

Original Article - Year 2016 - Volume 31 -
Thin superior flap in mammoplasty procedures
Retalho superior delgado nas mamoplastias
ABSTRACT
INTRODUCTION: For being one of the procedures mostly performed in our environment, breast plastic surgery involves many technical variations and surgical strategies that provide the plastic surgeon with several options. The objective of this study was to evaluate the use of thin superior flap technique in mammoplasties.
METHODS: Over a period of 2 years, we selected 30 patients presenting with mammary hypertrophy and/or breast ptosis. A technique based on the inverted-T marking and Ribeiro's type IV inferiorly based flap was carried out. The intervention involved the production of a thin superior flap with a thickness of approximately 2 cm. This comprised 30% of the breast volume, while the inferior flap was responsible for the remaining 70%.
RESULTS: Three expert plastic surgeons evaluated the patients. The results showed that 91.5% of the women who underwent this procedure presented with excellent quality outcomes, while 6.9% had a good outcome. Further, a fair outcome was observed only in 1.6% of the patients, while poor outcomes were not obtained. The procedure had a complication rate of 2.6%, which included one case of infection, one of asymmetry, and two of unsightly scars.
CONCLUSION: The thin superior flap proved to be very effective in mammoplasties.
Keywords: Mammoplasty; Surgical flap; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A cirurgia plástica da mama, por se tratar de um dos procedimentos mais realizados no nosso meio, traz consigo muitas variações técnicas e de táticas cirúrgicas, que proporcionam ao profissional da área da Cirurgia Plástica várias opções técnicas. O objetivo foi avaliar a técnica do retalho superior delgado nas mamoplastias.
MÉTODOS: Foram selecionadas 30 pacientes, no período de 2 anos, que apresentavam hipertrofia mamária e/ou ptose mamária. Foi realizada uma técnica utilizando a marcação em T invertido e um retalho inferior número IV de Ribeiro. A modificação introduzida foi a confecção do retalho superior delgado com aproximadamente 2 cm de espessura computando 30% do volume mamário, sendo o retalho inferior responsável por 70% do volume.
RESULTADOS: Três colegas especialistas em Cirurgia Plástica por mais de 10 anos avaliaram as pacientes e pudemos observar um resultado no qual 91,5% das pacientes avaliadas se mostraram de ótima qualidade, 6,9% de boa qualidade e apenas 1,6% de resultados regulares, sem resultados ruins. Foram computados 2,6% de complicações, com um caso de infecção, um de assimetria e dois de cicatriz inestética.
CONCLUSÃO: O retalho superior delgado se mostrou muito eficaz nas mamoplastias.
Palavras-chave: Mamoplastia; Retalhos cirúrgicos; Procedimentos cirúrgicos reconstrutivos.
Mammary hypertrophy and breast ptosis are conditions commonly associated with various degrees of morbidity1-3. To solve these problems, modern treatment approaches rely on surgical maneuvers, which are considered essential for their implementation. During such procedures, the surgeons are required to be very careful with the anatomy of the region and function of the organ. The combination and/or modification of various techniques enables a wide range of behaviors that complement the plastic surgeon's arsenal and are used for the treatment of different changes observed in daily practice. The first aesthetic intervention and/or breast reconstructive surgery was performed at the beginning of the last century4.
The approach of replacing healthy tissue with a silicone implant to improve its shape and consistency has generated much debate. This treatment removes breast tissue and replaces it with a silicone implant, resulting in a graceful form and a consistent texture. The strong argument supporting this procedure is that the morbidity rate of using silicone implants is low. As such, there is an increasing willingness among patients to undergo this procedure5.
Better shape and texture can also be achieved with mobilization and fixation of the breast tissues. Therefore, the aim of this study was to carry out a procedure in which the breast volume is defined by Ribeiro's inferior flap6, accounting for 70% of the breast volume, and a thin superior flap is produced for coverage, representing 30% of the breast volume. Thus, we seek a similar result to that obtained by replacing breast tissue with an implant without the need to replace healthy tissue.
OBJECTIVE
To evaluate the thin superior flap technique in mammoplasties.
METHODS
We followed the principles of the Helsinki Declaration revised in 2000 as well as of the Resolution 196/96 of the National Health Council.
Study design
This is a primary, clinical, interventional, longitudinal, prospective and self-controlled study, which was performed at a single center.
Selection
We selected all patients undergoing mammoplasty in the period between October 2012 and October 2014, totaling 30 women. The age of the patients varied between 18 and 60 years, and they were all treated in the author's private clinic. All patients read and signed the Informed Consent Form.
Inclusion criteria
Women aged between 18 and 60 years, of any ethnicity, with a body mass index (BMI) ranging from 18.5 and 29.9 kg/cm2, and presenting with normal preoperative examinations results and an indication for reduction mammoplasty or mastopexy.
Non-inclusion criteria
Diagnosis or history of malignant breast disease, diabetes mellitus and other immunosuppressive disorders, immunosuppression, non-controlled chronic diseases, smokers or patients who cannot quit smoking for at least one month.
Exclusion criteria
Patients who did not show up for postoperative evaluations, pregnancy and a weight loss of more than 5 kg over 6 months postoperatively.
Surgical procedure
All patients selected underwent preoperative examinations, which included hematologic, heart, and radiological evaluations; and other specific exams, when indicated. All patients were photographed preoperatively and six months after surgery. Frontal as well as right and left lateral images were taken from the patients, whose right and left profiles were also photographed at a regular distance.
Administration of antibiotic prophylaxis with 2 g of cefazolin, antisepsis with 1% degerming chlorhexidine and 2% dye were followed by sedation, which was performed by an anesthesiologist.
With the patient in a supine position, sitting, at 45th on the operating table, we drew the classic markings of an inverted-T mammoplasty7,8 and a Ribeiro's type IV flap6. The size of its lower base varied from 6 cm to the entire length of the resected area. This flap will determine 70% of the final volume of the breast, which is in agreement with the patient's request (Figure 1).
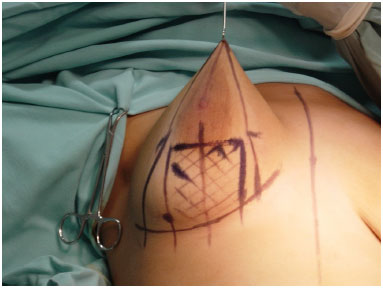
Figure 1. Final marking result of the inverted-T technique and inferior base flap.
A local anesthesia constituting 120 ml of a solution with 0.3% lidocaine and a concentration of epinephrine equal to 1: 300,000 was administered at the base of the breast. Incisions were then carried out according to previous markings, with the aim of starting skin resection in areas that have been buried.
An incision was made in the breast tissue 1 cm below the nipple-areolar complex (NAC) and in the dermis near the skin incisions. We then tilted the blade to produce a superior flap with an average thickness of 2 cm throughout its extension until the fascia of the pectoralis major muscle. This will determine 30% of the breast volume.
With one superior and one inferior flap produced with all the remaining breast tissue, we proceeded in manipulating the latter, either resecting the excess flap or not and leaving a volume that was sufficient to satisfy the dimensions of the breast according to our agreement with the patients. This resulted in 70% of breast volume6. In breast hypertrophies, we performed reduction of this flap from the internal and external sides and, when necessary, we reduced its thickness. In cases of mastopexy without tissue removal, this resection step is not carried out6 (Figures 2 and 3).
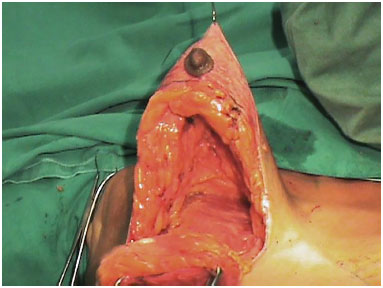
Figure 2. Thin superior flap produced with the inferior Lyacir Ribeiro's flap.

Figure 3. Detail of the great volume of the inferior flap, which will define 70% of the breast volume.
Using a 2-0 mononylon black thread, we subsequently proceeded to fix all lateral and superior edges of the inferior flap to the fascia of the pectoralis major muscle in a much higher position than the correspondent to the second rib. Each suture was carried out 1 cm apart, taking advantage of hardened tissues such as dermis and mammary glands when possible for its fixation. As a result, a rounded and hardened shape like that of a silicone implant was defined. In addition, 70% of the breast volume was provided by the inferior flap and 30% by the superior flap (Figure 4).
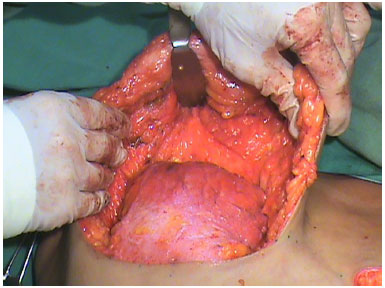
Figure 4. Inferior flap positioned showing the small volume of the superior flap, which will serve as a cover.
Subsequently, the inferior flap was covered with the superior flap, joining points B and C. The nipples were easily externalized due to the thickness of this flap. We then closed all incisions with sutures and applied occlusive dressing. Postoperatively, we recommended that the patients wear an enhanced bra for three months.
The patients were able to eat and walk without complaints after the surgery. Thus, they were discharged on that same day. The patients returned to perform the first dressing the day after and were guided on how to carry out daily dressings at home. They also returned three and eight days after the surgery when some sutures started to be removed, and on postoperative day fifteen to remove all remaining sutures. The patients returned 30, 60 and 90 days after the surgery, as well as after six months, to be photographed. If necessary, we consulted the patients in days aside from those scheduled.
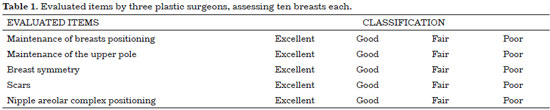
Three colleagues who are expert plastic surgeons with more than ten years of experience evaluated all patients using the photographic documentations of the pre- and postoperative period of six months. The response of the patients to a survey was also assessed (Table 1). A Kappa agreement analysis was carried out among the evaluators.
The presence of complications such as infection, poor quality scarring, necrosis, thrombosis and asymmetry was also observed.
RESULTS
The results of the evaluations carried out by the three plastic surgeons are shown in Tables 2 and 3 and Figures 5 and 7, while the pre- and post-operative period results are shown in Figures 8 to 16. The Kappa agreement analysis among the three evaluators showed a high concordance.
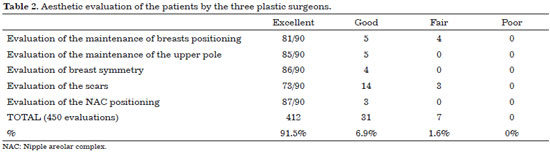
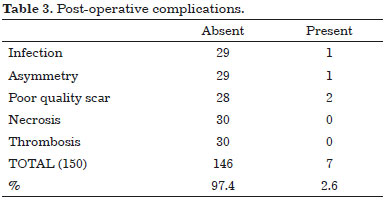
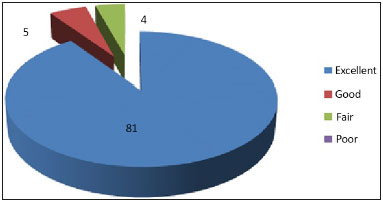
Figure 5. Evaluation graph of the maintenance of breast positioning by three plastic surgeons.
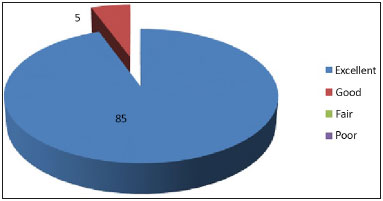
Figure 6. Evaluation graph of the maintenance of the superior pole by three plastic surgeons.
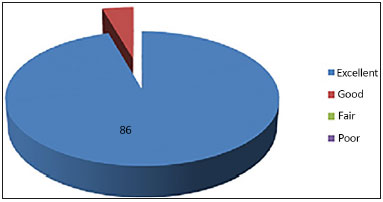
Figure 7. Evaluation graph of breast symmetry by three plastic surgeons.
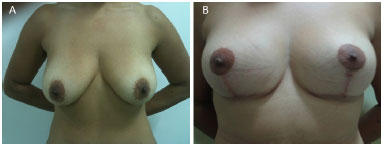
Figure 8. (A) pre and (B) post-operatory.
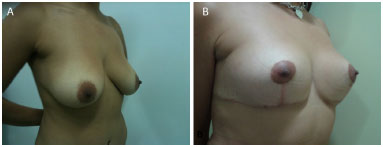
Figure 9. (A) pre and (B) post-operatory.
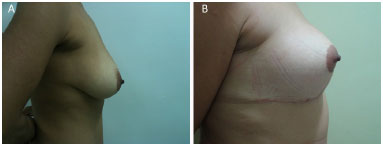
Figure 10. (A) pre and (B) post-operatory.
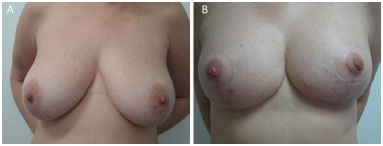
Figure 11. (A) pre and (B) post-operatory.
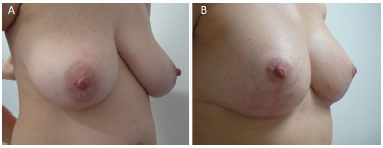
Figure 12. (A) pre and (B) post-operatory.
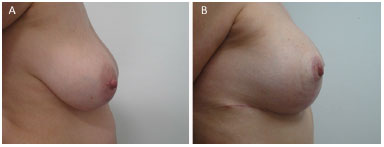
Figure 13. (A) pre and (B) post-operatory.
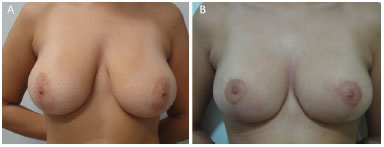
Figure 14. (A) pre and (B) post-operatory.
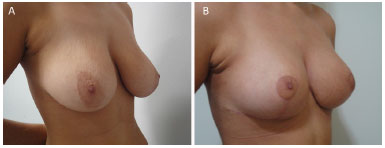
Figure 15. (A) pre and (B) post-operatory.
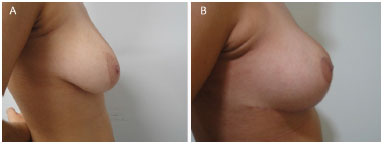
Figure 16. (A) pre and (B) post-operatory.
DISCUSSION
With the aim to seek a more rounded shape, with upper pole projection and harder texture, surgeons have often used silicone implants, which replace healthy tissues in procedures associated with mastopexy and breast reduction5.
The use of this treatment is increasing due to the pressure imposed by the patients themselves, who wish not only to obtain such result but also to use an implant. Although this leads to a satisfactory outcome, placing silicone implants in patients who do not aim to undergo breast augmentation generates a loss that must be considered. This refers to the presence of a foreign body, despite its low rate of morbidity.
The procedure described herein seeks to use a voluminous inferior flap fixed to the fascia of the pectoralis major muscle. This generated a rounded appearance and a firm texture, which mimicked the presence of a silicone implant without introducing a foreign body in the breast, while enabling to obtain the outcome desired (Table 2 and Figures 5 and 7).
The selection of the patients from our private clinic was at random. The females were selected also based on very similar profiles regarding social status and education. The inclusion, not inclusion and exclusion criteria followed common standards used in daily clinical practice.
To mark the external points of the skin resection, we used the inverted-T technique7. Any other technique leaving a final L-shaped or periareolar scar could have been used as long as a flap as previously described is produced. We used the Ribeiro's type IV inferior flap6, modifying only the residual volume of the superior flap, which measures around 2 cm thick. This served only to cover the inferior flap, leaving the latter to define the volume, form and texture of the breast when resections and fixations are carried out to achieve this aim6.
As demonstrated by the short-term percentages (Table 2 and Figures 5 to 7), the fixation of 70% of the breast volume (inferior flap) to a rigid structure (muscle fascia) is a very important factor to maintain breast positioning.
It is known that the modification of breast positioning is influenced by many factors including the elasticity of the tissue (quality of the skin), genetic and hormonal factors, previous pregnancy and diseases, age, loss or weight gain, breast parenchyma appearance, aspect of the capsule, level of postoperative activities and use of certain medications4. As shown in Figures 8 to 16, we can observe that the fixation maintains satisfactory breast positioning up to six months.
The evaluation carried out by the three expert plastic surgeons (evaluating ten patients each, 30 in total) revealed that 91.5% presented breasts with excellent quality and 6.9% with good quality. Only 1.6% of the patients presented a fair outcome, while poor results were not observed. Good and fair outcomes mostly referred to the aspect of the scars and not to the breast shape (Table 2 and Figures 5 to 7).
Most fair outcomes, referring to the quality of the scar, were easily resolved with outpatient procedures and treatments. With these findings, we believe that a very significant degree of satisfaction was obtained with this technique.
As involving the production of a thin superior flap, we could observe that this procedure was capable to increase the morbidity related to irrigation, leading to varying degree of pain and necrosis. However, as shown in Table 3, this was not observed due to the good irrigation of this flap by the branches of the internal (internal breast) and lateral thoracic arteries as well as anterior and lateral branches of the posterior intercostal arteries9,10.
In other procedures, they use the Pitanguy's technique, which is performed by resecting the gland as an inverted keel on the posterior face of the breast, keeping the internal and external breast pedicle. This allows very large resections, which results in an inverted-T scar. Minimum percentages of complications were observed including: areolar (1.2%) and skin (3.6%) damage, hematoma (0.5%) and unaesthetic scar (1.4%). These findings closely match those found in our study, although complications of hematoma and skin damage were not observed11.
McKissock12 recommends his technique when performing procedures for large hypertrophy associated with ptosis. It involves a vertical flap, which is superiorly and inferiorly bipedicled, and both medial and lateral resections. However, the vascular supply to the NAC is more parenchymal than sub-dermal, and ensured by inferior intercostal perforating branches.
