ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Foot replantation in children: a case report
Reimplante de pé em criança: relato de caso
Case Report -
Year2014 -
Volume29 -
Issue
4
Marina Buainain Balbuena1; Kleder Gomes de Almeida2; Paulete Yuri Nukariya Gomes de Almeida3; Bruno Barros de Azevedo Coutinho4; Tatyanne Ferreira da Silva5; Fábio Tacla Saad6
http://www.dx.doi.org/10.5935/2177-1235.2014RBCP0102
ABSTRACT
INTRODUCTION: The indications for lower limb replantation in children are still controversial in the literature. Furthermore, they are more selective than those for upper limb replantation. Replantations of lower limbs are less frequent for various reasons, including that the traumas leading to amputations at the lower limb level are usually high-kinetic-energy injuries and involve severe tissue damage, in addition to their frequent association with other organ damage that discourage the use of the procedure. Because of the association with frequent serious postoperative complications and unsatisfactory outcomes in some cases, many surgeons feel discouraged to replant these segments. There are few literature reports on lower limb replantations with functional success.
CASE REPORT: Patient E.S.S. is a 4-year-old girl who was run over by a train in July 1997. The accident resulted in the crushing of the lower third of her left leg and the amputation of her left ankle. She was admitted to the emergency room of Santa Casa de Campo Grande-MS, in good overall condition. Replantation of the amputated limb was recommended. She was then transferred to the operating room, and her left foot was replanted after 8 h of ischemia.
CONCLUSION: Clearly, in selected cases, such as the patient reported here, microsurgical replantation is a valid and extremely valuable option, both from a functional and an aesthetic point of view.
Keywords:
Limb replantation; Microsurgery; Replantation in children.
RESUMO
INTRODUÇÃO: As indicações de reimplante de membros inferiores em crianças são ainda controversas na literatura e, comparadas com os reimplantes de membros superiores, são mais seletivas. Os reimplantes de membro inferior são menos frequentes por várias razões, haja vista que os traumas que provocam amputações ao nível do membro inferior geralmente são de alta energia cinética e provocam grave lesão tecidual, além da associação frequente de lesões de outros órgãos que contraindicam o procedimento. Associada à frequência de complicações graves no pós-operatório e os resultados medíocres de alguns casos, muitos cirurgiões se sentem desencorajados a reimplantar estes segmentos. Existem poucos relatos de reimplantes de membros inferiores com sucesso funcional na literatura.
Relato de caso: Paciente E.S.S., sexo feminino, quatro anos de idade, vítima de atropelamento por trem em julho de 1997, que resultou em esmagamento do terço inferior da perna esquerda e amputação ao nível do tornozelo esquerdo. A paciente deu entrada na emergência da Santa Casa de Campo Grande-MS, apresentando boas condições gerais, sendo indicado o reimplante do membro amputado. Foi então transferida à sala de operação (S.O), e após oito horas de isquemia foi reimplantado o pé esquerdo.
CONCLUSÃO: Fica claro que em casos selecionados, como o da paciente acima, o reimplante microcirúrgico é uma opção válida e extremamente valiosa, não só do ponto de vista funcional, mas estético.
Palavras-chave:
Reimplante de membros; Microcirurgia; Reimplante em crianças.
INTRODUCTION
The indications for lower limb replantation in children are still controversial in the literature. Furthermore, they are more selective than those for upper limb replantation. Replantations of lower limbs are less frequent for various reasons, including that the traumas leading to amputations at the lower limb level are usually high-kinetic-energy injuries and involve severe tissue damage, in addition to their frequent association with other organ damage that discourage the use of the procedure. Because of the association with frequent serious postoperative complications and unsatisfactory outcomes in some cases, many surgeons feel discouraged to replant these segments1-6.
There are few literature reports on replants of the lower limbs with functional success. Usui et al.3 reported the successful replantation of a leg on a 4-year-old patient who, after 4 years of surgery, showed an excellent functional outcome.
Morrison et al.4 state that lower-limb replantation is less suitable because of the poor quality of nerve regeneration and the quality of prosthesis in the lower limb.
