

Case Report - Year 2019 - Volume 34 -
Idiopathic scrotal calcinosis: an unusual skin disorder
Calcinose idiopática escrotal: uma inabitual desordem de pele
ABSTRACT
Idiopathic scrotal calcinosis is a rare benign entity. Patients affected by scrotal calcinosis usually do not have other associated symptoms. We report the case of a 30-yearold man with several calcified nodules in the scrotal sac with onset at age 15 years. A complete surgical excision of the nodules was performed, and the patient recovered well with satisfactory aesthetic and functional results.
Keywords: Scrotum; Calcinosis; Epidermal cyst; Reconstructive surgical procedures; Surgical pathology
RESUMO
A calcinose escrotal idiopática é uma entidade rara, benigna. Não costuma ter outros sintomas associados. O caso reportado se trata de um paciente de 30 anos com diversos nódulos calcificados em bolsa escrotal, com 15 anos de evolução. Como medida terapêutica, foi realizada excisão cirúrgica completa dos nódulos, apresentando boa evolução cirúrgica e resultados estético e funcional satisfatórios.
Palavras-chave: Escroto; Calcinose; Cisto epidérmico; Procedimentos cirúrgicos reconstrutivos; Patologia cirúrgica
INTRODUCTION
Idiopathic scrotal calcinosis (SC) is a rare condition with few cases reported in the literature. It consists of multiple stony calcified nodules on the scrotal skin. It generally affects young men and is not associated with symptoms (pain, edema, flushing etc.) or increase in serum calcium and phosphate levels. Although several hypotheses have been proposed, the pathophysiology of SC has not yet been established1. Histopathologically, an SC is characterized by the presence of calcium deposits within the dermis surrounded by a foreign-body type granulomatous reaction2. Currently, surgical excision is the treatment of choice and provides satisfactory results, despite the lack of knowledge and controversies surrounding the origin of this disease. We describe a case of idiopathic scrotal calcinosis treated at the Plastic Surgery Department of the Medical School of the Federal University of Pelotas-RS.
CASE REPORT
Patient
We report the case of a 30-year-old man with multiple hardened nodules in the scrotum, with slow and painless growth and onset at 15 years of age. (Figure 1). The patient mainly complained of local aesthetics as he had difficulty in maintaining intimate relationships due to the appearance of the lesions. He had no history of metabolic, autoimmune, or neoplastic disease. He did not have any associated symptoms and no history of trauma and/or previous scrotal lesions or any comorbidities.
He used skin creams containing clobetasol and betamethasone (not simultaneously) several times, but without any effect. On physical examination, the scrotum was normal in size and consistency, with several white/yellowish stony nodules of various sizes covered by epithelium.
Serum calcium and phosphorus levels were within normal limits.
Surgical Technique
The surgery was performed under local anesthesia with a thin incision in the plane between the dermis and the dartos muscle. The calcified nodules were not anatomically separate and a single-stage resection was performed along with the surrounding epidermis. The nodules were removed and preserved for pathologic analysis and the wound was closed by approximation of the edges by primary closure using a 3-0 nylon suture.
The patient recovered well after surgery, without any complications. He had satisfactory aesthetic results (Figure 2), without any functional changes.
DISCUSSION
SC is classified into 3 types: metastatic, dystrophic, and idiopathic. In metastatic SC, serum levels of calcium and phosphorus are increased. In dystrophic SC, the levels of phosphorus and calcium are normal, but local conditions such as inflammation are present that promote calcium deposition. Idiopathic SC is not associated with any laboratory findings or history of trauma. It is a rare condition, and about 200 cases have been described so far3.
Lewinski was the first to describe this condition in 1883. SC is a rare benign condition that causes multiple, asymptomatic, painless nodules on the scrotal skin surface4. SC mainly occurs in early adulthood with an insidious onset, without any systemic disturbance of calcium/phosphorus metabolism.
The nodules are typically yellowish-white or dark, consisting of grouped or individual nodules, varying in quantity, and appear as calcium and phosphate deposits on the scrotal skin. Although the nodules are usually firm and asymptomatic, they may cause itching or pain, and the deposits may extrude through the skin as a white, chalk-like material after an episode of infection of the nodules2.
The etiology of SC has been controversial for a long time. The first studies on this subject suggested that SC was caused by a pathogen. However, no cellular elements, lipids or organisms were found within the calcified nodules to justify this theory. Later studies suggested that it originates from the dystrophic calcification of epidermoid cysts5.
