INTRODUCTION
Abdominoplasty is a popular surgical procedure, as the abdominal region is an important
functional esthetic unit defining the body contour. We observed some patients with
a prominent abdominal bulge, which was difficult to treat based on unsatisfactory
results or recurrence with conventional treatments1,2.
This bulge is the chief complaint in most patients undergoing abdominoplasty and is
most often caused by rectal diastasis. It may be associated with musculoaponeurotic
flaccidity or physiological incompetence, which may have predisposing and aggravating
factors, such as age, multiparity, significant weight loss in obese patients, and
cesarean section.
The degree of competence of the anterior abdominal wall depends on the balance among
the intra-abdominal pressure, visceral movements, diaphragm, and muscular and aponeurosis
tensions, determining the presence of abdominal protuberances3,4.
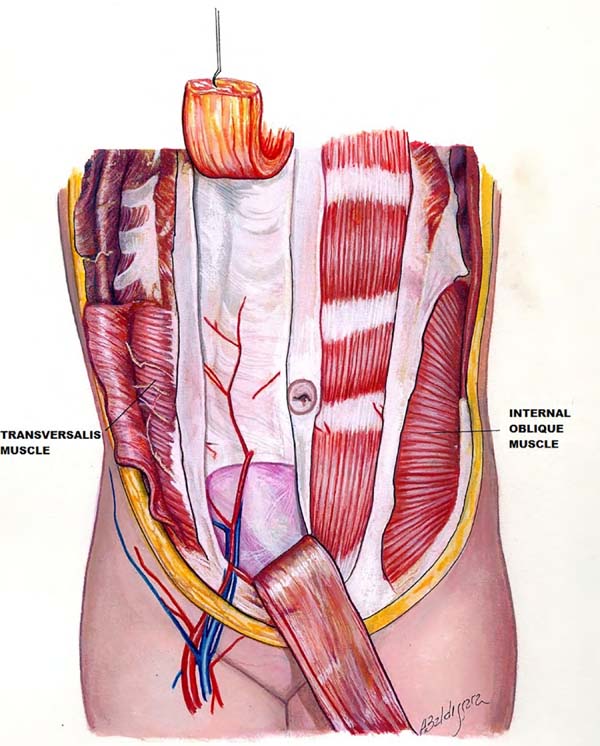
We believe that the protuberances are caused by the diastasis of the rectus abdominis
muscle and abdominal wall musculoaponeurotic flaccidity. Therefore, we considered
the transversalis fascia and transverse muscle the most important components of the
abdomen (Figure 1). We initiated the study in 1993, proposing the treatment by strengthening these
structures with polypropylene mesh1,5,6.
Figure 1 - Front view of the muscle distribution and arcuate line. Rectus abdominus is located
beneath the arcuate line and the aponeurosis of the internal oblique and transverse
muscles of the abdomen, which merge and pass superficially to the mm.
Figure 1 - Front view of the muscle distribution and arcuate line. Rectus abdominus is located
beneath the arcuate line and the aponeurosis of the internal oblique and transverse
muscles of the abdomen, which merge and pass superficially to the mm.
METHODS
In 32 years of professional practice, 925 patients were treated with the body contouring
surgery. In this period, we observed patients with prominent abdomen showing unsatisfactory
results or recurrences.
Fifteen patients were treated (Table 1). Seven patients who underwent primary abdominoplasty and eight patients who underwent
secondary abdominoplasty showed an abdominal bulge even after abdominoplasty, and
consequently, were not satisfied with the result1,5.