The survival and success of the replant are dependent on several factors, including the duration of ischemia; associated lesions; appropriate surgical technique with debridement of the extremities, bone shortening, osteosynthesis, myotendinous repair, arteriovenous anastomoses, and microneurorraphy with or without grafts or the help of a magnifying glass, microscope, or appropriate microsurgical material; as well as the presence of a multidisciplinary team and relevant support in the intensive care unit1-6.
OBJECTIVE
The goal of replantation should be, primarily, to restore the function of the extremity, and, secondarily, to restore the limb's appearance. The foot's sensitivity is critical for providing proprioception and to prevent the formation of pressure ulcers.
CASE REPORT
Patient E.S.S. is a 4-year-old girl who was run over by a train in July 1997. The accident resulted in the crushing of the lower third of her left leg and the amputation of her left ankle (Figure 1), but with good retro foot conditions.

Figure 1. Left foot, amputated at the level of the ankle joint.
She was admitted to the emergency room of Santa Casa de Campo Grande-MS, in good overall condition. Replantation of the amputated limb was recommended. She was then transferred to the operating room, and, after 8h of ischemia, her left foot was replanted by using the following procedure:
1. Debridement of all devitalized tissues;
2. Individualization of all viable structures;
3. Bone shortening of about 8cm;
4. Tibial-tarsal arthrodesis;
5. Tenorrhaphy of the Achilles tendon and the flexor digitorum longus;
6. Tenorrhaphy of the extensor digitorum longus and extensor hallucis longus;
7. Arteriovenous microanastomosis of the anterior tibial and posterior tibial;
8. Microneurorraphy of the deep peroneal nerve and posterior tibia.
The patient developed perfusion of the amputated segment; however, she presented partial necrosis of the skin on the side of the leg (Figure 2), which was debrided and grafted with partial skin of the thigh on the 15th day after surgery. She was discharged after 22 days of hospitalization and followed at Plastic Surgery and Orthopedics clinic. Gradual improvement of the sensitivity of the plantar region was observed, and 8 months after the replantation, plantar sensitivity returned completely, except in the calcaneal region due to healing by secondary intention in this region at the time of fixation of the transdermal bone. After 3 months, she could extend the hallux, and by 6 months she was able to walk with the aid of an orthopedic boot. She remained under orthopedic care and was submitted in July 1999 to bone transport with limb lengthening by using the Ilizarov method (Figure 3), with a gain of about 3cm.

Figure 2. The replanted foot at the immediate postoperative period, demonstrating good perfusion.

Figure 3. Elongation of the limb by using the Ilizarov method.
She presented with a decrease in foot length due to a lesion in the tibial-tarsal bone growth site, compared with the contralateral foot. Moreover, the anterior-posterior muscles of the leg developed atrophy because of the lack of a suitable therapeutic follow-up. She was able to perform discrete flexion-extension of the fingers.
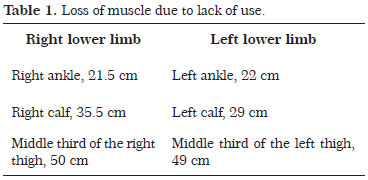
She currently presents atrophy on all muscles of the left lower limb (Figure 4), with loss of muscle due to lack of use (Table 1), and a shortening of about 3cm in relation to the contralateral limb.
DISCUSSION
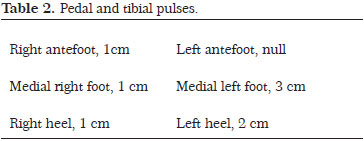
According to an arterial Doppler echo of the left leg, the patient presented patent distal arteries and two-phase flow (low resistance).
