one days after surgery to remove the graft stitches from the
NAC. At this point, the usual activities such as housework and driving are
released. After three months, intense physical activities are allowed.
RESULTS
The mean age of patients was 27 years and nine months (age range between 18 and
47 years). The weights of the patients were between 48 and 133kg (mean 73kg),
height varied between 1.59m and 1.80m (mean 1.66m), and the mean body mass index
(BMI) was 26.9 (between 17.8 and 39.1). Nineteen patients (73%) had a history of
receiving testosterone hormone therapy before the operation. This hormone was
discontinued three weeks before the surgical intervention and resumed three
weeks later, according to Lo Russo and Innocenti (2017)2. In addition, every patient
underwent a psychological evaluation that allowed the diagnosis of
“female to male” (FTM) transsexualism and was documented through a
psychological report, as well as an evaluation with an endocrinologist and
social worker for a minimum period of 2 years, which was the legal requirement
in effect at the time of this work.
Liposuction was not associated with these surgical procedures. The rate of major
complications was 3.8%, and one patient had small suture dehiscence of
0.5x3.0cm, which healed by the second intention. Minor complications were:
seroma (19.2%) and hematoma (7.7%), punctured and emptied in the office without
needing a new surgical approach. Scarring disorders were found as follows:
keloid in 15.4%, hypertrophic scar in 3.8% and scarring in 3.8%. This patient
with scarring was the only one who underwent a new surgical approach (3.8%),
where fat grafting was performed in the inframammary fold scar.
Other local complications were not found, such as large dehiscence, skin
necrosis, total loss of the NAC graft, infection or evident asymmetries, and
systemic: deep vein thrombosis, pulmonary thromboembolism, fat embolism or
death. Small dyschromia in NACs was seen in some cases, common in this surgical
procedure2, but there
was no desire for a new surgical approach or tattoo for dermal pigmentation for
them.
The total weight of the breasts ranged between 284 and 3,155 grams (average of
1,136), with the weight of the right breasts ranging between 140 and 1,585 grams
(average of 557) and of the left ones between 144 and 1,570 grams (average of
578). All breasts were sent for anatomopathological diagnosis, which showed the
absence of malignancy in all surgical specimens.
The final scar evolved in an inverted “T” in four cases (15.4%) in
breasts of moderate volume and flaccidity. All surgical procedures were
performed separately, without association with other combined surgeries. No
breast had been previously operated on for reduction mammaplasty or mastopexy.
None of the patients in the sample had undergone transgenitalization before MM,
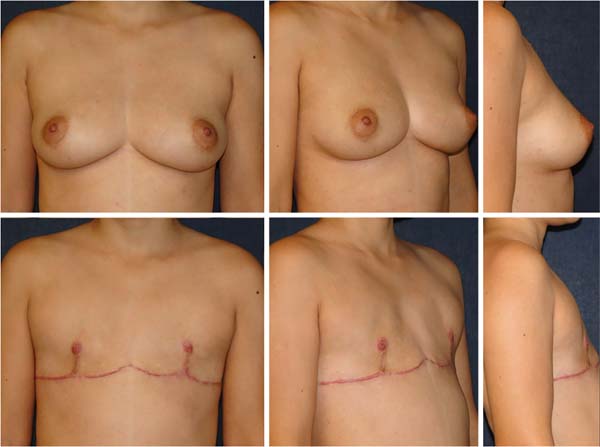
as well as oophoretomy (Figure 9-10).
DISCUSSION
Male transsexualism (or female to male, “female to male” - FTM) is
a gender identity disorder (dysphoria). These individuals believe that they were
raised in the body of the wrong gender, suffer from persistent psychological
discomfort related to their anatomical gender and wish to live and be
permanently accepted in the social role of the male gender1,2.
Figure 9 - Patient 1: 31 years old, body mass index 20, 3 and a half months
after surgery.
Figure 9 - Patient 1: 31 years old, body mass index 20, 3 and a half months
after surgery.
Figure 10 - Patient 2: 19 years old, body mass index 27, 2 months
postoperatively.
Figure 10 - Patient 2: 19 years old, body mass index 27, 2 months
postoperatively.
The treatment of gender dysphoria consists of a combination of different
approaches such as hormonal therapy, surgical therapy and
psychotherapy1,2. Due to the desire to change
their anatomical sexual characteristics to those of the opposite sex, MM is
generally the first, the most important and often the only surgical procedure in
gender readjustment in male transsexuals, especially those with large
breasts2,4 .5.
Regarding the current legal bases for transsexual surgeries, Resolution No. 2265,
of September 20, 2019, of the Federal Council of Medicine, corroborated by
publication in the Federal Official Gazette on 01/09/2020 (edition 6, section 1,
page 96), defines the minimum age of 18 years for sexual reassignment breast
surgeries, such as simple bilateral mastectomy (masculinizing) and 16 years for
hormone therapy, as well as one year of minimum psychiatric follow-up. During
this work, the legal basis was the CFM Resolution 1955/2010, which required 2
years of prior follow-up with an endocrinologist, psychologist and social
worker, in addition to releasing hormone therapy at 18 and surgical procedures
at 21 years of age. The four patients in this study aged 18 and 21 were operated
on with court orders before surgery.
An ultrasound examination of the breasts was performed to assess the presence of
glandular tissue and exclude any pathological tumors in all cases. Patients with
an indication (over 40 years old with no family history and 35 years old with a
positive family history of breast cancer) underwent mammography as a
preoperative diagnostic complement.
Gynecomastia6,7 or mastectomy techniques for breast disease are
commonly used in female patients. Still, subcutaneous mastectomy in FTM
transsexuals is more difficult than the two procedures because these individuals
have considerably larger breast volume, a greater degree of flaccidity and lower
skin elasticity8. Continuous
breast compression with elastic bands makes the quality of the skin and breast
parenchyma worse4,6,8.
The first surgical techniques for MM had unsightly scars along the
chest9,10. Currently, some authors such as Lo Russo and
Innocenti (2017)2, Agarwal et
al. (2017)5 and Knox et al.
(2017)11 indicate to
guide the position of the horizontal scar based on the lower edge of the
pectoralis major muscle, especially on its lateral portion, in an ascending
curve and not exactly on the original inframammary fold, so that it becomes more
imperceptible.
The DIEL-CAP MM is used for most cases, in breasts of moderate to large volume
and moderate to large ptosis, by most authors in the literature2-6,8,12.
Small breasts with little skin flaccidity were not part of this study. The
periareolar technique is indicated, as described by Davidson (1979)7, Colic and Colic
(2000)13, McEvenue et
al. (2017)3 in one surgical
time or Takayagi and Nakagawa (2006)14 in two surgical times, to minimize the resulting scar
in the NAC, or transareolar according to Hage and Bloem (1995)15.
The advantages of the surgical technique described in this author’s work
(DIEL-CAP) are the creation of a good field of view for dissection, exeresis of
the breast parenchyma and hemostasis, allowing an adequate reduction of the NAC
and skin excess, in addition to the absence of possible bulging due to excess
volume with an inferior pedicle areolate. The disadvantages of the technique are
a long inframammary scar and deformities in the projection, and decreased
sensitivity of the breast papillae2.
The upper and lower flaps are adjusted so that the edges are as comfortable as
possible, given that the length of the upper flap tends to be longer than the
lower one. In cases where the breasts have large volumes, the right and left
suture lines can be connected in the median region, forming a
“W”-shaped scar, but this should be avoided when possible due to
the possibility of keloid formation in the presternal region.
Wolter et al. (2015)8 describe
other surgical techniques for treatment, depending on breast volume, summarizing
the previous classification by Monstrey et al. (2008)4:
1) Small breasts, with good elasticity and without ptosis: semicircular
periareolar subcutaneous mastectomy associated with liposuction;
2) Small breasts, moderate elasticity and grade I ptosis: periareolar concentric
mastopexy associated with liposuction;
3) Medium breasts, moderate to poor elasticity and grade II ptosis: mammoplasty
with an inferior pedicle areolate;
4) Large breasts, poor elasticity and grade III ptosis: MM DIEL-CAP.
The technique in group 3 above causes lower patient satisfaction and a higher
rate of irregularities and reoperations8.
