

Original Article - Year 2014 - Volume 29 -
Predictive factors for complications in plastic surgery procedures - suggested safety scores
Fatores preditivos de complicações em procedimentos da cirurgia plástica - sugestão de escore de segurança
ABSTRACT
INTRODUCTION: This study analyzed the association between plastic surgery complications and risk factors in the study population, and presents a safety scale for planning plastic surgery procedures.
METHODS: A case-control study was performed, including patients who underwent procedures at various plastic surgery centers from 2010-2011 and who had some type of postoperative complication. The control group consisted of patients who underwent similar procedures during the same period without complications. Descriptive analysis was performed using absolute and relative frequency and measures of central tendency (mean and median) and dispersion (standard deviation and minimum and maximum value). Associations were analyzed using the chi-squared test of association and univariate and multiple logistic models. In all analyses, statistical significance was defined as p-values <0.05.
RESULTS: A total of 168 patients were analyzed: 75 cases with complications (Group I, 44.64%) and 93 controls (Group II). There was a statistically significant association between the presence of a complication and two variables: undergoing an associated procedure (p = 0.049) and surgery duration greater than 240 minutes (p = 0.049).
CONCLUSION: The literature shows multifactorial risks for plastic surgery procedures. Proper patient selection, preoperative planning, and intra- and postoperative prophylactic care have contributed to decreased incidence of serious complications. The main risk factors associated with post-surgical complications were surgery durations longer than 4 hours and associated procedures.
Keywords: Safety in Plastic Surgery; Safety Score in Plastic Surgery; Predictive Safety Factors in Plastic Surgery.
RESUMO
INTRODUÇÃO: O objetivo deste estudo foi analisar, em nosso meio, a associação entre a ocorrência de complicações em procedimentos de cirurgia plástica e os fatores de risco presentes nessa população, e apresentar uma Escala de Segurança para planejamento do ato cirúrgico em Cirurgia Plástica.
MÉTODOS: Estudo do tipo caso-controle, com pacientes submetidos à cirurgia plástica no período de 2010-2011, em vários centros de cirurgia plástica e que apresentaram algum tipo de complicação pós-operatória. Os controles foram pacientes submetidos a procedimentos semelhantes de cirurgia plástica no mesmo período, e que não tiveram complicações. Foi realizada análise descritiva por meio de frequências absoluta e relativa e medidas de tendência central (média e mediana) e dispersão (desvio padrão e valores mínimo e máximo). A análise da associação foi realizada pelo Teste da Associação pelo x2 e modelos de regressão logística univariada e múltipla. Em todas as análises foi considerado estatisticamente significativo quando p<0,05.
RESULTADOS: Foram analisados 168 pacientes, sendo 75 casos com complicações (Grupo I, 44,64%) e 93 controles (Grupo II). Houve associação estatisticamente significativa entre a presença de complicação com duas variáveis, ter realizado procedimento associado (p=0,049), e o tempo de cirurgia maior que 240 minutos (p=0,049).
CONCLUSÃO: A literatura demonstra aspectos multifatoriais de risco nos procedimentos da cirurgia plástica. A seleção adequada do paciente, o planejamento pré-operatório e os cuidados profiláticos no trans e pós-operatório têm contribuído para diminuição de incidência de complicações graves. Os principais fatores de risco relacionados a complicações no pós-operatório foram tempo cirúrgico maior que 4 horas e associação cirúrgica.
Palavras-chave: Segurança em Cirurgia Plástica; Escore de Segurança em Cirurgia Plástica; Fatores Preditivos de Segurança em Cirurgia Plástica.
The demand for cosmetic plastic surgery has been increasing steadily, mainly due to new surgical techniques and greater social acceptance. The most common procedures include breast surgery (augmentation or reduction), liposuction, abdominoplasty, and facial surgeries1-3.
Cosmetic plastic surgery has historically been considered safe2-6, but as with any surgery, there are risks7-9. Therefore, plastic surgeons should evaluate patients by following the same rigorous standards adopted for other surgeries, including detailed preoperative evaluation, physical examination, and laboratory tests in addition to intraoperative and immediate postoperative monitoring to ensure patient safety. It is important to collect data on drug use, smoking, and alcohol consumption, and to provide preoperative guidelines10,11. Preoperative evaluation is key for safe surgical procedures; it starts with thorough anatomical and physiological knowledge and choosing an appropriate surgical technique12.
Respiratory problems and bacterial infections are frequently described in plastic surgery procedures in general. Analysis of predictors of complications requires attention to multiple aspects, which complicates analysis in studies on this topic4,5,9. There is much controversy among various authors and studies.
The literature reports that plastic surgery performed in accredited surgical facilities, even those not located in hospitals, results in much lower incidence of complications5.
Byrd et al.2 reviewed medical charts of more than 5,000 plastic surgeries performed between 1995 and 2000 in Texas, USA, including procedures such as rhytidectomy, blepharoplasty, breast surgery (augmentation and reduction), rhinoplasty, otoplasty, abdominoplasty, and liposuction. They concluded that procedures performed in office-based facilities (outpatient, day clinics, or clinics) are safe, with a 0.7% rate of complications due to plastic surgery, provided appropriate care was taken in relation to anesthesia. The most frequent complications were hematoma (27 cases) and infection (6 cases).
However, according to Iverson and the American Society of Plastic Surgeons (ASPS)4, physiological stress related to surgical procedures is a safety factor that must be considered when choosing the most appropriate location for surgical procedures. The main factors for physiological stress are those caused by blood loss during surgery, hypothermia, liposuction in combination with other procedures, procedure duration, and risk of thrombosis or pulmonary embolism4.
Significant blood loss during surgery can lead to clinical instability during the postoperative period as well as unplanned rehospitalization4. It is recommended that patients be reassessed within 24 hours after discharge4,5.
Both local and general anesthesia adversely affect regulation of body temperature. Hypothermia is a concern for infection and anesthetic safety4. The guidelines from the American Classification Society of Anesthesiologists (ASA)13 are recommended for evaluation of surgical anesthesia risk. Anesthesiologists should classify patients based on clinical examination and presence of comorbidities. Higher classification values are associated with increased risk13.
Combined procedures have become increasingly common in plastic surgery, mainly due to reduced financial cost compared to individual surgeries as well as a single postoperative recovery phase2,4,5. Some authors have reported a cumulative effect of multiple procedures performed in a single operation, resulting in increased likelihood of complications14,15. Nevertheless, many plastic surgery procedures are routinely and safely combined in various clinical settings4,5.
Some combinations are more controversial, especially procedures such as liposuction and abdominoplasty16,17. The Lipoplasty Task Force has emphasized that performing multiple procedures is a major risk factor for complications as a result of liposuction4. Another study conducted in the United States by the American Society for Aesthetic Plastic Surgery (ASAPS) sent questionnaires to its members to evaluate liposuction morbidity and mortality in more than 94,000 procedures, and also noted increased risks when other procedures were performed at the same time, especially the combination of liposuction and abdominoplasty17. By contrast, various authors have reported that abdominoplasty and liposuction can be performed during the same lipoabdominoplasty procedure with selective detachment without increased complications, with improved aesthetic results and body contouring18.
Byrd et al.2, and Stevens et al.19, did not attribute adverse results to surgery with multiple procedures, since the frequency of complications was similar to rates for individual surgical procedures. Similarly, Matarasso et al.18, found no increased risk of local and systemic complications even in combined abdominal plastic surgeries such as abdominoplasties and liposuction. In the same study, participating physicians were asked which surgical procedures they would perform concurrently with full abdominoplasty; the most cited were thigh liposuction (83%), breast reduction (64%), blepharoplasty (64%), and rhinoplasty (40%).
One of the most critical attributes to consider in relation to patient safety is the time variable, including surgery duration and average length of stay in post-anesthetic recovery (Duarte and Ferreira20). Most plastic surgeries take over an hour to complete. Moreover, when more than one procedure is performed during the same operative period, the total surgery duration increases2.
A study in the 70s (Howland and Schweiser14) first pointed out that surgeries lasting more than 6 hours are associated with a dramatic increase in the incidence of post-surgical heart, kidney, and lung complications. This cutoff point was adopted by other researchers (Forgaty et al., Iverson15).
Another study carried out in Ireland by Norte15 compared three categories of reconstructive plastic surgery that usually last more than 6 hours: head and neck, breast reconstruction, and surgery of the upper and lower limbs, to verify if the surgery duration or type of surgery were related to postoperative complications. The researchers concluded that the duration of surgery was not a factor in postoperative morbidity, but the type of surgery and the patients' general health were.
Thrombosis and pulmonary embolism have a very low incidence, but cause significant harm. Matarasso et al.18 analyzed the incidence of complications of abdominal plastic surgery in more than 20,000 procedures and observed thrombosis and pulmonary embolism in 0.04% and 0.02% of procedures, respectively.
Several known factors predispose patients to these complications, including genetic or acquired factors such as antiphospholipid syndrome, homocysteine levels, and use of contraceptives and hormone replacement, among others4.
In addition to the general risks described by Iverson and the American Society of Plastic Surgeons (ASPS) in 20024, specific procedures are also associated with increased risks for complications. For example, another risk factor for complications following liposuction is excessive fat removal. According to the ASPS Committee on Patient Safety, removal of more than 5 liters is considered excessive4. More than half of the physicians (54%) in a study by Horton et al.5 reported removing up to 2.5 liters of fat and 5 liters or more in 5.4% of patients undergoing liposuctions. The authors concluded that this important data indicate that doctors are acting in accordance with plastic surgery safety standards.
