ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Lipoabdominoplasty. Systematization to minimize complications
Lipoabdominoplastia. Sistematização para minimizar complicações
ABSTRACT
INTRODUCTION: Abdominoplasty and liposuction are two of the most frequently performed plastic surgeries in Brazil. Many Brazilian plastic surgeons have contributed to their improvement and constantly seek the best result for their patients. Surgeons also must always be attentive to thromboembolic events that may have a tragic outcome.
METHODS: Twenty (20) female patients, aged 29 to 63 years, with a mean age of 43 years, underwent surgery. The patients attended a pre-anesthetic visit, where they were classified according to surgical risk using the American Society of Anesthesiologists classification, underwent routine testing, abdominal wall ultrasonography, cardiovascular assessment, and psychological assessment.
RESULTS: Among the 20 cases, there was one case of persistent seroma, one case of "dog-ear," and one case of umbilical wound dehiscence. The complications that occurred did not influence the final surgical outcome and 15 patients were very satisfied 6 months post-surgery.
CONCLUSION: Lipoabdominoplasty proved to be a safe technique with good results. Psychological factors must be assessed and a necessarily rigorous routine starting from the preoperative period allows a reduction in the risk of complications.
Keywords:
Lipoabdominoplasty; systematization; complications.
RESUMO
INTRODUÇÃO: A abdominoplastia e a lipoaspiração estão entre as cirurgias plásticas estéticas mais realizadas em nosso país, inúmeros cirurgiões plásticos brasileiros contribuíram para o seu aperfeiçoamento, sempre visando um melhor resultado ao paciente. Devemos sempre estar atentos aos fenômenos tromboembólicos que podem ter um desfecho dramático.
MÉTODOS: Foram operadas 20 pacientes, com idade variando de 29 a 63 anos, idade média de 43 anos, todas do sexo feminino. As pacientes passaram por consulta pré-anestésica, onde foram classificadas segundo o risco cirúrgico utilizando tabela da ASA (American Society of Anesthesiologists), realizaram os exames de rotina, Ultrassonografia de parede abdominal, avaliação cardiológica e avaliação psicológica.
RESULTADOS: Em nossa casuística de 20 pacientes, tivemos um caso de seroma persistente, um caso de "dog ear" e um caso de deiscência de cicatriz umbilical, as complicações encontradas não influenciaram o resultado final da cirurgia e 15 pacientes se disseram muito satisfeitos após 6 meses de operados.
CONCLUSÃO: A lipoabdominoplastia demonstrou ser uma técnica segura e que traz bons resultados ao paciente, aspectos psicológicos devem ser avaliados e uma rotina criteriosa desde o pré-operatório visa diminuir possíveis intercorrências.
Palavras-chave:
Lipoabdominoplastia; sistematização; complicações.
INTRODUCTION
Per a recent study by the Brazilian Society of Plastic Surgery and the International Society for Aesthetic Plastic Surgery, liposuction and abdominoplasty are the first and fourth most frequently performed plastic surgeries in Brazil1. For more than a century, since the study by Kelly2, many surgeons have acquired an interest in the technique and contributed towards its improvement. In Brazil, surgeons such as Callia3, Pitanguy4,5, Baroudi6, Hakme7, Avelar8,9 and Saldanha8, among others, have gained prominence with their contributions to better outcomes for patients while always maintaining the fundamental principles of the technique. These principles are transverse low abdominal incision, plication of the abdominal muscles, resection of the excess abdominal flap and umbilical transposition.
There is a perfect marriage between the contributions of Illouz10,11, who described liposuction in the 1980s, and surgery with selective detachment of the abdominal flap, described by Saldanha12, resulting in a more complete operation with fewer complications. Abdominoplasty is no longer the only solution to enhance abdominal contour, since liposuction can also be used. Through combined surgery, outcomes were more satisfactory to both the surgeon and the patients, whose demands increase each year. The reduction in flap detachment area and the preservation of abdominal perforating vessels gave rise to the era of lipoabdominoplasty (Saldanha et al., Avelar2,9,12) without necrosis of the large flap that was once observed. With preservation of the vascularization of most of the abdominal flap, lipoabdominoplasty became indicated for a large group of patients and problems such as seroma, epitheliosis, and skin necrosis, especially in smokers, significantly decreased, since skin detachment was reduced12,13,14.
The aim of this study is to demonstrate the authors' experience with systematization in lipoabdominoplasty, with particular attention to the prophylaxis of thromboembolic events (deep vein thrombosis and pulmonary embolism), which may have a tragic outcome15.
METHODS
Between January and July 2012, 20 female patients, aged 29 to 63 years old, with mean age of 43 years, underwent surgery. The patients attended a pre-anesthetic visit, where they were classified according to surgical risk using the American Society of Anesthesiologists (ASA) classification, underwent routine testing, abdominal wall ultrasonography, cardiovascular assessment, and psychological assessment.
The patient inclusion criteria were good overall health, normal preoperative exams, ASA surgical risk of 1 or 2 and a real expectation of surgical outcome. Patients who were smokers, had diabetes, or had hypertension or abdominal wall hernias were excluded from the study. All patients signed an informed consent form16 and underwent routine photographic documentation. The patients were requested not to take Ginkgo Biloba, anti-inflammatory drugs, paracetamol, aspirin, or oral contraceptives in the 10 days prior to the surgery.
Surgical technique
Surgical procedures were as follows
The patient was placed in the prone position and was placed under spinal anesthesia and sedation. The dorsal region and flanks were infiltrated with a solution of 0.9% saline + adrenaline in a ratio of 1:500,000. Liposuction of the dorsal region and flanks was performed. The patient was placed in the supine position. A 6-7cm mark for abdominoplasty was made above the vaginal fold. The supraumbilical abdominal region and flanks were infiltrated with a solution of 0.9% saline + adrenaline in a ratio of 1:500,000. The abdomen was detached by tunneling towards the xiphoid appendix. Strict hemostasis was applied. Muscular aponeurotic plication of the abdominal rectus was performed over the midline with 2-0nylon thread. Umbilical fixation was performed with four cardinal points using 4-0nylon thread. Infraumbilical flap resection (classic abdominoplasty) and two-plane fixation (subcutaneous and intradermal) were performed using 2-0nylon threads. The abdomen was marked for navel reconstruction using to the rectangular technique17. A vacuum drain was placed and fixed with 2-0nylon thread. Local dressing using nebacetin ointment, Dersani ointment, gauze, and microporation was applied. The surgical belt was placed. Liposuction was performed to remove 1000-4000 mL over 2.5-4h.
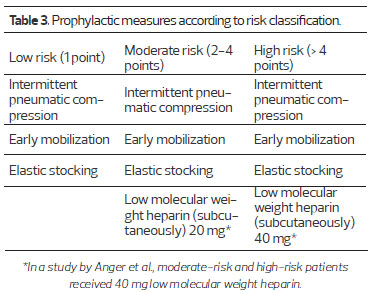
For deep vein thrombosis prophylaxis, all patients used compression stockings and a device providing a continuous and sequential massage. Drug-based prophylaxis was performed by subcutaneous injection of low molecular weight heparin 6 h post-surgery, using a dosage as determined by Table 3 15,19,20. Intravenous application of 2 g Keflin was used to prevent infections during anesthetic induction (Figure 1).
Walking was encouraged as soon as motion in the legs was possible. Patients stayed overnight at the hospital and were discharged the next morning as long as they had been able to eat and showed diuresis. An antibiotic, an anti-inflammatory, and an analgesic were prescribed for seven days.
During the post-operative course, the drain was removed and the dressing was replaced on day 3 post-operation. The patients were examined weekly until the end of the first month, at the end of the third month, and at the end of the sixth month. Photographs were taken one, three, and six months post-operation. Possible surgical complementation was assessed at the end of the sixth month, with consideration of the patients' complaints and photographic documentation.
RESULTS
From a total of 20 operated patients, the complications that occurred were one persistent seroma, where the patient was drained weekly for 4 weeks to resolve the symptoms, one case of "dog-ear" (skin redundancy around the scar), and one case of umbilical wound dehiscence, which resolved with local dressings in two weeks.
None of the complications mentioned above represented an impairment to the outcome of the surgery. The patient presenting with dog-ear underwent corrective operation with local anesthesia within 8 months. The patient with epidermolysis of the umbilical wound was the most obese patient and had the thickest adipose panniculus in our study. The patients' level of satisfaction at 6 months post-surgery was assessed through a simple questionnaire with the options "very satisfied," "satisfied," and "unsatisfied." Of the 20 patients, 15 were very satisfied and 5 were satisfied (Figures 2-10).

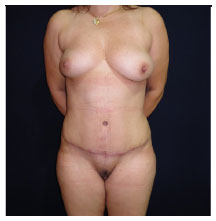
Figure 2. One month post-operation.
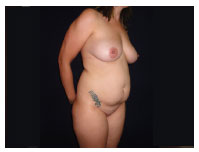
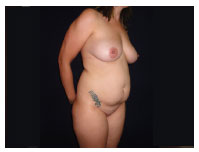
Figure 3. Before operation.
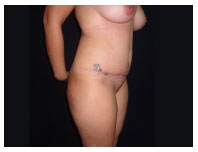
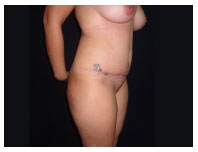
Figure 4. One month post-operation.

Figure 5. Before operation.

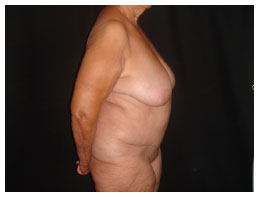
Figure 6. One month post-operation.

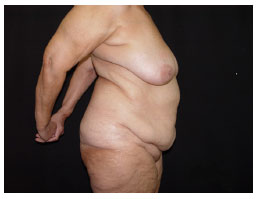
Figure 7. Before operation.
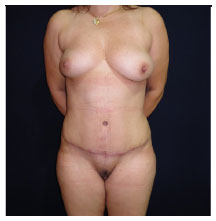
Figure 8. Three months post-operation.
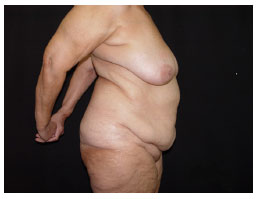
Figure 9. Before operation.
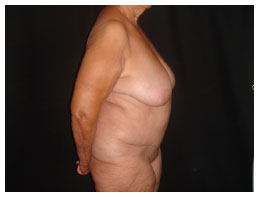
Figure 10. Six months post-operation.
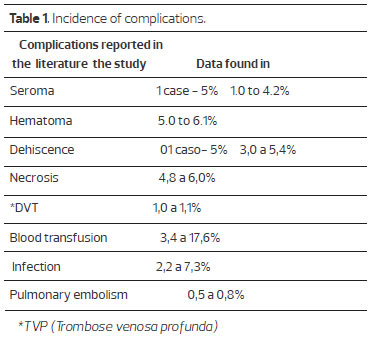
The number of complications was similar to that reported in the literature, and the inclusion criteria and sample certainly contributed to the absence of complications such as flap necrosis, hematoma, and deep vein thrombosis (DVT), as shown in Table 120,21.
DISCUSSION
Plastic surgery has always been very prominent in the media and the search for a perfect body, particularly in tropical countries like Brazil. Patients' demands increase every year, compounded by lawsuits against plastic surgeons. In a study conducted by the Regional Council of Medicine of the State of São Paulo between 2000 and 2006, plastic surgery was the most frequently sued medical specialty22,23.
Women represent the vast majority of plastic surgery patients 24 and, due to their active social lives, demand fast recovery, which requires a less traumatic operation with better outcomes than the ones achieved in previous decades. This complicates the job of the surgeon.
Every surgery carries the risk of complications and it is the physician's task to request preoperative tests and perform a proper assessment of the patient. Outcome success begins with a well-performed evaluation. Abdominoplasty significantly contributes towards a better silhouette, but is impossible to perform in regions with localized fat such as the flanks and back. By combining liposuction, a more harmonious result is achieved.
The studies performed by Saldanha et al., with a selective abdominal flap detachment to preserve vascularization on its side, have significantly contributed to a reduction in flap complications and have enabled concomitant liposuction. This was very evident in a study using Doppler12,26.
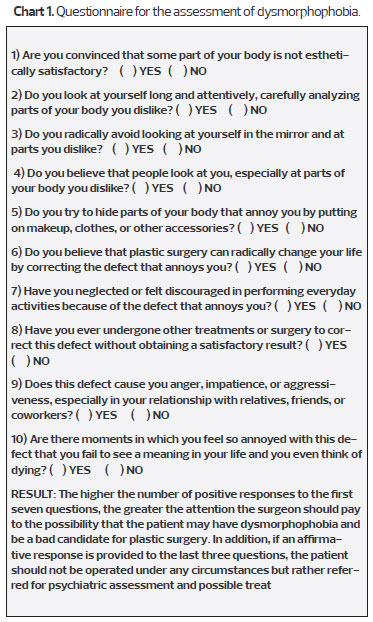
During preoperative psychological assessment, the patient is examined for dysmorphophobia (body dysmorphic disorder). Patients with this disorder are never pleased with the result, which may affect the doctor-patient relationship. Here, we used the Pisa scale modified by D'Assumpção26 (Chart 1).
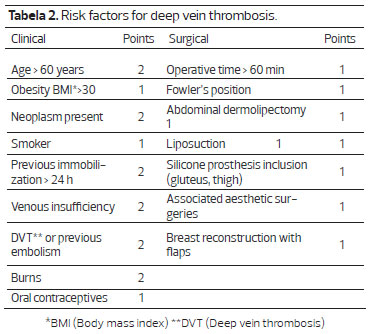
The high morbimortality of DVT and pulmonary embolism justify our concern with this topic. We performed mechanical and drug-based prophylaxis following a score table used in a study by Anger et al., which classifies patients as being at low-risk, moderate-risk, and high-risk for thromboembolic phenomena18, as shown in Tables 2 and 3. Lipoabdominoplasty, due to its operative time and patient's position post-operation, classifies the patient at least as medium-risk. As shown in Virchow's triad (endothelial injury, hypercoagulability status and stasis of blood flow), patients undergoing this type of surgery present all the factors necessary for the development of thromboembolic problems.
CONCLUSION
Lipoabdominoplasty has been shown to be a safe surgical technique that provides good results to patients. Surgeons should always be attentive to the possibility that thromboembolic phenomena may occur and take preventative action through mechanical and drug-based prophylaxis.
The psychological factors, which can cause future complaints and affect the doctor-patient relationship, should also not be ignored.
A rigorous assessment must be performed from the preoperative period to medical discharge to minimize any complications that might occur.
REFERENCES
1. Pesquisa publicada no site da Sociedade Brasileira de Cirurgia Plástica.www.cirurgiaplastica.org.br(http://www2.cirurgiaplastica.org.br/wp-content/uploads/2012/11/sbcp_isaps.pdf)
2. Kelly HA. Excision of the flat abdominal wall lipectomy. Surg Gynec Obstet. 1910;10:229.
3. Callia W. Dermolipectomia abdominal. São Paulo: Carlos Erba, 1963.
4. Pitanguy I, Gontijo de Amorim NF, Radwanski HN. Contour surgery in the patient with great weight loss. Aesth Plast Surg. 2000;24(6):406-11.
5. Pitanguy I. Abdominoplaty: Classification and surgical techniques. Rev Bras Cir. 1995;85:23 44.
6. Baroudi R, Ferreira CAA. Seroma, how to avoid it and how to treat it. Aesth Surg J. 1988;18:439.
7. Hakme F. Technical details in the lipoaspiration associate with liposuction. Rev. Bras. Cir. 1985;75(5):331-7
8. Avelar JM. Surgical anatomy and distribution of the subcutaneous fat tissue on Human Body. In: Avelar JM, Illous YG (ada.). Lipoaspiração. São Paulo: Ed.Hipócrates, 1986:45-57.
9. Avelar JM. Abdominoplasty: A new technique without underminig and fat layer removal. Arquivo Catarinense de medicina. 2000;29:147-9.
10. Illouz YG. Study of subcutaneous fat. Aesth Plast Surg. 1990;14(3):165-77.
11. Illouz YG. A new safe and aesthetic approach to suction abdominoplasty Aesth Plast Surg. 1992;16(3):237-45.
12. Saldanha O. Lipoabdominoplastia-Técnica Saldanha. Rev. Soc. Bras. Cir. Plast. 2003;lS(1):37-46.
13. Avelar JM. Uma nova técnica de abdominoplastia: sistema vascular fechado de retalho subdérmico dobrado sobre si mesmo, combinado com lipoaspiração. Rev Bras Cirurg. 1999;27(3):3-20.
14. Saldanha OR, Souza Pinto EB, Mattos Jr. WN, Pazetti CE, Lopes Bello EM, Rojas Y et al. Lipoabdominoplasty with selective and safe undermining. Aesthetic Plast Surg. 2003;27(4):322-7.
15. Wisniesky, Costa V, Fortaleza J.B. Tromboprofilaxia em cirurgia plástica. Rev. Bras. Cir. Plást. 2010;25(supl):1-102.
16. Ferraz EM. Complicação ou erro médico? Rev Col Bras Cir. 2006;33(4):205-6.
17. Garbero R, Vieira A. Fármacos no pré-operatório. Rev Hosp Universitário Pedro Ernesto, UERJ. 2007:28-37.
18. Luis López-Tallaj. Restauração Urnbilical na Abdorninoplastia: Urna Simples Técnica Retangular. Rev Soc Bras Cir Plast. 2001;16(3)39-46.
19. Anger, Baruzzi A.C.A., Knobel E. Um protocol de prevenção de trombose venosa profunda em cirurgia plástica.Rev. Soc. Bras. Cir. Plast. 2003;(I8)47-54.
20. De Paiva A. et al. Tromboembolismo venoso em cirurgia plástica:protocolo de prevenção na Clínica Ivo Pitanguy. Rev. Bras. Cir. Plást. 2010;25(4):583-8.
21. Almeida EG, et al. Abdominoplastia:Estudo retrospectivo. Rev. Soc. Bras. Cir. Plást. 2008;23(1):1-10.
22. Jatene PRS, et al. Abdominoplastia: Experiência clínica, complicações e revisão da literatura. Rev. Soc. Bras. Cir. Plást. 2005;20(2):65-71.
23. Conselho Regional de Medicina do Estado de São Paulo (CREMESP) 9 de outubro de 2007. Denúncias e processos relacionados ao exercício profissional da medicina no Estado de São Paulo no período de 2000 a 2006.
24. Seugling , et al. Distribuição dos processos disciplinares pelo CREMESP - Conselho Regional de Medicina do Estado de São Paulo e seus resultados nas diversas especialidades médicas. Centro Universitário São Camilo. 2007;1(2):56-62.
25. Pesquisa Datafolha-Instituto de pesquisa. Publicada no site da Sociedade Brasileira de Cirurgia Plática. www.cirurgiaplastica.org.br (http://www2.cirurgiaplastica.org.br/wpcontent/uploads/2012/11/pesquisa2009.pdf)
26. Graf R, Araujo LR, Rippel R, Neto LG, Pace DT, Cruz GA. Lipoabdominoplasty: liposuction with reduced undermining and traditional abdominal skin flap resection. Aesthetic Plast Surg. 2006;30(1):1-8.
27. D'Assumpção EA. Dismorfofobia ou complexo de Quasímodo. Rev. Soc. Bras. Cir. Plást. 2007;22(3):183-7.
1-Medical Specialist - Top Clínica-Frutal Plastic Surgery Clinic
2-Medical Specialist - Top Clínica-Frutal Plastic Surgery Clinic
Institution: Study performed at the Top Clínica-Frutal Plastic Surgery clinic, Minas Gerais, Brazil.
Corresponding author:
Carlos Gustavo Zahluth Monteiro
Rua das Margaridas 89
Frutal-Minas Gerais
Telefone 034-3421-4845
E-mail: drgustavoplastico@hotmail.com
Article received: November 19, 2013
Article accepted: December 8, 2013
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license