INTRODUCTION
Abdominoplasty is one of the most common plastic surgeries performed in Brazil.
In 2015, data from the International Society of Aesthetic Plastic Surgery
(ISAPS) indicated that abdominoplasty was the fourth most common plastic surgery
performed worldwide1.
Functional changes, genetics, life habits, inadequate diet, lack of physical
exercise, pregnancy, weight loss, aesthetic alterations of the abdominal wall,
and other factors contribute to decreasing patient self-esteem and
well-being2,3.
For more than a century, plastic surgery has sought solutions to correct the
abdomen, initially by abdominoplasty and later with liposuction, which are the
two cosmetic surgeries most commonly performed in this anatomical area4.
The first descriptions of the surgical treatment of abdominal wall deformities
were associated with the correction of umbilical hernias, which required the
concomitant removal of fat and skin4,5.
In 1899, Kelly described a dermofat excision technique, elliptical and
transversal at the level of the umbilicus, in which skin and fat were resected
together, initiating a challenge for surgeons in the treatment of abdominal
deformities6.
In 1957, extensive dissection of the dermofat graft was standardized to
facilitate transposition of the navel, initiating this important phase in
abdominoplasty7.
In 1965, Callia positioned the horizontal incision in the suprapubic region,
extending it laterally toward the iliac crests and leaving the scar less
apparent. This type of incision has had large acceptance and is used today with
slight design variations. Pitanguy described rectus abdominis muscle plication
at the midline7,8.
The introduction of liposuction by Illouz in 1980 enabled the reduction of fat
volume of the body contour in patients with excessive adipose tissue without
excess or sagging skin. Between liposuction and plastic surgery of the abdomen
are intermediate modality interventions called partial abdominoplasties9.
Several surgical techniques aim to restore the abdominal contour10-12.
Abdominoplasty markings are performed using a ruler, protractor, compass, nylon
thread, toothpick, and pen and/or methylene blue, according to the surgeon’s
preference.
OBJECTIVE
To develop a surgical instrument that optimizes abdominoplasty marking time.
METHODS
Ethical Approval
The study was approved by the Ethics Research Committee (Comitê de Ética em
Pesquisa) of the Federal University of São Paulo (Universidade Federal de
São Paulo - Unifesp, no. 2355210116).
Precedence Search
A precedence search was performed in national and international patent
databases of the National Institute of Industrial Property (Instituto
Nacional da Propriedade Industrial)13.
A list of all patents concerning abdominoplasty marking was obtained with a
description of each patent and drawing.
Technological Innovation Nucleus
The invention report, drawings of the instrument, and documents needed to
request a filing application for the abdominoplasty marking instrument were
forwarded to the village consultancy.
Description and characteristics
A description of the features and functions of the abdominoplasty marking
instrument was created.
Illustration of use
Graphics were developed to identify each part of the instrument.
RESULTS
Description of the instrument components and characteristics
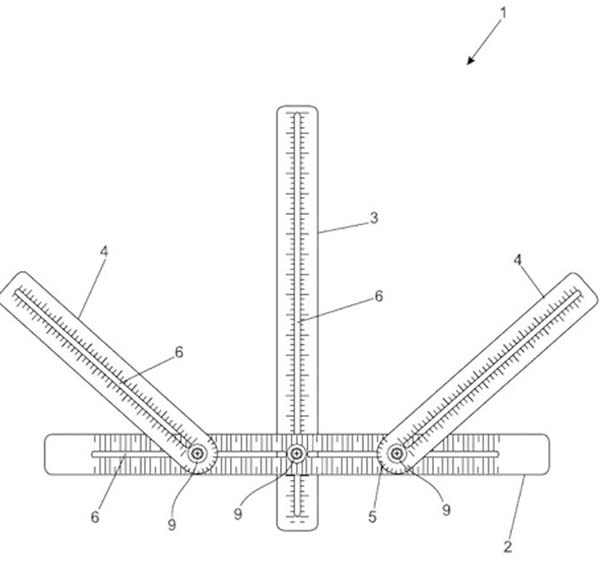
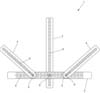
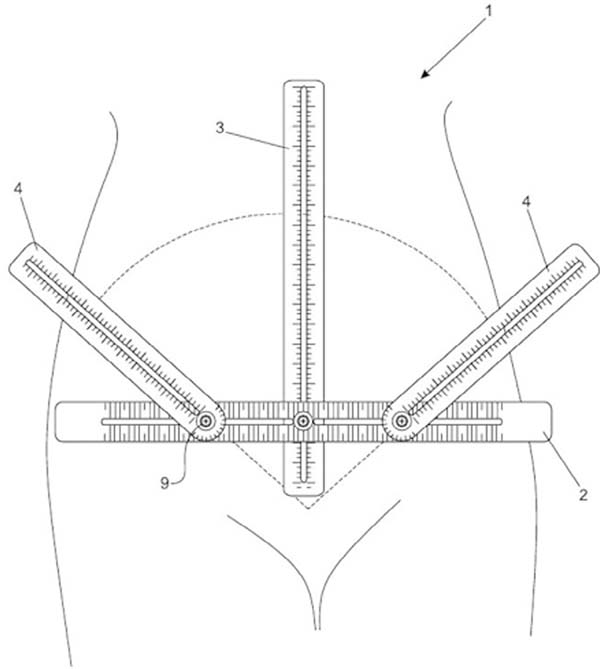
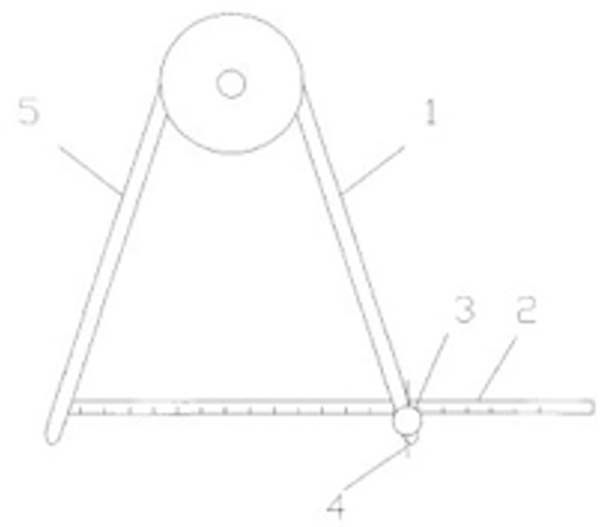
The instrument shown in Figures 1-5 that consists of a horizontal ruler
(1), which receives a vertical ruler (2) at its midpoint, and two pivotal
rulers (3) with a basal protractor (4), all marked in millimeters, and a
central void (5) that allows marking in this region with methylene blue or
pen and, consequently, the marking of the abdominoplasty procedure. It also
functions as a compass with laterally derived pivotal rulers (4) with a
basal-type protractor (5), all rulers (1, 3, 4) marked in millimeters on
both sides and a void in the central axis; a mechanism (9) formed by a screw
(10) attached to the blade of the slats (3 and 4) allows movement between
the parts.
Figure 1 - Diagram of the abdominoplasty marking instrument.
Figure 1 - Diagram of the abdominoplasty marking instrument.
Figure 2 - Exploded diagram of the abdominoplasty marking
instrument.
Figure 2 - Exploded diagram of the abdominoplasty marking
instrument.
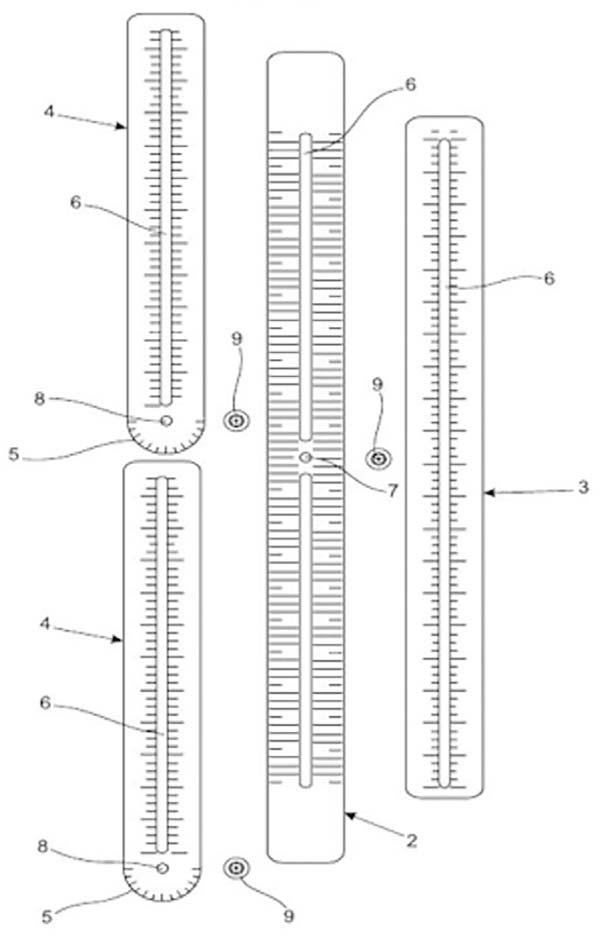
Figure 3 - Side view of the abdominoplasty marking instrument.
Figure 3 - Side view of the abdominoplasty marking instrument.
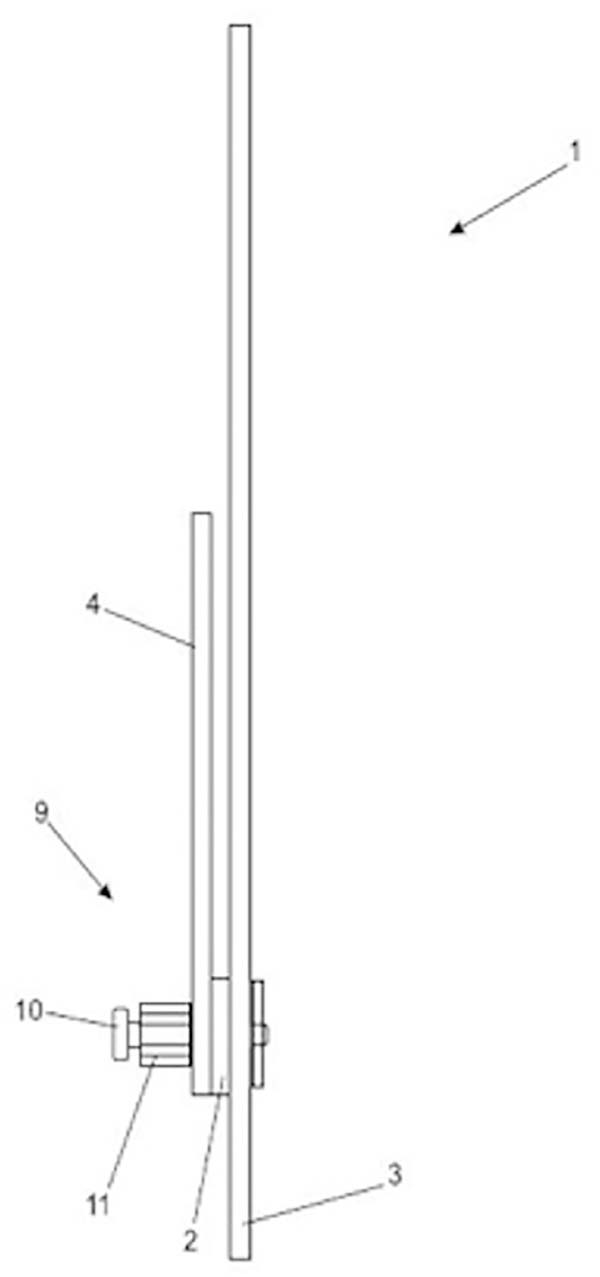
Figure 4 - Enlarged lateral detail of the inter-ruler joint of the
abdominoplasty marking instrument. Perspective view of the
abdominoplasty marking instrument in transport position.
Figure 4 - Enlarged lateral detail of the inter-ruler joint of the
abdominoplasty marking instrument. Perspective view of the
abdominoplasty marking instrument in transport position.
Figure 5 - Perspective view of the abdominoplasty marking instrument in
a demonstration of its use.
Figure 5 - Perspective view of the abdominoplasty marking instrument in
a demonstration of its use.
In one example of the invention, the joint between the rulers is achieved
using a mechanism (9) formed by a screw (10) fastened to the blade of the
slats (3 and 4) in which the tightening and loosening is affected by an
acrylic screw (11), but such a grip may be provided by another
movable/rotary mechanism.
Illustration of use
As shown in Figure 5, the methodology
of the abdominoplasty marking procedure involves positioning the instrument
on the patient’s abdomen, where a horizontal line is drawn in the suprapubic
region with extensions of approximately 12-14 cm, 7 cm from the vulvar
commissure and laterally toward the iliac crests by 6-7 cm on each side.
Areas in which liposuction can be performed are also demarcated using this
method. The measurements may vary according to the abdominal lipodystrophy
of each patient and the marking preferences of each surgeon.
Patents found in the precedence search
Chart 1 contains information of three
patents found in the precedence search.
Chart 1 - Precedence search of abdominoplasty marking patents.
| Patent |
Publication Date |
International Classification |
Country/Organization |
Inventors |
| PI 9702889-4 |
28/03/2000 |
A61B 17/00 |
Brazil |
Bernardo |
| Sérgio |
| Hochman |
| Reszetkowki |
| PI 0106759-1 |
14/10/2003 |
A61B 19/00 |
Brazil |
Anselmo |
| Luiz Penna |
| PI 9702889-4 |
01/2006 |
A618 5/00 |
China |
|
Chart 1 - Precedence search of abdominoplasty marking patents.
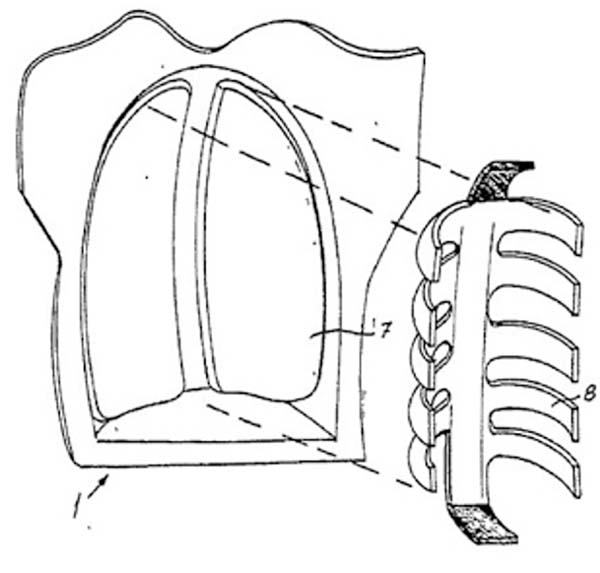
Description of patent PI 9702889-4
The PLASTIC SURGERY SIMULATOR KIT (Figure 6) provides the resident a practical learning opportunity for
various surgical techniques as well as periodic self-assessments. The kit
contains breasts (1) or a trunk replica including breasts and an abdomen (2)
and is made of suitable materials that simulate skin, glands, and muscles of
different colors to indicate the different layers of these regions of the
human body and that can constructively limit the “prohibited” areas of
access in certain surgical techniques so that, when sensitized (e.g. by the
touch of the scalpel), they trigger a visual or audible alarm in addition to
counting errors in an electronic panel.
Figure 6 - Plastic surgery simulator kit.
Figure 6 - Plastic surgery simulator kit.
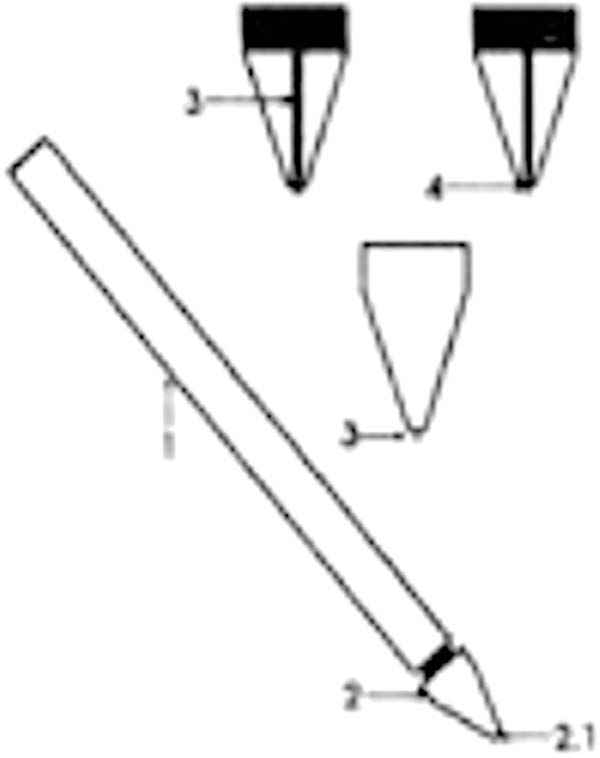
Description of patent PI 0106759-1
The surgical marking pen (Figure 7) is
used in superficial surgeries to demarcate the area to be operated. It is
composed of a rod (1) and a marker tip (2). This tip has an inner orifice
(2.1) into which appropriate graphite can be inserted (3), whose main
characteristic is to produce an accurate and fixed marking on human skin to
perfectly demarcate the area that will undergo incision, or even marker tip;
in this case, there is a cone needle (4) that, when pressed against the
skin, will release microquantities of ink, filling the space previously
occupied by the graphite and marking the area with the same efficiency.
Figure 7 - Surgical marking pen.
Figure 7 - Surgical marking pen.
Description of patent PI 9702889-4
The pincers used for navel marking in abdominal surgery (Figure 8) is composed of a scissors body. An extension
with a slot in the middle is present on one of its faces with the aim of
precisely and definitely locating the navel beneath the skin. On the other
side is an extension at which a navel marking device of various forms is
positioned on the skin.
Figure 8 - Navel marking pincers.
Figure 8 - Navel marking pincers.
Public domain instruments used for abdominoplasty marking
The marking of abdominoplasty surgeries is performed according to the
lipodystrophy of each patient and the surgeon’s marking preferences.
Chart 2 contains public domain tools
used for abdominoplasty marking.
Chart 2 - Public domain tools used for abdominoplasty marking.
| Public domain instruments |
| Instrument |
Purpose |
| Ruler |
Draw straight line segments and measure short
distances
|
| Compass |
Plot arcs of circumference and mark a segment
in a straight line
|
| Protractor |
Measure angles |
| Suture wire |
Join tissues and mark straight lines with
dyes
|
| Pen |
Write, draw, demarcate |
| Methylene blue |
Color |
| Toothpick |
Used as a pen when associated with dyes |
Chart 2 - Public domain tools used for abdominoplasty marking.
Description of the ruler
The origin of the word ruler is French and means “law or rule.” Rulers were
found in excavations in Mohenjo-Daro in 1500 B.C. This is an instrument used
to draw straight lines made in wood, plastic, or metal with measurements
marked in millimeters or centimeters (http://www.reguaonline.com/sobre-a-regua.html)14.
Description of the compass
The compass is a drawing instrument that makes circumferential arcs. It is
also used to mark a segment on a line of equal length to that of another
given segment and solve some types of geometric problems, such as
constructing a hexagon or finding the center of a circle15.
Description of the protractor
A protractor is an instrument that is used to measure angles. It is composed
of a circular scale, or circle sections, divided and marked at angles spaced
regularly as those on a ruler. Its use is diversified in education,
mathematics, engineering, surveying, construction, and various other
activities that require the precise measurement of angles. There are fixed
360°, 180°, and 90° protractors. Protractors can measure angles not only in
degrees but also in thousandths of a degree, such as those used by the
military for shooting applications16.
Description of suture wire
Suturing is a very important step in the surgical procedure. From ancient
times, a large number of suturing materials have been tested and used, such
as vegetable fibers, resins, tendons, intestines of various animals, horse
hair, and gold filaments. One of the earliest mentions of suturing is
recorded in Egyptian writing, which dates from 3500 B.C. In the
13th century, surgeons began to worry not only about the
nature of the material used for suturing but also about antisepsis. Thus,
the trend of using a variety of sterilized suture threads with pre-installed
needles that are supplied ready to use began17.
Description of the pen
The pen is an instrument used for writing with ink. Even today, students use
it worldwide for schoolwork. Ballpoint pens, which are mainly used today,
were invented in 1937 by the Hungarian Ladislao Biro, based on a pen that
did not erase and the ink did not dry in the deposit, unlike old fountain
pens.
The pens vary from simple to sophisticated and elegant, such as those
commonly used by professionals, and of various colors. Even today they are
used worldwide18.
Description of methylene blue
In 1876, Caro synthesized methylene blue; it has subsequently had various
uses in medical research. Methylene blue is an aromatic heterocyclic
compound that is solid dark green, soluble in water, and produces an
odorless blue solution. Methylene blue dye is used as a bacteriological dye
and indicator. It has many applications in various fields, such as biology
and chemistry19.
Description of the toothpick
Toothpicks are small rods usually made of wood or plastic that are frequently
used to remove detritus from the teeth, especially after meals, that have
existed for hundreds of years. The toothpick usually has one or two sharply
tapered ends to ensure better insertion between the teeth20.
A chart was prepared with the patent data found in the precedence search with
International Patent Classification identification number and code, inventor
name(s), date of publication, and place of registration.
Given the patents mentioned previously, comparisons were made with the design
of the marking instrument presented in this thesis.
Comparison between the study instrument and patent PI 9702889-4
The Plastic Surgery Simulator Kit (Figure 6) is used to train students and residents to perform surgical
techniques. The differences between the abdominoplasty marking instrument
and patent PI 9702889-4 are described in Chart 3.
Chart 3 - Comparison between the study instrument and patent PI
9702889-4.
| Study Instrument |
PI 9702889-4 |
| Advantage |
Disadvantage |
Advantage |
Disadvantage |
| Articulated mold for abdominoplasty
marking
|
Does not signal danger zones |
Simulators of "organs" to train surgical
techniques with flags of danger zones
|
Restricted to training |
Chart 3 - Comparison between the study instrument and patent PI
9702889-4.
Comparison of study instrument and patent PI 0106759-1
The surgical marking pen (Figure 7) is
used to delineate markings. The differences between the abdominoplasty
marking instrument and patent PI 0106759-1 are described in Chart 4.
Chart 4 - Comparison of study instrument and patent PI 0106759-1.
| Study Instrument |
PI 0106759-1 |
| Advantage |
Disadvantage |
Advantage |
Disadvantage |
| Articulated mold for
abdominoplasty marking
|
Does not signal danger
zones
|
Allows precise marking of human
skin
|
No demarcation mold |
Chart 4 - Comparison of study instrument and patent PI 0106759-1.
Comparison of study instrument and patent PI 0106759-1
The pincers used for navel marking in abdominal surgeries (Figure 8) is an instrument used in
abdominal surgeries; however, its use is limited to marking the navel,
unlike the study instrument, which demarcates the entire surgical area with
the exception of the navel (Chart 5).
Chart 5 - Comparison between study instrument and the pincers used for
navel marking in abdominal surgeries.
| STUDY INSTRUMENT |
Patent PI 0106759-1 |
| Advantages |
Disadvantages |
Advantages |
Disadvantages |
| Allows abdominoplasty marking |
Does not allow navel marking |
Allows navel marking only |
Use exclusive to the navel |
Chart 5 - Comparison between study instrument and the pincers used for
navel marking in abdominal surgeries.
Comparison of study instrument and the ruler
The instrument of study comprises a horizontal ruler that articulates with a
vertical ruler at its mid-point and two pivoting rulers. Unlike the public
domain ruler, the study ruler features a central empty space that allows
marking in this region with methylene blue or a pen to delineate the
abdominoplasty procedure. The instrument also has a mechanism formed by a
bolt fastened to the blade of the rulers that allows movement between the
parts, thus enabling the pivotal slides to also be used as a compass (Chart 6).
Chart 6 - Comparison of study instrument and the ruler.
| Study Instrument |
Public Domain Ruler |
| Advantages |
Disadvantages |
Advantages |
Disadvantages |
| Features a central void, a vertical ruler,
and two pivots that allow horizontal, vertical, and lateral
markings using the same instrument
|
Thesize of the vertical ruler does not allow
the marking to reach the xiphoid appendix positioned on the
pubis
|
Allows greater reach in the vertical position
line that defines the distance between the xiphoid
appendixand the pubis
|
Is able to providemeasures of straight lines
and angles in a single measure.
Different ruler
positions (vertical, horizontal, and oblique/lateral
bilaterally) and association with the compass are
required.
|
Chart 6 - Comparison of study instrument and the ruler.
After the precedence search, the study of the presented results, and the
development of the study instrument, a patent application as a utility model
was made and a deposit was made to the National Institute of Intellectual
Property.
DISCUSSION
In 2015, Brazil registered 1,224,300 plastic surgeries, including 758,590
abdominoplasties. A survey of these data has been performed by the ISAPS among
the total number of plastic surgeries performed by all plastic surgeons in each
of the participating countries15.
The search for improvements in body contour and quality of life has led to an
increase in demand for plastic surgery2,21,22.
Professionals should be able to accurately diagnose these deformities and know
the alternatives to provide adequate treatment2,21,23.
When choosing abdominoplasty, in accordance with the diagnosed deformity, the
marking can be made by the surgeon using a ruler, protractor, compass, nylon
thread, toothpick, pens, and methylene blue.
Preoperative surgical marking has been reported since the early days of plastic
surgery with Sushruta Samhita’s description of the use of vegetable leaves to
demarcate the nasal flaps and has progressed over centuries to the use of
leather and wax and then the more widespread use of incision drawings done with
paints and dyes starting in the 19th century8.
According to the pertinent literature, intraoperative surgical marking has
received less attention. Weiss’s study (1947) can be highlighted since it
advocated the use of technical pens and precision compasses made of aluminum
and
steel and sterilized in germicidal solutions for use during surgeries.
The use of this study instrument is performed in the following way: the
instrument is placed on the abdomen of the patient in the supine position during
the pre- or intraoperative period; and it defines the extension of the
horizontal trajectory of the suprapubic region, the extension of the vertical
trajectory of the vulvar commissure, and the tracing of the extension and the
angles of the lateral region toward the iliac crests. Using a pen or methylene
blue, the abdominoplasty marking is performed in the empty space of the
overlapping articulating and millimeter rulers in an easy, practical, and fast
manner.
In abdominoplasties performed after major weight loss, the utility of the
abdominoplasty marking instrument is reduced to the anchor technique, but the
use of its vertical and horizontal components to ensure symmetry and alignment
is of great value.
Since the scar’s final position results from the traction force of the abdominal
flap upward versus the traction suprapubic tissue resistance (pubic region)
versus marking precision, this study is important.
Details of the present invention
The conventional technique used to mark the abdominoplasty involves the use
of a ruler, protractor, compass, nylon thread, toothpick, pens, and
methylene blue.
The instrument developed in this study can be used in the pre- and
intraoperative periods, has an integrated ruler and compass, is articulated,
is easy to handle and transport, and features an empty space in the central
region of the rulers to reduce the incidence of misaligned markings and
blurring of methylene blue or ink of the chosen pen used for the
marking.
Target audience
The target audience for abdominoplasty marking instrument use includes
plastic surgery trainees and residents and plastic surgeons.
Applicability and social impact
Prevention of marking corrections;
Fewer instruments used; and
Facilitation of the surgical teaching of abdominoplasties in
accredited medical residency programs.
Perspectives
The perspective is that many surgeons and plastic surgery residency services
use the instrument developed in this study in their surgeries and teaching
practices.
CONCLUSION
Here we developed an abdominoplasty marking instrument that minimizes the amount
of material used and optimizes the marking time.
COLLABORATIONS
|
SAAP
|
Analysis and/or data interpretation, conception and design study,
conceptualization, data curation, investigation, methodology,
realization of operations and/or trials, resources, writing -
original draft preparation, writing - review & editing.
|
|
HCG
|
Final manuscript approval, project administration, supervision.
|
|
DN
|
Analysis and/or data interpretation, writing - review &
editing.
|
|
EBG
|
Conceptualization, supervision.
|
|
PRS
|
Conception and design study, data curation, writing - review &
editing.
|
|
PPP
|
Conception and design study, data curation.
|
|
ORS
|
Analysis and/or data interpretation, conception and design study.
|
|
LMF
|
Conceptualization, supervision.
|
REFERENCES
1. Azul de Metileno. Wikipédia; 2016 dez [acesso 2017 Mar 22].
Disponível em: https://pt.wikipedia.org/wiki/Azul_de_metileno
2. Brasil. Conselho Federal de Medicina. Resolução Nº. 2.131/2015, de
12 de novembro de 2015. Brasília: Diário Oficial da União;
2015.
3. Champion HR, Gallagher AG. Surgical simulation - a 'good idea whose
time has come'. BR J Surg. 2003;90(7):767-8.
4. Cintra W Jr, Modolin ML, Gemperli R, Gobbi CI, Faintuch J, Ferreira
MC. Quality of life after abdominoplasty in women after bariatric surgery. Obes
Surg. 2008;18(6):728-32.
5. Comess MS, Masson JK. A new method of skin marking. Plast Reconstr
Surg (1946). 1957;20(1):83-4.
6. Compasso. Wikipédia; 2017 mar [acesso 2017 Jan 12]. Disponível em:
https://pt.wikipedia.org/wiki/Compasso_(geometria)
7. Gorman PJ, Meier AH, Krummel TM. Simulation and virtual reality in
surgical education: real or unreal? Arch Surg.
1999;134(11):1203-8.
8. Granick MS, Heckler FR, Jones EW. Surgical skin-marking techniques.
Plast Reconstr Surg. 1987;79(4):573-80.
9. Grazer FM. Abdominoplasty. Plast Reconstr Surg.
1973;51(6):617-23.
10. Ideal Conference. Help us to improve research quality in surgery,
radiotherapy, physiotherapy and other áreas of complex intervention. The Ideal
Collaboration 2017 May. [acesso 2017 Jan 12]. Disponível em:http://www.ideal-collaboration.net
11. Ministério da Indústria, Comércio Exterior e Serviços. Instituto
Nacional da Propriedade Industrial. [acesso 2016 Jun]. Disponível em: http://www.inpi.gov.br/
12. International Society of Aesthetic Plastic Surgery (ISAPS). Global
survey released by ISAPS reports increase of over one million cosmetic and
aesthetic procedures perfomed in 2015. New York: ISAPS; 2016. 2
p.
13. Kneebone R. Simulation in surgical training: educational issues and
pratical implications. Med Educ. 2003;37(3):267-77.
14. Kohn LT, Corrigan JM, Donaldson M. To err is human: building a safer
health system. Washington: National Academy Press; 1999. 287 p.
15. Lenharo M. Cai número de plásticas no Brasil, mas país ainda é 2º no
ranking, diz estudo. São Paulo: G1; 2016. [acesso 2017 Jan 12]. Disponível em:
http://g1.globo.com/bemestar/noticia/2016/08/cai-numero-de-plasticas-no-brasil-mas-pais-ainda-e-2-no-ranking-diz-estudo.html
16. Paik AM, Mady LJ, Sood A, Eloy JA, Lee ES. A look inside the
courtroom: an analysis of 292 cosmetic breast surgery medical malpractice cases.
Aesthet Surg J. 2014;34(1):79-86.
17. Palito. Wikipédia; 2009 Jul [acesso 2017 Mar 25]. Disponível em:
https://pt.wikipedia.org/wiki/Palito
18. Caneta. Wikipédia 2009 jul [acesso 2017 Mar 25]. Disponível em:
https://pt.wikipedia.org/wiki/Caneta
19. Patané J, Patané CV. Legal responsibility of the plastic surgeon.
Propositions. Rev Arg Cir Plast. 1996;2(2):123-7.
20. Pitanguy I. Abdominal lipectomy: an aproach to it through an
analysis of 300 consecutive cases. Plast Reconst Surg.
1967;40(4):384-91.
21. Saldanha OR, Federico R, Daher PF, Malheiros AA, Carneiro PR,
Azevedo SF, et al. Lipoabdominoplasty. Plast Reconst Surg.
2009;124(3):934-42.
22. Tardelli HC, Vilela DBo, wartzmann GLES, Azevedo M, Mello Júnior AM,
Farina Júnior JA. Padronização cirúrgica das abdominoplastias em âncora
pós-gastroplastia. Rev Bras Cir Plást. 2011;26(2):266-74.
23. Tuma Junior P, Batista BPSN, Milian LS, Faria GEL, Milcheski DA,
Ferreira MC. Abdominoplastia vertical para tratamento de excesso de pele
abdominal após perdas ponderais maciças. Rev Bras Cir Plást.
2012;27(3):445-9.
1. Universidade Federal de São Paulo, São Paulo,
SP, Brazil.
2. Hospital Ana Costa, Serviço de Cirurgia
Plástica Dr. Ewaldo Bolivar, Santos, SP, Brazil.
3. Hospital São Lucas, Serviço de Cirurgia
Plástica Dr. Osvaldo Saldanha, Santos, SP, Brazil.
Corresponding author: Sabina Aparecida Alvarez de Paiva, Rua
Gonçalves Dias, nº 746 - Vila Tibério - Ribeirao Preto, SP, Brazil, Zip Code
14050-380. E-mail: sabinapaiva@hotmail.com
Article received: July 1, 2018.
Article accepted: October 1, 2018.
Conflicts of interest: none.