Another surgical option for Wolter classification 3 cases is described by Conte
et al. (2019)7, with a NAC
island skin flap, but tends to leave the breast with potential excess
parenchyma.
McEvenue et al. (2017)3
published the study with the largest series of this surgical procedure in the
literature (679 patients over 15 years). They simplified the surgical approach
based on the classification into two single groups:
1) Subcutaneous mastectomy with a semicircular periareolar incision associated
with liposuction in a patient with grade 0 or 1 ptosis with good skin elasticity
(called “keyhole” technique);
2) Double-incision mastectomy associated with NAC-free graft in all other
breasts.
Resende (2007)17 describes a
technique to treat gynecomastia usually applied to male transsexuals. Still, the
scar tends to be noticeable and placed outside the inframammary fold, where the
lower chest contour tends to have less horizontal tension. Monstrey et al.
(2008)4 also use this
technique in some cases.
An important detail refers to the free NAC graft, similar to Thorek’s
technique (1946)18. The graft
donor area can be: 1 - areola margin; 2 - the center of the areola with the
papilla; or 3 - the combination of both, with the central papilla around 0.5 to
1.0 cm in diameter and areolar diameter of 2.5 cm19. The author’s preference is for option
2, with satisfactory results. To improve the contour, tattooing is indicated for
dermal pigmentation after six months. Still, no patient did it, as they were
satisfied with the result, based on the author’s subjective experience,
according to their reports in subsequent visits to the office. However, no
questionnaire on satisfaction has been filled in by the patient, such as those
performed by Wolter et al. (2015)8 or Nelson et al. (2009)12, or evaluation of the quality of the result evaluated
by a surgeon and patient, such as Antoszewski et al. (2012)21.
A crucial point of this surgical procedure is the final horizontal position of
the NAC graft in the chest. Normally, its position tends to be more pleasant
when it is located around one to two centimeters lateral to the intersection
between the original midclavicular line and the final horizontal scar in the
inframammary fold. Thus, the author of this work simplifies other marking
techniques based on the lateral border of the pectoralis major muscle, on the
junction of body lines or a table concerning the chest circumference, which are
more difficult to reproduce2,3,5,9. The author
recommended the vertical distance between the NAC and the final scar of the
inframammary fold to be 2.5 cm, close to what Monstrey et al. (2008)4 orient (half clavicular line and
2-3 cm above the horizontal scar).
When collected in a circular shape, the NAC graft is common to be elliptical with
a longer vertical axis over time due to the tension forces in this direction of
the chest. To avoid this complication, Agarwal et al. (2017)5 advise removing the elliptical
graft measuring 1.5 by 2.5 centimeters and fixing it vertically with the
smallest diameter. Over time it tends to have a rounded shape.
This work was based on the author’s casuistry in that period and presented
to the examining board for Ascension to Full Member of the Brazilian Society of
Plastic Surgery (SBCP - Sociedade Brasileira de Cirurgia
Plástica) at the 55th Brazilian Congress, in Recife, in
2018. After the publication of this work, the author will publish future papers
with the subsequent experience in this technique described, as well as two
others used for smaller breasts: 1) periareolar for patients classified as
grades 1 and 2 by Wolter or grade 1 by McEvenue; 2) double incision with a NAC
mobilization flap for Wolter grade 3 and McEvenue grade 2 without great
flaccidity and ptosis.
CONCLUSION
Mastectomy is a safe procedure with good reproducibility, and that brings
satisfactory aesthetic results.
REFERENCES
1. Hage JJ, Karim RB. Ought GIDNOS get nought? Treatment options for
nontranssexual gender dysphoria. Plast Reconstr Sur. 2000
Mar;105(3):1222-7.
2. Lo Russo G, Innocenti M. Masculine chest-wall contouring in FtM
transgender: a personal approach. Aesthetic Plast Surg. 2017
Abr;41(2):369-74.
3. McEvenue G, Xu FZ, Cai R, McLean H. Female-to-male gender affirming
top surgery: a single surgeon’s 15-year retrospective review and
treatment algorithm. Aesthet Surg J. 2017 Dez;38(1):49-57.
4. Monstrey S, Selvaggi G, Ceulemans P, Van Landuyt K, Bowman C,
Blondeel P, et al. Chest-wall contouring surgery in female-to-male transsexuals:
a new algorithm. Plast Reconstr Surg. 2008 Mar;121(3):849-59.
5. Agarwal CA, Wall VT, Mehta ST, Donato DP, Walzer NK. Creation of an
aesthetic male nipple areolar complex in female-to-male transgender chest
reconstruction. Aesth Plast Surg. 2017 Dez;41(6):1305-10.
6. Top H, Balta S. Transsexual mastectomy: selection of appropriate
technique according to breast characteristics. Balkan Med J. 2017
Mar;34(2):147-55.
7. Davidson BA. Concentric circle operation for massive gynecomastia to
excise the redundant skin. Plast Reconstr Surg. 1979
Mar;63(3):350-4.
8. Wolter A, Diedrichson J, Scholz T, Arens-Landwehr A, Liebau J.
Sexual reassignment surgery in female-to-male transsexuals: an algorithm for
subcutaneous mastectomy. J Plast Reconstr Aesthet Surg. 2015
Fev;68(2):184-91.
9. Hage JJ, Van Kesteren PJ. Chest-wall contouring in female-to-male
transsexuals: basic considerations and review of the literature. Plast Reconstr
Surg. 1995 Ago;96(2):386-91.
10. Lindsay WR. Creation of a male chest in female transsexuals. Ann
Plast Surg. 1979;3(1):39-46.
11. Knox ADC, Ho AL, Leung L, Hynes S, Tashakkor AY, Park YS, et al. A
review of 101 consecutive subcutaneous mastectomies and male chest contouring
using the concentric circular and free nipple graft techniques in female-to-male
transgender patients. Plast Reconstr Surg. 2017
Jun;139(6):1260e-72e.
12. Nelson L, Whallett EJ, McGregor JC. Transgender patient satisfaction
following reduction mammaplasty. J Plast Reconstr Aesthet Surg. 2009
Mar;62(3):331-4.
13. Colic MM, Colic MM. Circumareolar mastectomy in female-to-male
transexuals and large gynecomastias: a personal approach. Aesthetic Plast Surg.
2000 Nov/Dez;24(6):450-4.
14. Takayagi S, Nakagawa C. Chest wall contouring for female-to-male
transexuals. Aesthetic Plast Surg. 2006 Mar/Abr;30(2):206-213.
15. Hage JJ, Bloem JJ. Chest wall contouring for female-to-male
transsexuals: Amsterdam experience. Ann Plast Surg. 1995
Jan;34(1):59-66.
16. Conte CHR, Correa JPT, Pinto EBS, Rocha PAC, Puhl RC, Daher JAC.
Técnica de mastectomia masculinizadora (FTM) -
interpretação pessoal. Rev Bras Cir Plást.
2019;34:45-7.
17. Resende JHC. Técnica para correção de ptose
mamária masculina pós-grandes emagrecimentos. Rev Bras Cir
Plást. 2007;22(1):1-9.
18. Thorek M. Plastic reconstruction of the breast and free
transplantation of the nipple. J Int Coll Surg. 1946
Mar/Abr;9:194-224.
19. Tanini S, Lo Russo G. Shape, position and dimension of the nipple
areola complex in the ideal male chest: a quick and simple operating room
technique. Aesth Plast Surg. 2018 Ago;42(4):951-7.
20. Antoszewski B, Bratos R, Sitek A, Fijalkowska M. Long-term results
of breast reduction in female-to-male transsexuals. Pol Przegl Chir. 2012
Mar;84(3):144-51.
1. Hospital Santa Lucinda, Sorocaba, SP,
Brazil.
2. Private Clinic of Plastic Surgery, Dr. Bruno
Marques, Sorocaba, SP, Brazil.
Corresponding author: Bruno Pires do Amaral
Marques, Rua Av Antônio Carlos Comitre, nº 1296 Parque
Campolim, Sorocaba, SP, Brazil, Zip code: 18047-620, E-mail:
brunopamarques@gmail.com
Article received: February 17, 2019.
Article accepted: July 12, 2021.
Conflicts of interest: none.
Institution: Private Clinic of Plastic Surgery, Dr. Bruno Marques, Sorocaba,
SP, Brazil.