Another study of post-liposuction complications conducted in Germany noted that bacterial infection was the most frequent complication, and that poor hygiene, high postoperative discharge, and selection of patients unfit for the surgery were the main risk factors for serious complications16.
Local complications after abdominal plastic surgery include hematoma, infection, seroma, and abdominal perforation, as well as pain, nausea, and vomiting16. In another study, the main complications were irregular abdominal contour (5.0%), skin necrosis with spontaneous healing (4.9%), need for scar revision (4.4%), or a second surgery (3.5%)16.
The most frequently diagnosed breast implant complications include capsular contracture, asymmetry, infection, and hematoma5. In a study conducted in the United Kingdom7, the most common complication was hematoma (1.5%), followed by infection (1.1%), and asymmetry (0.8%). Capsular contracture occurred in only 0.5% of 3,002 patients in this study of cumulative risk five years post-surgery. Finally, smoking is another factor consistently associated with complications. The prevalence of pulmonary, cardiovascular, and cerebrovascular complications during and after surgery is significantly higher among smokers. Finally, among risk factors related to patient history, diabetes and hypertension have been reported to be predictors of complications4.
Based on these findings, it appears that the major risk factors of post-surgery complications of plastic surgery are well known, and have resulted in several recommendations to improve patient safety. However, most articles on this subject are mainly theoretical. Postoperative complications are distressing for both the patient and the physician, and, due to the increasing number of plastic surgeries, they are becoming more frequent and deserve a more detailed study and practical application22. The development of a predictive score for plastic surgery complications would help surgeons to define preventive measures, allowing better choices and better discussion of risks with the patient during the preoperative period.
The objective of this study was to analyze the association between plastic surgery complications and risk factors in Brazil, and to develop a safety scale for planning plastic surgery procedures.
METHODS
Study design and samples
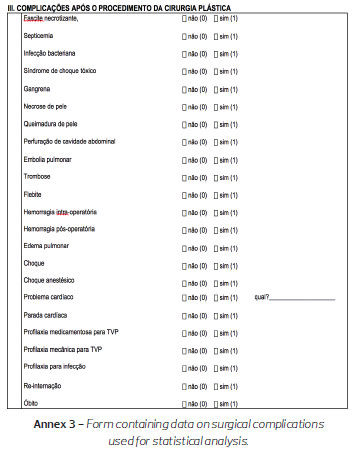
This case-control study included patients who underwent plastic surgery procedures from 2010 to 2012 in various medical centers in Brazil and who had some type of postoperative complication, namely: necrotizing fasciitis, septicemia, bacterial infection, toxic shock syndrome, gangrene, skin necrosis, cavitary perforation, pulmonary embolism, thrombosis, phlebitis, hemorrhage, hyperhydration (pulmonary edema), hypo-hydration (shock, epilepsy) shock due to anesthesia, heart problems, rehospitalization, cardiac arrest, or death.
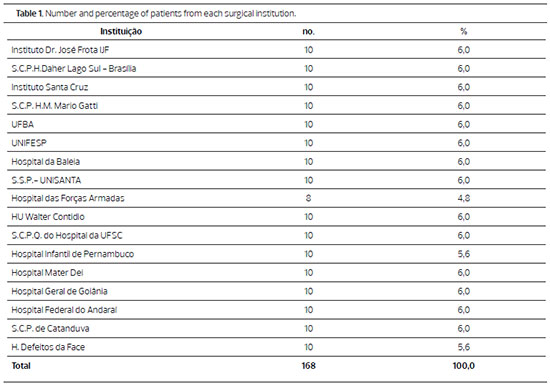
Control subjects in this study were patients who underwent similar plastic surgery procedures during the same period who had none of the complications mentioned above. The list of institutions that sent patient data is shown in Table 1. Surgical cases performed under local anesthesia lasting less than 30 minutes were excluded.