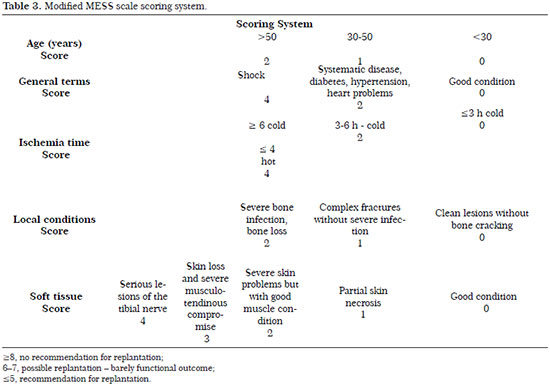
Very few reports have been published about successful foot replantations in children at the articular level. This procedure has few indications because of the severity of the trauma; the main criteria include age, overall condition, ischemia time, type and extent of tissue damage, and associated amputations. The modified Mangled Extremity Scoring System (MESS) scale (Table 3) can be used in emergency situations, to aid in the surgical decision to perform replantation. According to the scoring system, the present patient had 6 points in total. As she is young, she was in good general condition with good conservation of the segment; she received 4 points for ischemia duration, 1 point for the presence of complex fracture without serious infection, and 1 point for presenting partial skin necrosis.
Sensitivity was restored as expected but with a slight decrease in the calcaneal region due to scarring.
Priority was given to performing tenorrhaphy on the flexor and extensor musculature to maintain opponency and stabilization of the functioning joints.
Deep posterior tibial and peroneal microneurorraphy was performed to preserve the sensitivity of the first digital space and recover the driving force of the short extensor digitorum and plantar sensitivity, respectively.
Shortening was corrected through the use of a boot without compromising ambulation.
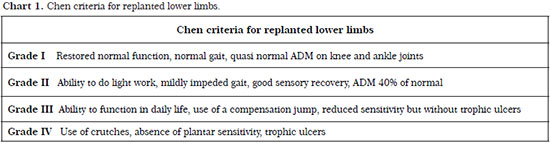
According to the Chen criteria (Chart 1) for replanted lower limbs, the patient, after 14 years of development, is in stage III because she can carry out light work and use a compensation jump, as well as presents sensitivity reduction but without pressure ulcers, demonstrating that the procedure performed had a good functional outcome.
CONCLUSION
Clearly, in selected cases, such as the patient in this report, microsurgical replantation is a valid and extremely valuable option, both from a functional and an aesthetic point of view.
This is important considering the psychosomatic traits of human beings that value the preservation of self-image together with the maintenance of physical integrity.
REFERENCES
1. Hoehn JG. Replantation of the foot. Surg Ronds. 1978;1:53-60.
2. Magee HR, Parker WR. Replantation of the foot: results of two years. Med J Aust. 1972;2:175-755.
3. Usui M, Minami M, Ishui S. The successful replantation of one amputated leg in a child. Plats Reconst Surg. 1979;63:611-613.
4. Morrison WA, O'Brien BM, MacLeod AM. Major limb replantation. Orthop Clin North Am. 1977 Apr;8(2):343-8.
5. Chen ZW, Chen LE. Lower limb replantation. In: Brunelli G (ed). Textbook of Microsurgery. Milan, Masson, 1988, p. 503-508.
6. Helfet DL, Towey T, Sanders R, Johansen K. Limb salvage versus amputation. Preliminary results of the Mangled Extremity Severity Score. Clin Orthop Relat Res. 1990;(256):80-6.
1. Aspirant Member of the Brazilian Plastic Surgery Society - Resident in Plastic Surgery
2. Member of the Brazilian Plastic Surgery Society - Plastic Surgeon
3. Specialist Member at the Brazilian Plastic Surgery Society - Plastic Surgery
4. Aspirant Member of the Brazilian Plastic Surgery Society - Resident in Plastic Surgery
5. Aspirant Member of the Brazilian Plastic Surgery Society - Resident in Plastic Surgery
6. Aspirant Member of the Brazilian Plastic Surgery Society - Resident in Plastic Surgery
Institution: Santa Casa de Campo Grande Mato Grosso do Sul.
Corresponding author:
Marina Buainain Balbuena
Rua Eduardo Santos Pereira, 88 - 2ºandar - Ala B, Setor de Queimados - Centro
Campo Grande, MS, Brazil Zip code: 79002-924
E-mail: mamedicina@yahoo.com.br
Article submitted: August 14, 2011.
Article accepted: February 24, 2012.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license