Table 1 - Patients who underwent treatment with a polypropylene mesh
| |
Patient |
Age (years) |
Primary Procedure |
Secondary Procedure |
Complications |
Results |
| 1 |
C.S.M.A.T. |
52 |
Abdominoplasty + plication of the rectus abdominis muscle + external oblique flap
+ liposuction
|
After 2 years: Abdominoplasty with a polypropylene mesh |
None |
Satisfactory |
| 2 |
M.E.B.P." |
42 |
Abdominoplasty + plication of the rectus abdominis muscle + external oblique flap
+ liposuction
|
After 14 years: Abdominoplasty with a polypropylene mesh |
None |
Satisfactory |
| 3 |
M.G.E. |
41 |
Miniabdominoplasty + plication of the rectus abdominis muscle + external oblique flap
+ liposuction
|
After 6 years: Abdominoplasty with a polypropylene mesh |
None |
Satisfactory |
| 4 |
R.C.M.A. |
40 |
Miniabdominoplasty + plication of the rectus abdominis muscle + liposuction |
After 1 year: Abdominoplasty with a polypropylene mesh |
None |
Satisfactory |
| 5 |
T.M.A.B. |
52 |
Abdominoplasty + plication of the rectus abdominis muscle + liposuction |
After 15 years: Abdominoplasty with a polypropylene mesh |
Chronic pain |
Satisfactory |
| 6 |
T.J. |
70 |
Abdominoplasty + polypropylene mesh + liposuction |
- |
Chronic pain |
Satisfactory |
| 7 |
C.X.* |
34 |
Fleur-de-Lis abdominoplasty + polypropylene mesh + plication of the rectus abdominis
muscle + liposuction
|
- |
None |
Satisfactory |
| 8 |
A.M.N. |
55 |
Abdominoplasty + polypropylene mesh + liposuction |
- |
None |
Satisfactory |
| 9 |
L.E.M.C.B. |
51 |
Abdominoplasty + polypropylene mesh + plication of the rectus abdominis muscle + liposuction |
- |
None |
Satisfactory |
| 10 |
A.I. |
46 |
Abdominoplasty + polypropylene mesh + plication of the rectus abdominis muscle + liposuction |
- |
None |
Satisfactory |
| 11 |
O.A.P.* |
40 |
Anchor abdominoplasty + polypropylene mesh + plication of the rectus abdominis muscle
+ liposuction
|
- |
None |
Satisfactory |
| 12 |
R.F.S. |
31 |
Abdominoplasty + polypropylene mesh + plication of the rectus abdominis muscle + external
oblique flap + liposuction
|
- |
Umbilical fistula |
Satisfactory |
| 13 |
R.S.C. |
25 |
Miniabdominoplasty + plication of the rectus abdominis muscle + liposuction |
After 3 years: Miniabdominoplasty + polypropylene mesh |
None |
Satisfactory |
| 14 |
E.C.G. |
30 |
Vertical abdominoplasty + polypropylene mesh + liposuction |
- |
None |
Satisfactory |
| 15 |
V.C.H.R. |
53 |
Abdominoplasty + plication of the rectus abdominis muscle + liposuction |
After 20 years: Abdominoplasty with a polypropylene mesh |
None |
Satisfactory |
Table 1 - Patients who underwent treatment with a polypropylene mesh
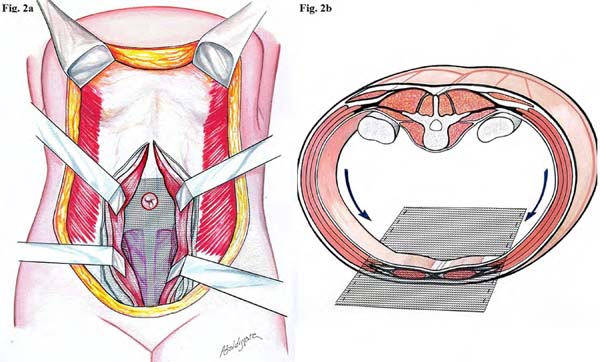
These patients underwent abdominoplasty with a suprapubic incision, which has a curved
line of superior concavity than the pre-existing scar. Subsequently, the subcutaneous
flap was raised, xiphoid process perforated, and linea alba incised to dissect the
rectus abdominis muscle of the posterior aponeurosis layer and transverse fascia,
reaching the external border of the rectus abdominis muscle on both sides (Figure 2). We applied the polypropylene mesh in direct contact with the deep aponeurosis layer
and transverse fascia, fixing it cranially to the xiphoid process, caudally to the
pubis at the origin of the pyramidalis muscle, and laterally to the musculoaponeurotic
complex of the oblique and transverse muscles (Figures 3A, 3B and 3C). The mesh was sutured with Prolene 0, U-stitches and was distended over the transverse
fascia and posterior sheath of the rectus abdominis muscle, resecting their excesses6,7. Subsequently, the rectus abdominis muscle was continuously sutured (Figures 4A, 4B and 4C). The suction drainage was left underneath the dermal fat flap and closed in three
planes.
Figure 2 - Position of the polypropylene mesh in the submuscular plane. A: The image shows the
submuscular position of the polypropylene mesh fixed anterior to the transversalis
fascia, with U-stiches and plication of the mm. Rectus Abdominis; B: The approximation
and repositioning of the intra-abdominal contents and traction vectors are also observed.
Figure 2 - Position of the polypropylene mesh in the submuscular plane. A: The image shows the
submuscular position of the polypropylene mesh fixed anterior to the transversalis
fascia, with U-stiches and plication of the mm. Rectus Abdominis; B: The approximation
and repositioning of the intra-abdominal contents and traction vectors are also observed.
Figure 3A - Patient was reinforced with a polypropylene mesh. A and B: Preoperative patient with abdominal bulge.
Figure 3A - Patient was reinforced with a polypropylene mesh. A and B: Preoperative patient with abdominal bulge.
Figure 3B - Patient was reinforced with a polypropylene mesh. C and D: Three years after abdominoplasty, the patient complained of recurrent abdominal bulge
in the lower abdomen.
Figure 3B - Patient was reinforced with a polypropylene mesh. C and D: Three years after abdominoplasty, the patient complained of recurrent abdominal bulge
in the lower abdomen.
Figure 3C - Patient was reinforced with a polypropylene mesh. E and F: Five years after secondary abdominoplasty with a polypropylene mesh. We can observe
an improvement in the infraumbilical bulge after the mesh was placed.
Figure 3C - Patient was reinforced with a polypropylene mesh. E and F: Five years after secondary abdominoplasty with a polypropylene mesh. We can observe
an improvement in the infraumbilical bulge after the mesh was placed.
Figure 4A - The other patient reinforced with a polypropylene mesh. A and B: The patient was not satisfied with abdominoplasty performed by another surgeon because
of the lower and supraumbilical bulge.
Figure 4A - The other patient reinforced with a polypropylene mesh. A and B: The patient was not satisfied with abdominoplasty performed by another surgeon because
of the lower and supraumbilical bulge.
Figure 4B - The other patient reinforced with a polypropylene mesh. C and D: Increased umbilical scar and supraumbilical abdomen bulge 14 years after postoperative
secondary abdominoplasty.
Figure 4B - The other patient reinforced with a polypropylene mesh. C and D: Increased umbilical scar and supraumbilical abdomen bulge 14 years after postoperative
secondary abdominoplasty.
Figure 4C - The other patient reinforced with a polypropylene mesh. E and F: Improvement in the umbilical scar and the abdominal wall with a slight concavity
one year after abdominoplasty with a polypropylene mesh.
Figure 4C - The other patient reinforced with a polypropylene mesh. E and F: Improvement in the umbilical scar and the abdominal wall with a slight concavity
one year after abdominoplasty with a polypropylene mesh.
All patients attended the follow-up for five postoperative years and underwent annual
ultrasound examinations of the abdominal wall.
RESULTS
In our observation period, the esthetic results and integrity of the abdominal wall
were maintained in the long term and showed no recurrences.
For example, we found a representative case of unsatisfactory results following abdominoplasty
by another surgeon in a 42-year-old patient. After the evaluation, a secondary abdominoplasty
was performed with plication of the rectus abdominis muscle and external oblique aponeurosis
flap8. Despite improvement, a slight upper abdominal projection persisted. She returned
14 years later with the complaint of increased upper abdominal projection. We indicated
the performance of an abdominoplasty with reinforcement of the abdominal wall using
a polypropylene mesh, fully correcting the abdominal projection, even in the sitting
position.
Three complications were observed in our cases. Two patients had localized chronic
intermittent pain (laparodinias), which improved with conventional anti-inflammatory
drugs and was treated with corticosteroid infiltrations. Another complication was
an early umbilical fistula with spontaneous and rapid resolution, regardless of the
proposal.
The satisfaction assessments were obtained using the Body-QoL® instrument, which is structured in 5 domains with 20 questions in total. The questions
are presented as Likert-type statements in which the patient expresses his/her degree
of agreement of that statement9. We administered this instrument in the patients in the postoperative period of 6
months and 5 years, considering the answers in the questionnaires as the final result.
DISCUSSION
It is concluded that this treatment cannot be indicated as the first-line treatment,
as many patients with musculoaponeurotic flaccidity obtained satisfactory results
with the conventional treatment and therefore, reinforcement with the polypropylene
mesh was not necessary. It is necessary to correctly evaluate the recurrent factors,
as this treatment consists of an aggressive intervention, which we only recommend
for select cases.
The surgeon should know and consider the miodynamism and importance of muscle layers
in the appearance of abdominal protuberances, the most important element being the
transverse abdominal muscle10. The external oblique muscle causes an upward lateral traction and the descending
internal oblique muscle causes two equal antagonistic forces, acting harmoniously.
On the other hand, the longitudinal position of the rectus abdominis muscle helps
approach the thorax as an antagonist of the spinal muscles3,4,10. Similarly, the transverse muscle allows contraction and expansion of the abdominal
wall, keeping the viscera in the correct position and bringing the anterolateral muscles
against the strong spine4. These traction forces make the linea alba a neutral support point, allowing the
intra-abdominal content to be in perfect balance, promoting normal functioning of
the upper diaphragm, which facilitates pulmonary ventilation and the dynamics of the
mesenteric complex. The rupture of this balance may lead to consequences, such as
rectal diastasis, increase in the abdominal area, change in the center of gravity,
change in the lumbar spine, low back pain, decrease in the diaphragmatic domes with
decreased pulmonary ventilation, and digestive disturbances resulting from visceral
dislocations4. Our proposal is based on the abdominal dynamics, reinforcing the aponeurosis muscle
wall, and consequently, restoring abdominal balance.
In our proposal, the mesh is placed over the transverse fascia and posterior to the
abdominal rectum, preventing the patient from experiencing the sensation of a foreign
body and providing additional protection and a reduced possibility of infection11.
CONCLUSION
One disadvantage we found in our experience was the episode of intermittent localized
pain (laparodinias). It is important to note that pain is a subjective complication,
and improvement with anti-inflammatory drugs is possible, in addition to determining
the correct use of polypropylene mesh in each case. New materials such as ADM and
ULTRAPRO will probably be incorporated as the technique evolves, as they provide improved
safety owing to the lower number of reactions in other procedures11.
COLLABORATIONS
|
AMLC
|
Analysis and/or data interpretation, Conception and design study, Final manuscript
approval, Realization of operations and/or trials, Supervision
|
|
JFJS
|
Analysis and/or data interpretation, Conception and design study, Conceptualization,
Data Curation, Realization of operations and/or trials, Writing - Original Draft Preparation,
Writing - Review & Editing
|
|
KSCM
|
Conception and design study, Conceptualization, Data Curation, Realization of operations
and/or trials, Writing - Original Draft Preparation, Writing - Review & Editing
|
REFERENCES
1. Caldeira AML, Lucas A. Flacidez músculo-aponeurótica abdominal intensa y su tratamiento.
Cir Plást Iberolatinoam. 1998;24(1):9-15.
2. Caldeira AML, Robles MBM. Chapter 30 – Challenges in Abdominoplasty, In: Avelar J,
editor. New Concepts on Abdominoplasty and Further Applications. Switzerland: Springer
Internacional Publishing. 2016. p.481-495. DOI: 10.1007/978-3-319-27851-3_30
3. Testut L, Jacob O. Traité d’Anatomie Topographique. Avec Applications Médico-Chirurgicales.
Paris: Gaston Doin; 1909.
4. Alcino LS, Pimenta LG. Técnica da Transposição Peritoneoaponeurótica Longitudinal
Bilateral. In: Alcino LS, Luiz GP, editores. Hérnia Incisional. São Paulo: MEDSI;
2004.
5. Caldeira AML, Niéves PA, Oliveira AL. Cirurgia do Contorno Corporal – Reflexões sobre
um novo enfoque da cirurgia plástica do abdome. I – Classificações das deformidades
abdominais e suas correlações cirúrgicas. Rev Bras Cir. 1990; 80(2):95-104.
6. Usher FC, Ochsner J, Tuttle LL. Use of marlex mesh in the repair of incisional hernias.
Am Surg. 1958 Dec;24(12):969-74.
7. Caldeira AML, Niéves PA, Oliveira AL. Cirurgia do Contorno Corporal – Reflexões sobre
um novo enfoque da cirurgia plástica do abdome – II Parte. Rev Bras Cir. 1990;80(3):169-186.
8. Psillakis JM. Abdominoplasty: Some ideas to improve results. Aesth Plast Surg. 1978
Dec;2(1):205-215. DOI: 10.1007/bjs.1800590134
9. Anson BJ, McVay CB. Surgical Anatomy. 6th ed. Philadelphia: WB Sauders; 1984.
10. Danilla S, Dominguez C, Cuevas P, et al. The Body-QoL®: measuring patient reported
outcomes in body contouring surgery patients. Aesth Plast Surg. 2014 Jun;38(3):575-583.
DOI: 10.1007/ s00266-014-0302-x DOI: https://doi.org/10.1007/s00266-014-0302-x
11. Caldeira AML, Carrión K, Jaulis J. Repair of the Severe Muscle Aponeurotic Abdominal
Laxity with Alloplastic Mesh in Aesthetic Abdominoplasty. Aesth Plast Surg. 2018 Feb;42(4):1039-1049.
DOI: https://doi.org/10.1007/s00266-018-1101-6 DOI: https://doi. org/10.1007/s00266-018-1101-6
1. Instituto Avançado de Cirurgia Plástica Alberto Caldeira, Rio de Janeiro, RJ, Brazil.
Corresponding author: Alberto Magno Lott Caldeira Rua Visconde de Pirajá, 414, Grupo 1012, Ipanema, Rio de Janeiro, RJ, Brasil. Zip
Code: 22410-002. E-mail: lottcaldeira@gmail.com
Article received: January 24, 2019.
Article accepted: June 24, 2019.
Institution: Instituto Avançado de Cirurgia Plástica, Hospital Casa Evangélico, Rio
de Janeiro, RJ, Brazil.
Conflicts of interest: none.