Recent studies have stated that scrotal calcinosis may result from inflammation of the epidermis, with formation of dermal cysts followed by dystrophic calcification within the nodule, with migration of keratin from the adjacent cyst or dermis to a ruptured cell wall. Other studies, state that epidermal inclusion cysts play an important role in the pathogenesis of the disease6.
Recently, Pabuccuoglu et al. reported that degeneration and necrosis of the dartos muscle are the most important factors in the pathogenesis of this disorder. Additionally, it has been suggested that low-impact trauma plays an important role in the etiology of dystrophic calcification3.
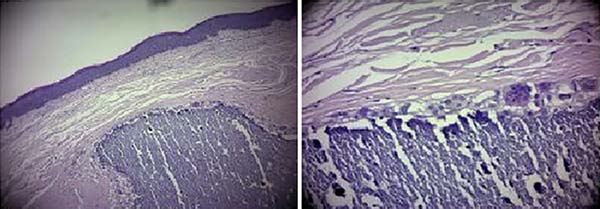
Histologically, an SC is characterized by the presence of variable calcium deposits within the dermis, and is commonly surrounded by a granulomatous foreign-body type reaction
Histopathologically, SC is characterized by the presence of calcium deposits of various sizes within the dermis, and usually surrounded by a foreign-body type granulomatous reaction2 (Figure 3).
Calcification of the keratin content is observed in some cysts, with little evidence of active inflammation. These lesions were variously described as sebaceous cysts, calcified steatocystoma, fibroma, atheroma, and xanthoma. Previous studies that reviewed histological data found no evidence of epithelial lining, residual cysts, and lipids and concluded that calcification was idiopathic, introducing the term idiopathic scrotal calcinosis2. Most cases are asymptomatic, and patients usually seek medical advice for aesthetic reasons, as in our case. Total excision is the treatment of choice, and primary closure is almost always possible because the scrotal skin is very flexible.
CONCLUSION
Although other etiologies are suspected, SC is still considered to be idiopathic; thus, further studies should continue investigating the cause for the development of idiopathic scrotal calcinosis. Moreover, good aesthetic results after resection and primary closure are factors that increase the indication for surgery, particularly when performed by an experienced surgeon that applies the concepts of plastic surgery in his/her routine.
REFERENCES
1. Solanki A, Narang S, Kathpalia R, Goel A. Scrotal calcinosis: pathogenetic link with epidermal cyst. BMJ Case Rep. 2015;2015:pii:bcr2015211163. DOI: https://doi.org/10.1136/bcr-2015-211163
2. Parlaktaş BS, Uluocak N, Köseoğlu RD, Erdemir F, Sezer E. Idiopathic scrotal calcinosis: A rare scrotal skin disorder. J Ankara Univer Fac Med. 2005;58(1):20-2.
3. Dubey S, Sharma R, Maheshwari V. Scrotal calcinosis: idiopathic or dystrophic? Dermatol Online J. 2010;16(2):5.
4. Akosa AB, Gilliland EA, Ali MH, Khoo CT. Idiopathic scrotal calcinosis: a possible aetiology reaffirmed. Br J Plast Surg. 1989;42(3):324-7. PMID: 2667677 DOI: https://doi.org/10.1016/0007-1226(89)90155-0
5. Shah V, Shet T. Scrotal calcinosis results from calcification of cysts derived from hair follicles: a series of 20 cases evaluating the spectrum of changes resulting in scrotal calcinosis. Am J Dermatopathol. 2007;29(2):172-5. DOI: https://doi.org/10.1097/01.dad.0000246465.25986.68
6. Khallouk A, Yazami OE, Mellas S, Tazi MF, El Fassi J, Farih MH. Idiopathic scrotal calcinosis: a non-elucidated pathogenesis and its surgical treatment. Rev Urol. 2011;13(2):95-7.
1. Universidade Federal de Pelotas, Departamento
de Cirurgia Plástica, Pelotas, RS, Brazil.
2. Hospital Ernesto Dornelles, Departamento de Cirurgia Geral, Porto Alegre, RS, Brazil.
Corresponding author: Fernando Passos da Rocha, Praça Piratinino de Almeida, 13, Centro, Pelotas, Rio Grande do Sul, Brazil. Zip Code 96015-360. E-mail: fprocha.sul@terra.com.br
Article received: August 10, 2018.
Article accepted: November 11, 2018.
Conflicts of interest: none.







 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter