ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Retrospective analysis of a personal casuistry in reduction mammoplasty using the inferior pedicle technique for various indications
Análise retrospectiva da casuística pessoal em mamoplastia redutora utilizando a técnica de pedículo inferior em suas diferentes indicações
ABSTRACT
INTRODUCTION: Breast reduction surgery has been widely discussed, as different techniques are used to perform this procedure. The pursuit for aesthetics combined with surgical procedures that cause less unsightly scars promoted the development of alternative methods for breast reduction. The aim of this study was to conduct a bibliographic review of this technique, and present a personal casuistry regarding reduction mammoplasty using the inferior pedicle technique and compare it with those in the existing literature.
METHODS: This study describes the surgical approach used in 60 patients, their experience, and the results obtained with reduction mammoplasty performed with the inferior pedicle technique. The patients were followed up in outpatient settings at 15, 30, and 60 days; 3 months; 6 months; and 1 year.
RESULTS: Some complications occurred in the postoperative period but did not impair the final results. These include partial loss of sensitivity of the nipple-areolar complex, partial necrosis of the areola, hematomas, fat necrosis, and suture dehiscence.
CONCLUSIONS: The results obtained by using the inferior areolar complex in reduction mammoplasty proved, in my personal casuistry, to be similar to those found in the existing literature, with regard to complications and aesthetic outcomes. With this technique, the sensitivity and vascularization of the nipple-areola complex can be properly maintained, thus resulting in low complication rates. Moreover, it can also be used in medium-breast hypertrophy, mastopexy procedures, and silicone implant placement.
Keywords:
Mammoplasty; Plastic surgery; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: Cirurgia de redução de mama tem sido amplamente discutida a partir dos princípios de suas diferentes técnicas utilizadas neste processo. A busca da estética associada a procedimentos cirúrgicos que causem menos cicatrizes inestéticas tem promovido a busca de métodos alternativos de mama redução. O objetivo do presente estudo é realizar uma revisão bibliográfica desta técnica, apresentar minha casuística particular em mamoplastia redutora utilizando a técnica de pedículo inferior comparada à literatura mundial.
MÉTODOS: Descreve a abordagem cirúrgica do estudo com 60 pacientes relatando a experiência e os resultados da mamoplastia redutora pela técnica de pedículo inferior. As pacientes foram acompanhadas no consultório a cada 15, 30, 60 dias, 3 meses, 6 meses e 1 ano.
RESULTADOS: No pós-operatório algumas complicações sem repercussão no resultado final: perda parcial de sensibilidade do complexo aréolo-papilar, necrose parcial de aréola, hematomas, necrose gordurosa, deiscência de sutura.
CONCLUSÕES: A utilização da técnica de mamoplastia redutora com pedículo inferior areolado na minha casuística pessoal mostrou estar próxima da literatura mundial quanto às complicações e resultado estético. A técnica apresenta adequada manutenção da sensibilidade e vascularização do complexo aréolo-mamilar e baixos índices de complicações, podendo ser também empregada em mamas de médias hipertrofias e nas mastopexias e associada a prótese de silicone.
Palavras-chave:
Mamoplastia; Cirurgia plástica; Procedimentos cirúrgicos reconstrutivos.
INTRODUCTION
Reduction mammoplasty is a surgical procedure aimed at removing excess breast volume to attain a satisfactory shape, from an aesthetic point of view. It also allows correction of the consequences of excess breast volume in the thoracic and cervical spine regions.
To achieve this aim, many techniques have been developed over the recent years1,2. Each technique provides a specific result and, therefore, is specifically indicated for each case. The same technique cannot be used to correct problems that are due to different types of breast hypertrophy. However, the same technique can be used for different indications when the surgeon performing the technique has extensive knowledge about it.
The surgeon has the prerogative to learn and master other techniques that could be used for different types of breasts and anatomical variations. However, for breasts with exaggerated breast hypertrophy and a very wide distance from point A to the nipple-areolar complex (NAC), these techniques becomes difficult to apply because of the high risk of NAC necrosis3.
The inferior pedicle technique, first described by Ribeiro (1975)4, Robbins (1977)5, and Courtiss and Goldwyn (1977)6, proved to be a great alternative for breasts with severe mammary hypertrophy and an extreme distance between the NAC and point A. In 1979, Georgiade et al.7 presented their work on the inferior pedicle technique by introducing some important modifications regarding the width and depth of the inferior pedicle.
This technique can improve the shape of very large or small breasts, and can be an excellent technique for the correction of exaggerated ptosis. When combined with the use of silicone implants, it provides results that are even more satisfactory8.
Since the first article was published, literatures worldwide have shown that this technique has been widely used in North America but rarely used in Brazil9.
In many of the studies published worldwide, this technique has been shown to be easy to learn. It can also be performed without the occurrence of major complications, even when performed in breasts with severe hypertrophies10-12.
OBJECTIVE
The objective of this study was to present personal casuistry regarding reduction mammoplasty using the inferior pedicle technique and compare the occurrence of complications and aesthetic outcomes obtained in its various indications, in comparison with those reported in literatures worldwide. All the cases had different indications such as breast reductions due to gigantomastia, grade 4 breast ptosis with a great distance from the nipple-areolar complex and point A, combined use with silicone implants, and association with medium and large tumor resections due to breast pathology in cases of immediate breast reconstructions due to breast cancer.
METHODS
From 2008 to 2013, 60 patients aged between 20 and 85 years underwent breast reduction surgery. The reduction mammoplasty was performed by using the inferior pedicle technique, in the author's private clinic. All the cases were examined, and the technique was discussed with all the patients. The study followed the principles of the Declaration of Helsinki, and informed consent was obtained from all the patients.
Sixty patients from a private clinic who were indicated for reduction mammoplasty because of excessive breast augmentation and breast ptosis, and as alternative to immediate breast reconstruction were included in this study. In some cases, a silicone implant was used to provide a better breast contour, especially in the upper pole. All the patients underwent reduction mammoplasty performed by using the inferior pedicle technique, which has been described in the various references cited in this work.
All the patients underwent the surgery in a private clinic. The anesthetic techniques that were used varied from general anesthesia to high epidural block.
Description of the technique
The surgical technique was first reported in the 1970s4-7 and then was modified by Georgiade et al.7 in 1979.
Skin marking was performed routinely with the patient standing. Guideline marking was drawn in the sternal and mid-clavicular region.
Point A corresponds to the projection of the inframammary fold above the areola, coinciding with the average arm line. AB and AC flap arms make a 90° angle between each other and extend between 10 and 13 cm, in accordance with the evaluation performed with digital clamping of these lines up to the center of the inframammary fold. The base of the pedicle is drawn from the center point of the inframammary fold, which might vary between 6 and 10 cm, depending on the breast volume. The drawing of the pedicle narrows at the top, exceeding 3 to 5 cm of the NAC.
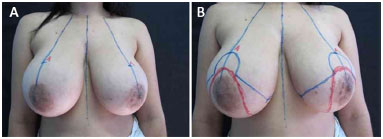
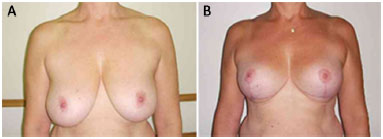
The excess subcutaneous cellular tissue that needs to be resected is carefully drawn to avoid extending outside the anatomical limits of the breast. A mold manufactured by following the principles of the original marking is placed to facilitate the design and symmetry of the marking, as shown in Figure 1. This mold is used as a simple guide to the original marking made when using the technique. The initial marking is the same as that previously made on the areolar site, as it is easy to make and follow the standard measures.
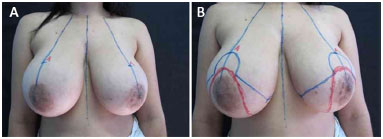 Figure 1.
Figure 1. Initial markings;
A: at point A;
B: in the inferior pedicle technique.
The surgery begins with the patient in the supine position, under general anesthesia or high epidural block, with local infiltration of an adrenaline solution and 250 mL of normal saline.
Infiltration with adrenaline at 1:200,000 is carried out in both breasts.
A de-epithelization of the inferior pedicle is performed, extending between 6 to 10 cm to the base and presenting a thickness of at least 5 to 6 cm, which extends 3 to 5 cm, even beyond the NAC.
The skin flaps detached from the breast were at least 2 to 3 cm thicker than those in the original technique4-7, and the upper pole of these flaps is maintained as thick as possible, avoiding flattening it.
After resection of the excess lateral and medial breast tissues, we performed pedicle fixation sutures to the pectoralis major fascia, avoiding lateralization of the pedicle. These sutures were no more than 5 cm from its base. The fixation of the pedicels should be performed as close as possible to the base to avoid compromising its mobility.
The sutures are made to join the skin flaps, the NAC site marking, and the natural emergence of the NAC (i.e., without tension and being slightly pulled with the aid of Gillies hooks). The sutures are made on two planes, with non-absorbable threads. The skin is closed with 3-0 monocryl and 4-0 monocryl thread (Figures 2-4).
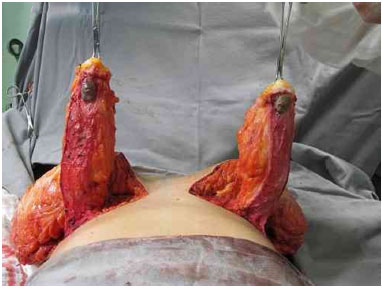
 Figure 2.
Figure 2. Inferior pedicle and medial edge of the upper flap.
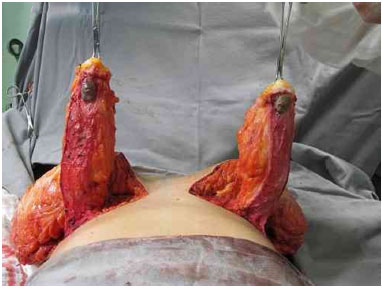 Figure 3.
Figure 3. Base, length, and thickness of the inferior pedicle.
 Figure 4.
Figure 4. Completion of the surgery with good perfusion of the areolas.
In some patients, continuous suction drains were used, contrary to those use in other patients and according to the volume of the operated breasts. The drain was removed on the third postoperative day. The patients were followed up in outpatient settings at 15, 30, and 60 days; 3 months; 6 months; and 1 year after surgery.
RESULTS
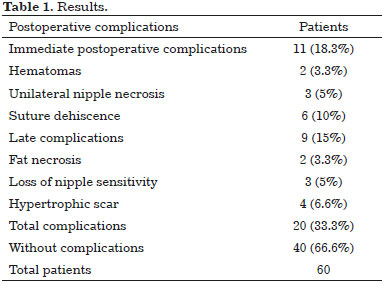
The study included 60 patients who underwent surgery between 2008 and 2013. Their ages ranged from 20 to 85 years, and breast reduction was the main surgical indication. During the postoperative period, the complications observed were comparable with those found in the existing literature, according to the statistics demonstrated in previous studies. These complications included the following: hematomas, areola necrosis, suture dehiscence, fat necrosis, loss of sensitivity of the areola and nipple, and hypertrophic scar, as listed in Table 1.
The complications were divided according to those found in the literature3,4,13.
Initial complications refer to those occurring in the immediate postoperative period, that is, 4 weeks after surgery. Late complications refer to those occurring in the late postoperative period, that is, 3 to 6 months after surgery.
Initial complications
Hematoma: Two patients presented with hematomas on one breast, which were resolved with drainage via a contra-incision and compressive dressings. This was probably due to not placing a drain and the resection of excess breast tissue.
NAC necrosis: Three patients presented with NAC necrosis. This was always unilateral and attributed to not having respected the pedicle thickness or observed its vascularization, and the possibility to perform fixation sutures above the desired limit, which could lead to a subsequent excessive NAC tension during its externalization. This often hindered its venous return, in addition to its vascularization.
Suture dehiscence: This occurred in 6 patients and always at the same point, that is, at the T-junction, where the lack of tension should be respected.
Late complications
Fat necrosis: Two patients had fat necrosis, which was confused with foreign-body granuloma. It usually occurs in the pedicle area, especially when very thick. The cases resolved when a late surgical reintervention was performed.
Loss of sensitivity of the areola and nipple: Three cases were diagnosed with the complication. Evaluation, according to the existing literature, was performed within 6 months to 1 year. One of the patients partially recovered, presenting areas of hypoesthesia after this period. Others have not been subsequently evaluated.
Hypertrophic scar: Four patients presented with hypertrophic scars, which were removed. A new suture was then made, and better results were obtained. This was probably caused by the patient's own healing or suturing performed.
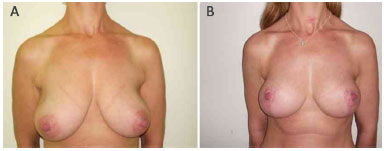
The preoperative and postoperative periods (6 months to 1 year) in 7 cases are illustrated in Figures 5 to 11.
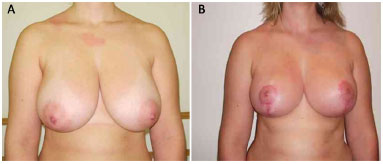
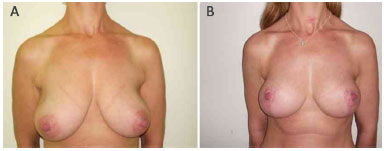 Figure 5.
Figure 5. Patient 1.
A: Preoperative;
B: Postoperative.
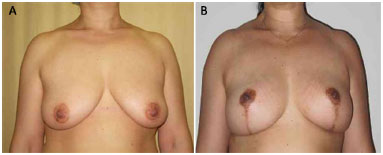
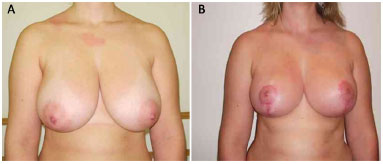 Figure 6.
Figure 6. Patient 2.
A: Preoperative;
B: Postoperative.
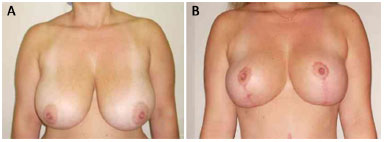
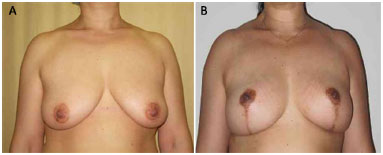 Figure 7.
Figure 7. Patient 5.
A: Preoperative;
B: Postoperative.
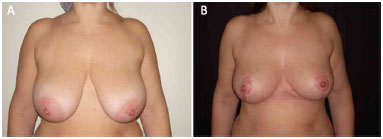
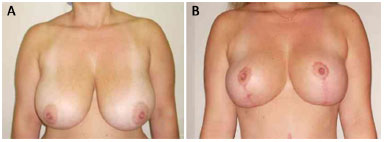 Figure 8.
Figure 8. Patient 6.
A: Preoperative;
B: Postoperative.
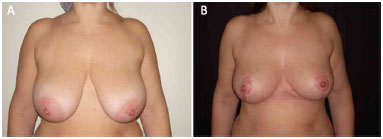 Figure 9.
Figure 9. Patient 7.
A: Preoperative;
B: Postoperative.
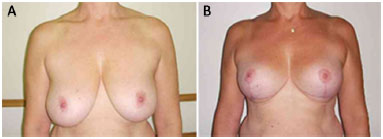 Figure 10.
Figure 10. Patient 9.
A: Preoperative;
B: Postoperative.
 Figure 11.
Figure 11. Patient 10.
A: Preoperative;
B: Postoperative.
DISCUSSION
Breast surgery has undergone major changes in the recent years, with the aim to reduce scars and to improve and maintain breast shape. Pacheco et al.13 report that breast reduction is mainly performed to correct the dysfunction and unaesthetic appearance of bulky breast and breast with ptosis. The surgery reduces the size of the breast, maintaining its symmetry, with minimal complications.
This technique was published by Ribeiro4, Robbins5, and Courtiss and Goldwyn6. They all published this technique almost at the same time but in different countries. The initial technique showed the large base of the pedicle as an alternative to proper NAC vascularization.
Georgiade et al.7 published the same technique with some modifications, mostly regarding the narrowing of the base of the pedicle and increased thickness, which allowed an excellent NAC vascularization.
Menderes et al.14 assessed that the symptoms presented in the preoperative period and the psychosocial aspects are also important for the indication of this surgery to reduce bulky breasts.
Arié15 points out that among the main complications observed in mammoplasty procedures are changes in the sensitivity of the nipple-areolar complex, unsightly scars, and postoperative breast pain.
Courtiss and Goldwyn6 suggested that patients with massive macromastia, or severe ptosis, should be candidates for breast reduction using the technique of inferior transposition of the pedicle, instead of the free nipple graft. With the inferior pedicle technique, ample blood supply to the nipple and areola continues, coming from the entire width of the inframammary fold.
Georgiade et al.7 discussed the advantages of the inferior pedicle technique as follows: (1) the breast size is predictable based on the preoperative marking; (2) all areas are direct visible, thus facilitating their removal and hemostasis; (3) the nipple is preserved along with its ductal system; (4) less loss of sensitivity, and (5) adequate blood supply.
Ariyan16 states that breast reduction is safe when the inferior pedicle technique is used, even in patients with massive macromastia. The same is reaffirmed by Castro et al.17, who advocated the use of the procedure for giant breasts and describe the technique in details.
According to Ribeiro4 and Arié15, when using the inferior base pedicle technique in mammoplasties, knowledge of the anatomical structures and distribution of the vascular network responsible for breasts vascularization is important. The results of this study were conclusive and enlightening, leaving no doubts about the behavior of the inferior pedicle cellular structures (dermo-lipo-glandular).
Migliori and Muldowney18 affirmed that the redundancy is obvious, to the extent that various techniques of breast reduction rely on completely different components of this vascular anatomy to sustain NAC. The inferior pedicle technique for breast reduction is well established as a reliable procedure. This technique underwent several modifications.
Similarly, Wallace et al.10 reported a rate of postoperative complications (5%) comparable with those in previous studies. Patient satisfaction was high (98%), with almost complete relief of preoperative symptoms. The concern with the resulting scars was low (2%) when the incisions followed the natural contour of the breast. The authors reported that this is a versatile flap for breasts of different shapes and size, which provides reproducible results. It can be used without increasing surgical time, in addition to its being an alternative to the free nipple graft technique.
Castillo and Hernández19 revealed that the outcome of the surgery was satisfactory in patients treated with the small-incision method. The authors stated that it can be applied in patients with gigantomastia and with different reduction techniques, known as mastoplasty procedures. Reis20 informed that the technique using the inferior base pedicle of the breast (dermo-lipo-glandular), when performed in breast reduction or lift, proved to be very safe. In addition, it provides satisfactory projection, shape, and support to the breasts for a longer period.
Based on the results of this study, we can conclude that the technique that uses the inferior base pedicle does not cause the formation of intramammary cysts.
In their study, Bezerra et al.9 commented that in Brazil, this technique is still poorly used despite the evidence of a large number of benefits. After 10 years' experience with this technique, the authors recommended the use of the inferior pedicle technique as a procedure with numerous advantages such as easy reproduction of the technique, with no significant increase in surgical time; usefulness for breasts of different shape and size, with long-lasting results; lower rate of complications in large resections and/or breast ptosis (e.g., NAC necrosis), in addition to the important maintenance of nipple sensitivity and erection, besides the great satisfaction of the patients.
Nahabedian and Mofid21 and Calderon Ortega et al.22 confirmed that despite the criticism of some authors about the fact that the inferior pedicle technique results in "lapless breasts," this could be avoided by leaving an areolate flap with more volume in its central portion associated with an increased thickness of the upper dermo-skin flap. This provides the appropriate and projected lap, without damaging the volume to be resected.
According to Saldanha et al.8, breast surgeries require a precise diagnosis for each breast type. Each patient has a different type of breast. Thus, a different strategy or surgical technique should be indicated. The plastic surgeon who intends to perform these types of procedures should broadly master several surgical techniques and strategies in order to achieve the best possible results, regardless of whether the patient presents mammary hypertrophy or gigantomastia.
According to Souza et al.12, breast plastic surgery focuses on fitness, suspension, and breast shape. Several techniques are used for breast reduction and mastopexy, with great attention to the pedicle responsible for NAC vascular supply. In order to understand the influence of each pedicle on late outcomes of mammoplasty, the authors pointed out that the measurement of the vertical distance between the more caudal part of the NAC and the horizontal scar in the inframammary groove (NAC-inframammary groove) can be obtained in a simple way, both in the immediate and late postoperative period.
Considering all conclusions presented herein and quick and effective learning curve, this study succeeded in consolidating the results obtained by other authors in using this technique.
If the results of this study are statistically analyzed and compared with those found in the existing literature worldwide, it can be inferred that the casuistry presented herein had many complications. However, these did not influence the final aesthetic results. All the complications were treated properly, without compromising the final outcomes.
CONCLUSIONS
In the comparison with the experiences reported in the literature, the conclusion is that breast reduction performed with the areolate inferior pedicle technique is an excellent procedure for breasts with large volumes (>1,000 g) and those presenting a large distance between point A and the NAC. This technique can also be used to correct smaller breasts, grade 4 breast ptosis, in mastopexy, and in silicone implant placement. The technique offers adequate maintenance of NAC sensitivity and vascularization, and presents lower rates of complications.
COLLABORATIONS
LDO Data analysis and/or interpretation; statistical analysis; final approval of the manuscript; conception and study design; realization of the surgical procedure and/or experiments; and writing of the manuscript or critical reviewing of its content.
REFERENCES
1. Pitanguy I, Salgado F, Radwansky HN. Reduções mamárias: técnicas pessoais sem descolamento cutâneo. In: Mélega JM, ed. Cirurgia plástica: fundamentos e arte. Cirurgia Estética. Rio de Janeiro: Médica e Científica; 2003. p. 477-84.
2. Rohrich RJ, Gosman AA, Brown SA, Tonadapu P, Foster B. Current preferences for breast reduction techniques: a survey of board-certified plastic surgeons 2002. Plast Reconstr Surg. 2004;114(7):1724-33.
3. Schlenz I, Rigel S, Schemper M, Kuzbari R. Alteration of nipple and areola sensitivity by reduction mammaplasty: a prospective comparison of five techniques. Plast Reconstr Surg. 2005;115(3):743-51.
4. Ribeiro L. A new technique for reduction mammaplasty. Plast Reconstr Surg. 1975;55(3):330-4.
5. Robbins TH. A reduction mammaplasty with the areola-nipple based on an inferior dermal pedicle. Plast Reconstr Surg. 1977;59(1):64-7.
6. Courtiss EH, Goldwyn RM. Reduction mammaplasty by the inferior pedicle technique. An alternative to free nipple and areola grafting for severe macromastia or extreme ptosis. Plast Reconstr Surg. 1977;59(4):500-7.
7. Georgiade NG, Serafin D, Morris R, Georgiade G. Reduction mammaplasty utilizing an inferior pedicle nipple-areolar flap. Ann Plast Surg. 1979;3(3):211-8.
8. Saldanha OR, Maloof RG, Dutra RT, Luz OAL, Saldanha Filho O, Saldanha CB. Mamaplastia redutora com implante de silicone. Rev Bras Cir Plást. 2010;25(2):317-24.
9. Bezerra FJF, Moura RMG, Silva Júnior VV. Mamoplastia redutora e simetrização de mama oposta em reconstrução mamária utilizando a técnica de pedículo inferior. Rev Bras Cir Plást. 2007;22(1):52-9.
10. Wallace WH, Thompson WO, Smith RA, Barraza KR, Davidson SF, Thompson JT 2nd. Reduction mammaplasty using the inferior pedicle technique. Ann Plast Surg. 1998;40(3):235-40.
11. Anger M, Schneider EJ, Souza CE, Nakayama LI. Mamoplastia redutora de pedículo inferior: sensibilidade aréolo-mamilar, indicações e resultados. Arq Catarin Med. 2001;30(3/4):32-7.
12. Souza AA, Faiwichow L, Ferreira AA, Simão TS, Pitol DN, Máximo FR. Avaliação das técnicas de mamoplastia quanto a sua influência tardia na distância do complexo areolopapilar ao sulco inframamário. Rev Bras Cir Plást. 2011;26(4):664-9.
13. Pacheco LMS, Pacheco AT, Batista KT. Mamoplastia redutora com pedículo medial: modificação na técnica de Skoog. Rev Bras Cir Plást. 2009;24(3):321-7.
14. Menderes A, Mola F, Vayvada H, Barutcu A. Evaluation of results from reduction mammaplasty: relief of symptoms and patient satisfaction. Aesthetic Plast Surg. 2005;29(2):83-7.
15. Arié G. Una nueva técnica de mastoplastia. Rev Latinoam Cir Plast. 1957;3(1):23-31.
16. Ariyan S. Reduction mammaplasty with the nipple-areola carried on a single, narrow inferior pedicle. Ann Plast Surg. 1980;5(3):167-77.
17. Castro CC, Salema RF, Ferreira VB, Gazola LA. Mamaplastia redutora pela técnica de pedículo dermogorduroso da base inferior. Rev Bras Cir. 1983;73(1):47-52.
18. Migliori MR, Muldowney JB. Breast reduction: the inferior pedicle as an axial pattern flap. Aesthet Surg J. 1997;17(1):55-7.
19. Castillo VMS, Hernández CMC. Incisiones mínimas para mastoplastias reductoras. Rev Cubana Cir. 2002;41(1):11-5.
20. Reis GMD. A técnica do pedículo de base inferior em mamaplastia redutora e mastopexia causa quistos? Rev Bras Cir Plást. 2006;21(2):73-6.
21. Nahabedian MY, Mofid MM. Viability and sensation of the nipple-areolar complex after reduction mammaplasty. Ann Plast Surg. 2002;49(1):24-31.
22. Calderon Ortega W, Arriagada Stuven J, Godoy Silanes M, Gomes SL. Anatomia y clinica de las mamoplastias de reducción según técnica del pedículo inferior. Rev Chil Cir. 1992;44(4):437-41.
Clínica DAlo de Cirurgia Plástica, Porto Alegre, RS, Brazil
Institution: Clínica DAlo de Cirurgia Plástica, Porto Alegre, RS, Brazil.
Corresponding author:
Leonardo DAlo de Oliveira
Rua Florêncio Ygartua, 270/909
Porto Alegre, RS, Brazil Zip Code 90430-010
E-mail: leonardodalo@yahoo.com.br
Article received: June 26, 2014.
Article accepted: November 15, 2014.
Conflicts of interest: none.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license