His study included 184 patients with a total of 368 breasts, in which a total NAC necrosis was not observed. However, 1.4% of the patients presented a partial loss and 0.81% of them had skin necrosis. In our study, these changes were not evident due to the greater safety of our flap's irrigation. Further, he observed low incidences of lipolysis (1.62%), hematomas (2.1%), and primary infection (0.27%), which are very close to our result.
He also presented rates of scar hypertrophy affecting 65% of the patients, which leads us to believe that a poor arsenal of complementary treatment for this type of condition was present at the time of the study. Late bascule was also observed in 50% of the patients. These values are higher than those found when we used our technique, which we attribute to the time elapsed from the examination. In our case, it was only for six months12-14.
Thus, at the end of the examinations, this technique showed the ability to improve the upper pole projection of the breast depending on the positioning of the flap as observed in the operating room during the immediate postoperative period. This positioning was maintained up to six months with very high rates of satisfaction (97.4%) (Table 3 and Figures 8 to 16). By mimicking the use of silicone implants, the flap proved to be safe due to the low necrotic index (0%). Facilitating the migration of the nipple papillary complex according to the thickness of the flap, as in the technique proposed by Costa Lima14, the procedure used breast tissue, without the need to insert silicone implants. Further, this technique is very easy to learn since most of the steps used in this procedure are already carried out in our environment6,8.
CONCLUSION
The thin superior flap proved to be very effective in mammoplasties.
COLLABORATIONS
HC Data analysis and/or interpretation; statistical analysis; final approval of the manuscript; conception and study design; realization of the procedures and/or experiments; writing of the manuscript and/or critical reviewing of its content.
REFERENCES
1. Foged J. Symptomatology of breast hypertrophy. Ugeskr Laeger. 1953;115(12):439-51.
2. Sigurdson L, Mykhalovskiy E, Kirkland SA, Pallen A. Symptoms and related severity experienced by women with breast hypertrophy. Plast Reconstr Surg. 2007;119(2):481-6.
3. McKissock PK. Reduction mammoplasty and correction of ptosis of the breast. In: Grabb WC, Smith JW, eds. Plastic surgery. Boston: Little Brown; 1997. p.737-59.
4. Ferreira LM, Freire M, Garcia EB, Sabino Neto M. Mastoplastia redutora. In: Ferreira LM, Shor N, eds. Guia de medicina ambulatorial e hospitalar - UNIFESP - Cirurgia Plástica. São Paulo: Manole; 2007. p.545-51.
5. Saldanha OR, Maloof RG, Dutra RT, Luz OAL, Saldanha Filho O, Saldanha CB. Mamaplastia redutora com implante de silicone. Rev Bras Cir Plást. 2010;25(2):317-24.
6. Ribeiro L, Backer E. Mastoplastia con pediculo de seguridad. Rev Esp Cir Plast. 1973;6:223-34.
7. Pitanguy I. Mamoplastia: estudo de 245 casos consecutivos e apresentação de técnica pessoal. Rev Bras Cir. 1961;42:201-20.
8. Pitanguy I. Surgical treatment of breast hypertrofy. Br J Plast Surg. 1967;20(1):78-85.
9. Spear SL, Little JW. Reduction mammaplasty and mastopexy. In: Grabb W, Smith JW, eds. Plastic Surgery. 5th ed. Philadelphia: Lippincott-Raven; 1997.
10. Strömbeck JO. Mammaplasty. In: Grabb W, Smith JW, eds. Plastic surgery. 5th ed. Washington: Library of Congress; 1997. p. 726-8.
11. Pitanguy I. Evaluation of body contouring surgery today: a 30-year perspective. Plast Reconstr Surg. 2000;105(4):1499-514.
12. McKissock PK. Reduction mammaplasty with a vertical dermal flap. Plast Reconstr Surg. 1972;49(3):245-52.
13. Castro CC, Salema R, Aboudib Junior JHC, Calixto CA. Mamaplastia redutora na mulher jovem: análise crítica e evolutiva a longo prazo. J Bras Ginecol. 1986;96(9):471-3.
14. Rocha ACG, Costa CS, Campos H. Técnica de Costa Lima nas hipertrofias mamárias associada ao retalho de pedículo vascular inferior. Rev Bras Cir Plást. 2010;25(1):154-67.
Escola Bahiana de Medicina, Salvador, BA, Brazil
Institution: Clinica Nova Face, Salvador, BA, Brazil.
Corresponding author:
Humberto Campos
Rua Quintino de Carvalho, 113/701 - Jardim Apipema
Salvador, BA, Brazil Zip Code 40155-280
E-mail: hc@humbertocampos.med.br
Article received: February 18, 2016.
Article accepted: August 6, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter