INTRODUCTION:
Aesthetic procedures in the gluteal region are increasingly in evidence in recent
decades. In the United States of America, there was an increase of 86% from 2013 to
2014, reaching in 2014 the number of 21.446 gluteoplasty procedures1. According to data from the Sociedade Brasileira de Cirurgia Plástica, in Brazil from 2008 to 2011, there was a 20% increase in procedures number 2.
This increased demand for the procedure added to the development of new techniques
and the greater ease of access to imaging methods, make imaging exams in patients
undergoing gluteoplasty increasingly frequent, currently highlighting magnetic resonance
imaging evaluation of this region. Thus, the image enters more and more into the plastic
surgeon’s daily clinical practice, requiring knowledge about basic concepts regarding
the exams’ request and interpretation.
This article reviews magnetic resonance imaging aspects of aesthetic procedures of
the gluteal region and its complications.
OBJECTIVE
Illustrate through magnetic resonance studies the usual findings in gluteoplasty procedures
and some of its complications. Also, propose a protocol of magnetic resonance sequences
to be performed to evaluate the region better, considering the particularities of
each suspect of the requesting physician and each procedure performed.
METHODS
Illustrative cases of patients who underwent gluteoplasty procedures were selected,
whether approved, off-label, or even illicit3, in which we conducted magnetic resonance imaging in the laboratories of the Fleury
group (Fleury brand, Amais and in the imaging service of the Hospital Alemão Oswaldo
Cruz, located in the city of São Paulo) in the period between 2016 and 2019, not being
the totality of the cases observed, but the most representative cases in relation
to the imaging findings.
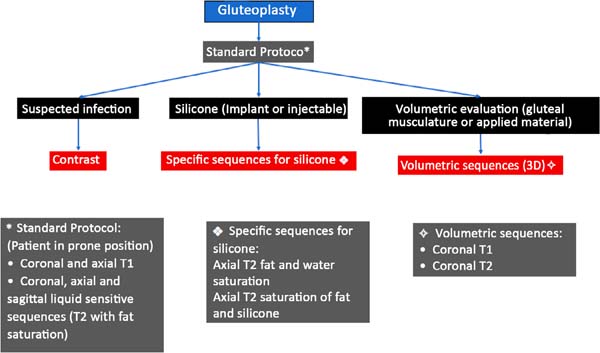
The patients underwent MRI scans on equipment from different manufacturers, all of
which were 1.5 Tesla. The protocol for image acquisition was the one we proposed (Figure 1), comprising for each suspicion and type of implant, additions of sequences to the
standard protocol usually performed for the cases. The type of procedure to which
the patient was submitted was decided by completing a questionnaire directed before
the examination and the medical request’s information. When it was necessary, contact
was made with the requesting physician to complement the information.
Figure 1 - Proposed protocol for conducting the MRI study with the sequences to be added to the
standard protocol for the requesting physician’s clinical suspicion and the procedure
performed.
Figure 1 - Proposed protocol for conducting the MRI study with the sequences to be added to the
standard protocol for the requesting physician’s clinical suspicion and the procedure
performed.
The patients’ examinations were evaluated by at least two radiologists with a subspecialty
in musculoskeletal radiology, with experience of 5 and 15 years and graduated from
the Brazilian College of Radiology.
DISCUSSION
Silicone implant, lipografting and so-called local flaps are surgical methods recognized
in the literature to increase the gluteal region’s projection. Minimally invasive
methods with the use of filling materials, in turn, have been gaining space in recent
years, being part of the clinical practice of many professionals. Unfortunately, the
use of liquid silicone injectables applied by non-medical individuals, or even the
application of filling materials by professionals without adequate specialization,
is still a Brazilian reality, resulting in often serious complications4.
Regardless of the type of procedure performed, all are subject to complications, the
most common being: seroma or hematoma formation, infection, material migration, inflammatory
reaction/foreign body, compression of the vasculonervous bundle, among others. In
the specific case of silicone implants, we may still have rupture, displacement and
capsular contracture5.
For analysis by magnetic resonance (MRI) method, we basically have the sequences in
the T1 weighting, in which the fat appears with a high sign (“white”) and demonstrates
more conspicuously the anatomy, and the T2-weighted sequences with fat suppression,
in which the fat appears with low signal (“dark”), and the areas containing liquid
or edema shine (liquid-sensitive sequences). Other additional sequences are employed
depending on each particular case: the specific sequences for silicone, post-contrast
sequences, and volumetric sequences; for this more specific type of evaluation, we
suggest following the protocol in Figure 1.
It is worth mentioning that this protocol consists only of a suggestion based on the
practice of imaging diagnoses performed in our service, and no validation of said
protocol was performed, which is a relevant limitation of the study.
Silicone implant:
Structurally, silicone implants are composed of a solid silicone elastomer enclosure
containing a silicone gel inside6. In the United States, unlike Brazil and other countries, only solid silicone elastomer
implantation is approved for gluteoplasties7, to the detriment of silicone gel and saline implant.
On computed tomography (CT) images, the implants are slightly hyperdense compared
to muscle6,8, demonstrating intermediate signal intensity on T1 and T2 weighted MRI images9.
Magnetic resonance imaging is the most accurate imaging modality for noninvasive evaluation
of implant integrity9.
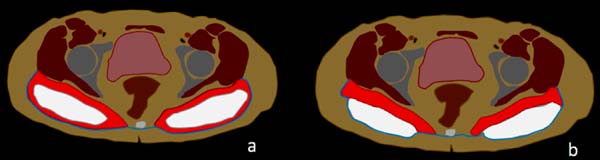
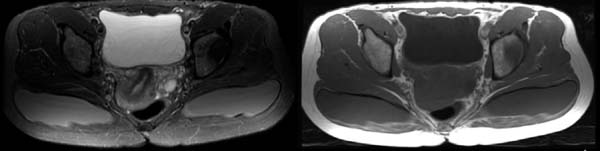
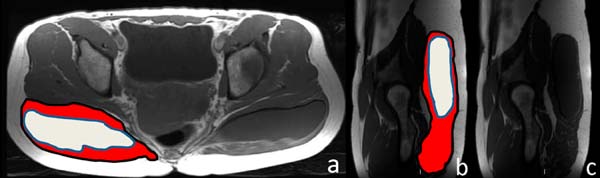
Figure 2 shows a scheme of the usual positioning seen in the axial magnetic resonance sections
for the two most common types of the gluteal implants’ location, the intramuscular
or subfascial spaces. In Figure 3, we have the usual presentation in the axial section of a patient with an intramuscular
implant in T1-weighted and T2-weighted sequences.
Figure 2 - Illustrative scheme of axial sections with intramuscular (a) and subfascial (b) gluteal
implants. Maximum gluteus in red, muscle fascia in blue and silicone implants in white.
Figure 2 - Illustrative scheme of axial sections with intramuscular (a) and subfascial (b) gluteal
implants. Maximum gluteus in red, muscle fascia in blue and silicone implants in white.
Figure 3 - Normal appearance of magnetic resonance imaging of intramuscular implants. (a) Axial
T2 with fat saturation; (b) Axial T1. Intermediate silicon signal in both sequences.
Figure 3 - Normal appearance of magnetic resonance imaging of intramuscular implants. (a) Axial
T2 with fat saturation; (b) Axial T1. Intermediate silicon signal in both sequences.
Figure 4 shows how intramuscular implants are seen in T1-weighted sequences, axial plane and
also sagittal plane.
Figure 4 - Illustrative scheme and normal appearance of intramuscular implants in axial (a) and
sagittal (b) T1-weighted sections. Maximum gluteus in Red and silicone implants in
white.
Figure 4 - Illustrative scheme and normal appearance of intramuscular implants in axial (a) and
sagittal (b) T1-weighted sections. Maximum gluteus in Red and silicone implants in
white.
Magnetic resonance protocols for evaluating the gluteus implant include sequences
similar to those used for breast implant evaluation, with sequences for both silicone
signal suppression and accentuation of its signal6,9.
Selective silicone sequences include the suppression of the water and fat signal,
which increases the contrast between silicone and surrounding tissues. Similarly,
a sequence that suppresses the silicone signal provides a useful additional means
to confirm, for example, whether extracapsular silicone is present9.
The depth of positioning of silicone implants varies by anatomical location and has
implications concerning the types of complications observed after surgery. They can
be inserted more commonly in intramuscular or subfascial spaces10,11 (figure 2).
In a plane created within the gluteus muscle fibers, the implant’s intramuscular placement
is the most popular because it provides satisfactory aesthetic results and a lower
prevalence of complications10,11.
A systematic review of the literature reported complication rates for different sites
of prostheses placement: 55% for subfascial, 18% for intramuscular, 18% for submuscular
methods and 13% for methods with intramuscular technique XYZ11.
Oranges et al.10, in turn, reviewed the literature that showed an overall complication
rate of 30.5% for cosmetic surgeries of gluteus implant, the most prevalent being:
surgical wound dehiscence (8.1%), seroma (4.4%), infection (3.2%) (figure 5) and implant revision (3.1%). Other complications reported, however, less frequent,
are rupture of the prosthesis (figure 6), displacement (figure 7) and contracture (figure 8).
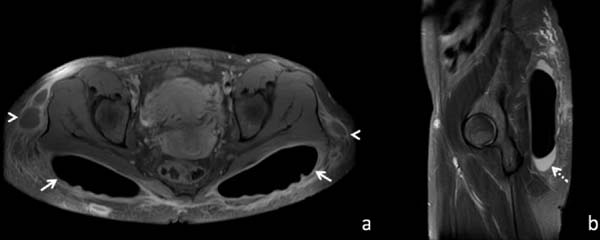
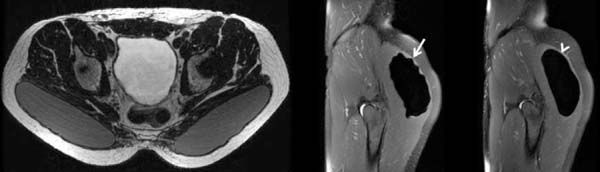
Figure 5 - (a) Axial T1 with saturation of fat and silicone, post-contrast; (b) Sagittal T2 with
suppressing fat and silicone. A 32-year-old patient with previous local subcutaneous
filling with polyacrylamide gel, who underwent gluteoplasty with silicone implants,
developing a postoperative infection. Images show bilateral silicone implants with
peripheral enhancement (arrows) and peri-implant effusion (dotted arrow). Also, note
the collections in the hips’ subcutaneous area (arrowheads), representing the infected
polyacrylamide gel.
Figure 5 - (a) Axial T1 with saturation of fat and silicone, post-contrast; (b) Sagittal T2 with
suppressing fat and silicone. A 32-year-old patient with previous local subcutaneous
filling with polyacrylamide gel, who underwent gluteoplasty with silicone implants,
developing a postoperative infection. Images show bilateral silicone implants with
peripheral enhancement (arrows) and peri-implant effusion (dotted arrow). Also, note
the collections in the hips’ subcutaneous area (arrowheads), representing the infected
polyacrylamide gel.
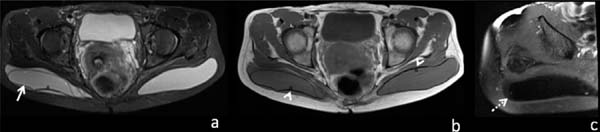
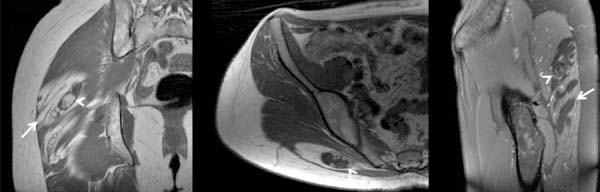
Figure 6 - (a) Axial T2 with fat saturation; (b) Axial T1; (c) Axial T2 with suppression of fat
and silicone from the right hip. A 42-year-old patient with a bilateral intramuscular
silicone implant. Lobulated and redundant appearance of the right implant casing (arrow).
Rotation of the right implant; note that the marker is positioned later, unlike the
contralateral side (arrowheads). Complete suppression of the intra and peri-envelope
contents in the silicone suppression sequence confirms the intracapsular rupture (dotted
arrow).
Figure 6 - (a) Axial T2 with fat saturation; (b) Axial T1; (c) Axial T2 with suppression of fat
and silicone from the right hip. A 42-year-old patient with a bilateral intramuscular
silicone implant. Lobulated and redundant appearance of the right implant casing (arrow).
Rotation of the right implant; note that the marker is positioned later, unlike the
contralateral side (arrowheads). Complete suppression of the intra and peri-envelope
contents in the silicone suppression sequence confirms the intracapsular rupture (dotted
arrow).
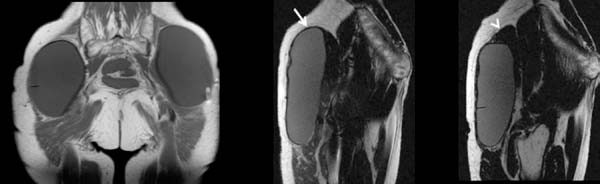
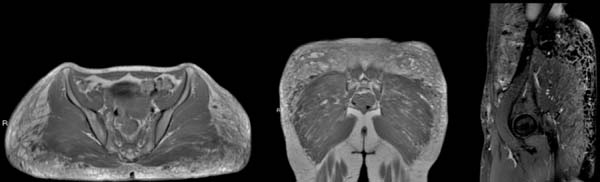
Figure 7 - (a) Coronal T1; (b) and (c) Sagittal T1. 59-year-old patient. Five years post-surgical
bilateral silicone implant. Recent pain and bulging in the left gluteal region. Images
show the upper displacement of the left implant. Note that the upper region of the
left implant is covered by a thin muscle layer (arrow in B). Compare to the thickest
layer on the contralateral side (arrowhead in C).
Figure 7 - (a) Coronal T1; (b) and (c) Sagittal T1. 59-year-old patient. Five years post-surgical
bilateral silicone implant. Recent pain and bulging in the left gluteal region. Images
show the upper displacement of the left implant. Note that the upper region of the
left implant is covered by a thin muscle layer (arrow in B). Compare to the thickest
layer on the contralateral side (arrowhead in C).
Figure 8 - (a) Axial T2 without suppression of fat; (b) and (c) Sagital T2 with suppression of
fat and silicone. Bilateral intramuscular silicone implant. Clinical suspicion of
implant contracture. No local pain. Observe the irregular / lobulated contours of
the right implant (arrow), representing the capsular contracture. Compare to regular
contours on the contralateral side (arrowhead).
Figure 8 - (a) Axial T2 without suppression of fat; (b) and (c) Sagital T2 with suppression of
fat and silicone. Bilateral intramuscular silicone implant. Clinical suspicion of
implant contracture. No local pain. Observe the irregular / lobulated contours of
the right implant (arrow), representing the capsular contracture. Compare to regular
contours on the contralateral side (arrowhead).
The number of procedures has been falling in the last two years in the United States,
possibly because it presents a percentage of complications still considered high,
a more limiting postoperative period with absence from usual activities for longer
than other techniques, in addition to large scars. This number decreased by 56% from
2016 to 2017 and by 28% from 2017 to 2018, with less than 1,000 procedures being performed
this past year12.
Autologous lipografting:
Autologous lipografting is characterized by a procedure for collecting fat from the
site where removal is aesthetically desired, such as the abdomen or thighs, and transfer
to increase other areas in the same patient, commonly in the buttocks. In the American
market, the method is known as”Brazilian buttock lift”13.
According to the American Society of Plastic Surgeons, procedures in the United States
increased 10% from 2016 to 2017 and 19% from 2017 to 2018, with more than 24,000 being
performed this past year.12.
Better aesthetic results are obtained by combining subcutaneous, subdermal and intramuscular
injections for augmentation gluteoplasty14,15.
On CT or MRI images (figure 9), fat grafting on the subcutaneous is difficult to characterize due to similar characteristics
with subcutaneous cellular tissue. On the contrary, the fat injected in the intramuscular
region is easily identified by both methods, such as lobular foci of macroscopic fat,
with low characteristic density on tomography (values of - 150 to -50 Hounsfield units),
of permeate to muscle fibers, and with high signal in conventional sequences weighted
in T1, on magnetic resonance imaging. The adipose nature is confirmed with the fat
suppression sequences on MRI, presenting low signal, both in T1 and T2( weighting6.
Figure 9 - (a) Axial T1 (b) Coronal T1. Normal aspect of gluteal fat grafting on magnetic resonance
imaging, with bands of fat permeating the most superficial fibers of the bilateral
maximum glutes, makes it impossible to differentiate in the grafted material’s subcutaneous
tissue and the natural fat.
Figure 9 - (a) Axial T1 (b) Coronal T1. Normal aspect of gluteal fat grafting on magnetic resonance
imaging, with bands of fat permeating the most superficial fibers of the bilateral
maximum glutes, makes it impossible to differentiate in the grafted material’s subcutaneous
tissue and the natural fat.
Magnetic resonance imaging (MRI) can be used to document the integration of the fat
graft and volumetric variations produced in the buttocks after lipografting10.
In the literature10, there is a global rate of complications in patients with autologous lipografting
of 10.5%, and donor site seroma is the most common complication (3.1%). Other complications
reported were: liponecrosis (0.7%) (figure 10), cellulitis (0.5%), asymmetry (0.4%), infection (0.3 %) and fatty embolism (0.2%).
Compared to silicone implants, lipografting has the advantages of being more targeted
and allowing the concomitant conformation of the hip and waist regions, which affects
the overall aesthetic appearance of the gluteus17 a more natural result. It also allows a higher degree of increase and less evident
scars7. Moreover, the rate of complications is lower than for implants6.
Figure 10 - (a) Coronal T1; (b) Axial T1; (c) Sagital T2 with fat saturation. 30-year-old patient.
Previous liposculpture procedure. Patient with a palpable nodule on physical examination.
Observe the usual aspect of liposculpture represented by elongated bands with a sign
similar to that of fat within the gluteus maximus muscle (arrows). Nodular images
within these fat areas show a slightly high T1-weighted signal, with a low-signal
halo of peripheral fibrotic tissue, without local edema, representing chronic steatonecrosis
(arrowheads).
Figure 10 - (a) Coronal T1; (b) Axial T1; (c) Sagital T2 with fat saturation. 30-year-old patient.
Previous liposculpture procedure. Patient with a palpable nodule on physical examination.
Observe the usual aspect of liposculpture represented by elongated bands with a sign
similar to that of fat within the gluteus maximus muscle (arrows). Nodular images
within these fat areas show a slightly high T1-weighted signal, with a low-signal
halo of peripheral fibrotic tissue, without local edema, representing chronic steatonecrosis
(arrowheads).
Filling Materials:
The use of dermal filling materials has grown sharply in recent years, totaling more
than 2.6 million procedures in 2018 in the United States, more than three times the
number of procedures performed in 200012.
As the indications and the number of procedures performed increase, the number of
complications is likely to increase18.
Concerning classification can be divided into absorbable/temporary (hyaluronic acid,
collagen, polyacrylamide gel, poly-L-lactic acid, calcium hydroxyapatite) and non-absorbable/permanent
acid (polymethylmethacrylate).
Although some studies report these materials’ imaging characteristics in magnetic
resonance imaging6, the literature’s data are still scarce, so the signal pattern is still considered
in general nonspecific. Thus, magnetic resonance imaging is more used to evaluate
possible complications, besides determining the location, quantity and extent of the
applied material.
Magnetic resonance imaging can detect amounts as small as 2 mm in diameter of filling
materials, in addition to complications such as abscesses and granulomas that have
not been clinically detected19.
The use in small amounts and specific regions, such as the face and back of the hands,
is well established in plastic surgery. However, the use of larger volumes and other
body sites, such as the gluteal region, is still a controversial issue.
Some European authors have published studies using hyaluronic acid applied to the
subcutaneous region of the gluteal region20,21, with volumes of up to 400 ml per patient, with satisfactory results. They emphasize
in their studies that traditional methods of gluteoplasty are all surgical procedures
that usually require general anesthesia and/or produce scarring. Consequently, many
people are looking for minimally invasive procedures. Hyaluronic acid is chosen because
it is easy to use, biocompatible, non-toxic and easily removable, if necessary 20. Material degradation results in volume reduction over time, which can be evaluated
by magnetic resonance imaging20. The overall rate of complications with the use of hyaluronic acid in these two studies
was equal to 39.1%, and none of the complications evaluated was severe. Among the
most frequent complications reported are swelling (7.2 %), pruritus (7.2 %), pain
at the injection site (5.8 %), hematoma (5.8 %), displacement of the material (4.3
%)10.
Other authors 22,23 reported in their articles the use of poly-L-lactic acid (PLLA) for filling in the
gluteal region, with the application of the material in the subcutaneous, using volumes
of up to 48 ml per buttock per session. They did not report serious complications.
Unlike other temporary filling materials that basically act occupying space, such
as collagen and hyaluronic acid-based products, poly-L-lactic acid (PLLA) aims to
gradually promote collagen deposition through a biostimulator response, with therapeutic
effects that last approximately two years24.
A recent publication25 brings a consensus on recommendations regarding (PMMA) in Brazil for facial and body
aesthetic procedures. According to the publication, deeper plans should be chosen
whenever possible for body treatment with PMMA. Subcutaneous, intramuscular and submuscular
planes can be used based on the needs of each patient. According to the experts’ recommendations,
the volume applied in the gluteal region can reach 150 ml in a single application.
Figure 11 illustrates a case of polymethylmethacrylate gluteoplasty on magnetic resonance imaging
in an asymptomatic patient, and Figure 12 illustrates a case of late complication with a local inflammatory process, but in
this case, liquid silicone was associated.
Figure 11 - (a) Axial and (b) Coronal T2 with fat saturation (c) Axial T1. 31-year-old patient,
asymptomatic. Bilateral procedure of gluteal filling with polymethylmethacrylate (PMMA)
for three years. Amorphous material with a high signal in T2 permeating the fibers
of the maximum glutes and in the adjacent subcutaneous mesh (arrows). The material
has a muscle-like signal in T1-weighted images (dotted arrow).
Figure 11 - (a) Axial and (b) Coronal T2 with fat saturation (c) Axial T1. 31-year-old patient,
asymptomatic. Bilateral procedure of gluteal filling with polymethylmethacrylate (PMMA)
for three years. Amorphous material with a high signal in T2 permeating the fibers
of the maximum glutes and in the adjacent subcutaneous mesh (arrows). The material
has a muscle-like signal in T1-weighted images (dotted arrow).
Figure 12 - (a) Axial and (b) coronal T1; (c) Sagital T2 with saturation of fat and silicone.
A 34-year-old patient presenting pain, heat, swelling and nodules in the lateral region
of the hips, six months after the application of methacrylate and liquid silicone
in the gluteal region. Diffuse heterogeneity of the subcutaneous mesh signal, related
to diffuse infiltration of lobulated and amorphous material.
Figure 12 - (a) Axial and (b) coronal T1; (c) Sagital T2 with saturation of fat and silicone.
A 34-year-old patient presenting pain, heat, swelling and nodules in the lateral region
of the hips, six months after the application of methacrylate and liquid silicone
in the gluteal region. Diffuse heterogeneity of the subcutaneous mesh signal, related
to diffuse infiltration of lobulated and amorphous material.
We have not found in the literature reports of polyacrylamide gel (PAAG) in the gluteal
region. We have one case using this material in an asymptomatic patient (figure 13) and another with material migration (figure 14).
Figure 13 - (a) Axial and (b) Coronal T2 with fat saturation; (c) Axial T1. 29-yearold patient.
Local filling procedure with PAAG 2 months ago. Conglomerates of rounded images with
a high signal at T2 weighting in the gluteal regions’ subcutaneous region (arrows).
Similar diffuse alteration of signal in the gluteus maximus is observed (arrowheads).
The material has a muscle-like signal in T1-weighted images (dotted arrow).
Figure 13 - (a) Axial and (b) Coronal T2 with fat saturation; (c) Axial T1. 29-yearold patient.
Local filling procedure with PAAG 2 months ago. Conglomerates of rounded images with
a high signal at T2 weighting in the gluteal regions’ subcutaneous region (arrows).
Similar diffuse alteration of signal in the gluteus maximus is observed (arrowheads).
The material has a muscle-like signal in T1-weighted images (dotted arrow).
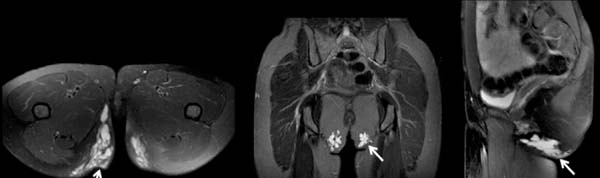
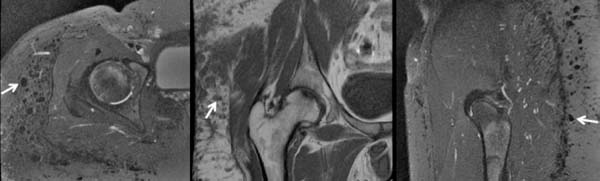
Figure 14 - (a) Axial (b) Coronal and (c) Sagittal T2 with fat saturation. A 34-year-old patient
presenting discomfort when sitting for a week. Application of polyacrylamide gel (PAAG)
on the buttocks for five years. The images show confluent material, with a high signal
at T2, located in the subcutaneous fat of the infragluteal fold regions and partially
insinuating itself into the bilateral ischioanal fat representing the filling material
(arrows). Observe the lower position of the material concerning the expected region,
probably due to the gravity effect.
Figure 14 - (a) Axial (b) Coronal and (c) Sagittal T2 with fat saturation. A 34-year-old patient
presenting discomfort when sitting for a week. Application of polyacrylamide gel (PAAG)
on the buttocks for five years. The images show confluent material, with a high signal
at T2, located in the subcutaneous fat of the infragluteal fold regions and partially
insinuating itself into the bilateral ischioanal fat representing the filling material
(arrows). Observe the lower position of the material concerning the expected region,
probably due to the gravity effect.
It is important to maintain a high rate of clinical suspicion of infection when filling
agents are identified in imaging tests because abscesses can be difficult to differentiate
from certain materials that have CT and MRI imaging characteristics close to those
of water, such as hyaluronic acid5. However, abscesses tend to exhibit a higher degree of enhancement around by intravenous
contrast26.
Silicone:
The Agência Nacional de Vigilância Sanitária (National Health Surveillance Agency)
(Anvisa) prohibits industrial silicone for aesthetic procedures. The illegal application
of industrial silicone in the human body is considered a crime against public health
provided for in the Penal Code. Of course, cosmetic augmentation silicone injection
is also not approved by the U.S. Food and Drug Administration (FDA).
Nevertheless, this practice is still present, possibly due to low costs compared to
approved surgical procedures and the lack of information on the associated risks.
The gluteal region is one of the most common sites of application of the material5.
Liquid silicone is as dense or slightly denser than soft parts on tomography. In MRI,
it tends to demonstrate intermediate signal intensity or slightly higher than the
water signal in T1-weighted images and variable intensity in T2-weighted images, possibly
due to different viscosities, with high viscosity silicone generally more hypointense
at T2 6,7,8,16,27,28.
In the specific sequence for silicone, with suppression of the water and fat signal,
it has a high signal19.
Because silicone permanently resides in tissues, surgical removal may be the only
way to treat chronic problems. However, surgical removal of silicone can be very difficult
for the surgeon and disfiguring for the patient. Preoperative MRI with specific silicone
sequences can help define and locate the material before any surgical attempt to locate
the silicone and facilitate identification and removal by the surgeon8.
The host’s tissue response after silicone injection results in the formation of granulomas6 (figure 15). Granulomatous reactions can occur weeks to decades after injection7.
Figure 15 - (a) T2 axial with saturation of fat and silicone (b) T1 coronal and (c) Sagital T2
with saturation of fat and silicone. History of liquid silicone injection in the gluteal
region. Multiple nodules of low signal intensity in the subcutaneous tissue of the
right buttock and hips (arrows), representing a typical aspect of the subcutaneous
silicone.
Figure 15 - (a) T2 axial with saturation of fat and silicone (b) T1 coronal and (c) Sagital T2
with saturation of fat and silicone. History of liquid silicone injection in the gluteal
region. Multiple nodules of low signal intensity in the subcutaneous tissue of the
right buttock and hips (arrows), representing a typical aspect of the subcutaneous
silicone.
Minor complications include injection site reaction, erythema, edema, and scars12. Due to silicone impurities and the non-sterile conditions under which injections
often occur, these procedures can be complicated by chronic cellulitis, abscesses,
and myositis. Other local silicone injection complications include migration, hyperpigmentation
and fibrosis of the skin, necrosis, ulceration, fistula, disfigurement6.
CONCLUSION
We present the common findings on magnetic resonance imaging of gluteoplasty procedures,
together with the spectrum of images of some of its possible complications, in addition
to an organization chart with suggested magnetic resonance protocol.
REFERENCES
1. https://doi.org/10.1093/asj/35.Supplement_2.1
2. Lima DA, Minakami DA, Pereira LC, Grando MC, Cruz RS, Braga AR, et al. Gluteoplasty
augmentation: the importance of teaching of training residents to meet increasing
demand. Rev Bras Cir Plást. 2011;26(1):127-33.
3. Nakamoto HA, Goldenberg D. We need to discuss gluteal fat grafting. Rev Bras Cir Plást.
2018;33(3):270-1.
4. Chasan PE. The history of injectable silicone fluids for soft-tissue augmentation.
Plast Reconstr Surg. 2007 Dez;120(7):2034-40;discussion:2041-3.
5. http://dx.doi.org/10.1097/sap.0000000000001765
6. Lin DJ, Wong TT, Ciavarra GA, Kazam JK. Adventures and misadventures in plastic surgery
and soft-tissue implants. Radiographics. 2017 Nov/Dez;37(7):2145-63.
7. Yahyavi-Firouz-Abadi N, Menias CO, Bhalla S, Siegel C, Gayer G, Katz DS. Imaging of
cosmetic plastic procedures and implants in the body and their potential complications.
AJR Am J Roentgenol. 2015 Abr;204(4):707-15.
8. Frank SJ, Flusberg M, Friedman S, Sternschein M, Wolf EL, Stein MW. Aesthetic surgery
of the buttocks: imaging appearance. Skeletal Radiol. 2014 Fev;43(2):133-9.
9. Seiler SJ, Sharma PB, Hayes JC, Ganti R, Mootz AR, Eads ED, et al. Multimodality imaging-based
evaluation of single-lumen silicone breast implants for rupture. Radiographics. 2017
Mar/Abr;37(2):366-82.
10. Oranges CM, Tremp M, Di Summa PG, Haug M, Kalbermatten DF, Harder Y, et al. Gluteal
augmentation techniques: a comprehensive literature review. Aesthet Surg J. 2017 Mai;37(5):560-9.
11. Flores-Lima G, Eppley BL, Dimas JR, Navarro DE. Surgical pocket location for gluteal
implants: a systematic review. Aesthetic Plast Surg. 2013 Jan;37(2):240-5.
12. American Society of Plastic Surgeons (ASPS). 2018 National Plastic Surgery Statistics:
cosmetic and reconstructive procedure trends [Internet]. Arlington Heights: ASPS;
2018; [access in 2019 May 15]. Available from:
13. https://doi.org/10.1093/asj/sjx004
14. Toledo LS. Gluteal augmentation with fat grafting: the Brazilian buttock technique:
30 years' experience. Clin Plast Surg. 2015 Abr;42(2):253-61.
15. Condé-Green A, Kotamarti V, Nini KT, Wey PD, Ahuja NK, Granick MS, et al. Fat grafting
for gluteal augmentation: a systematic review of the literature and meta-analysis.
Plast Reconstr Surg. 2016 Set;138(3):437e-46e.
16. Wolf GA, Gallego S, Patrón AS, Ramírez F, Delgado JA, Echeverri A, et al. Magnetic
resonance imaging assessment of gluteal fat grafts. Aesthetic Plast Surg. 2006 Jul/Ago;30(4):460-8.
17. Sinno S, Chang JB, Brownstone ND, Saadeh PB, Wall Junior S. Determining the safety
and efficacy of gluteal augmentation: a systematic review of outcomes and complications.
Plast Reconstr Surg. 2016 Abr;137(4):1151-6.
18. Funt D, Pavicic T. Dermal fillers in aesthetics: an overview of adverse events and
treatment approaches. Clin Cosmet Investig Dermatol. 2013 Dez;6:295-316.
19. Mundada P, Kohler R, Boudabbous S, Trellu LT, Platon A, Becker M. Injectable facial
fillers: imaging features, complications, and diagnostic pitfalls at MRI and PET CT.
Insights Imaging. 2017 Dez;8(6):557-72.
20. Camenisch CC, Tengvar M, Hedén P. Macrolane for volume restoration and contouring
of the buttocks: magnetic resonance imaging study on localization and degradation.
Plast Reconstr Surg. 2013 Out;132(4):522e-9e.
21. De Meyere B, Mir-Mir S, Peñas J, Camenisch CC, Hedén P. Stabilized hyaluronic acid
gel for volume restoration and contouring of the buttocks: 24-month efficacy and safety.
Aesthetic Plast Surg. 2014 Abr;38(2):404-12.
22. Lorenc ZP. Techniques for the optimization of facial and nonfacial volumization with
injectable poly-L-lactic acid. Aesthetic Plast Surg. 2012 Out;36(5):1222-9.
23. Mazzuco R, Sadick NS. The use of poly-L-lactic acid in the gluteal area. Dermatol
Surg. 2016 Mar;42(3):441-3.
24. Jabbar A, Arruda S, Sadick N. Off face usage of poly-L-lactic acid for body rejuvenation.
J Drugs Dermatol. 2017 Mai;16(5):489-94.
25. Souza TAB, Colomé LM, Bender EA, Lemperle G. Brazilian consensus recommendation on
the use of polymethylmethacrylate filler in facial and corporal aesthetics. Aesthetic
Plast Surg. 2018 Out;42(5):1244-51.
26. Ginat DT, Schatz CJ. Imaging features of midface injectable fillers and associated
complications. AJNR Am J Neuroradiol. 2013 Ago;34(8):1488-95.
27. Cheung YC, Su MY, Ng SH, Lee KF, Chen SC, Lo YF. Lumpy silicone-injected breasts:
enhanced MRI and microscopic correlation. Clin Imaging. 2002 Nov/Dez;26(6):397-404.
28. Mathews VP, Elster AD, Barker PB, Buff BL, Haller JA, Greven CM. Intraocular silicone
oil: in vitro and in vivo MR and CT characteristics. AJNR Am J Neuroradiol. 1994 Fev;15(2):343-7.
1. Fleury, Radiologia, São Paulo, SP, Brazil.
Corresponding author:
Flavio Donaire Cônsolo Rua Pernambuco, Higienópolis, 210, Apart. 61B, São Paulo, SP, Brazil. Zip Code: 01240-020
E-mail: fconsolo@me.com
Article received: February 06, 2020.
Article accepted: January 10, 2021.
Conflicts of interest: none.