Methodology
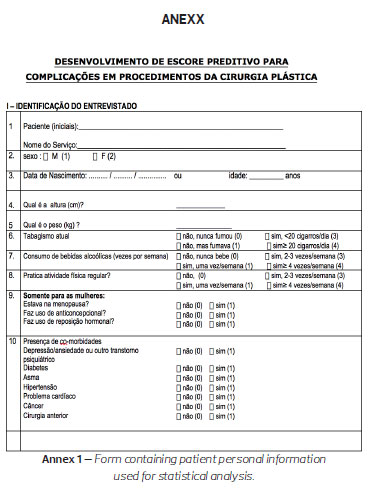
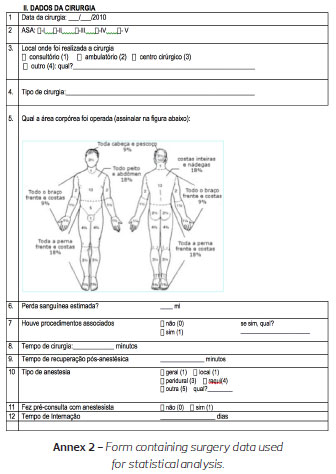
We distributed the form shown in Annexes (1, 2 and 3) to Accredited Services institutions in the Brazilian Society of Plastic Surgery (Sociedade Brasileira de Cirurgia Plástica, SBCP) and requested referral of 10 patients' data: five cases with complications (Group I) and five control cases (Group II). This form was developed based on Horton et al7.
Study variables
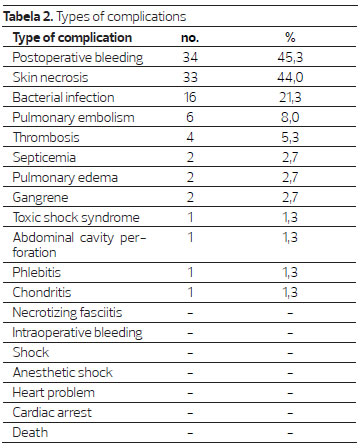
1. Dependent variablesThe analyzed variables are shown in Tables 2-4.
2. Presence of complications: yes or no
3. Independent variables
Statistical analysis
First, a descriptive analysis using absolute and relative frequencies and measures of central tendency (mean and median) and dispersion (standard deviation and minimum and maximum values) was made.
In association analysis, the dependent variable was the presence of complications (case = yes vs. control = no) and the independent variables. Associations were analyzed using chi-squared test of association and univariate and multiple logistic models. For the multiple logistic model, independent variables with p-values <0.20 in the chi-squared test of association should have been used, but among the variables with this p-value, the multiple model was impossible to perform; therefore, only the values of the odds ratio (OR) per point and the 95% confidence intervals were calculated.
In all analyses, statistical significance was defined as p < 0.05.
RESULTS
A total of 168 patients were analyzed: 75 cases with complications (Group I, 44.64%) and 93 controls (Group II).
Sample characterization
Women accounted for 82.1% of the study population. Patient ages ranged from 2 to 82 years, with a mean of 39.0 years (SD = 15.3 years) and a median of 37.5 years. Most patients were non-smoking (72.6%), non-alcohol drinkers (58.3%), non-practitioners of regular physical activity (62.5%), and eutrophic (57.7%). Of 139 female patients, 23.0% were in the postmenopausal period, 23.0% used contraceptives, and 7.9% used hormone replacement.
Few patients had comorbidities; the most frequent were cancer (13.1%), depression (11.9%), and hypertension (11.9%). Of 168 patients, 44.6% reported having undergone an associated surgery.
Most patients were classified as ASA I (70.8%) or ASA II (23.8%) (Table 2). Abdominal plastic surgery (23.3%), and mammoplasty (13.1%) were the most common procedures. Most patients underwent only one procedure; an associated procedure was performed in 14.9% of patients. The operated body area ranged from 1% to 40%, with an average of 10.5% (standard deviation = 7.9%) and median 10.0%. General anesthesia was most common (72.5%), but 41.1% did not undergo anesthetist pre-consultation. Drug and mechanical prophylaxis for deep vein thrombosis (DVT) was performed in 16.7% and 51.7% of patients, respectively. Blood loss ranged 1-1000 mL, with a mean of 149.0 mL (SD = 127.8mL) and median of 110.0 mL; 97.6% of patients lost less than 500mL of blood. Surgery duration ranged from 20 to 720 minutes, with an average of 178.9 minutes (SD = 91.8 minutes) and median of 180.0 minutes; 72.0% of patients had a surgery duration of less than 240 minutes (4hours). The post-anesthesia recovery time varied from 0 to 1,530 minutes, with an average of 91.8 minutes (SD = 131.9 minutes) and median of 60 minutes; 51.2% had a post-anesthesia recovery time of less than 60 minutes. The length of stay ranged from 0 to 60 days with an average of 3.2 days (SD = 6.8 days), median of 1.0 days, and 73.8% of patients stayed in the hospital no more than two days.
There were no statistically significant differences in variables between the two groups.
Characterization of complications
Among patients with complications 38.7% had more than one problem.
Table 2 shows complications in Group I. Post-operative bleeding (45.3%) was most frequent, followed by skin necrosis (44.0%), and bacterial infection (21.3%). No patients died.
Analysis of the association between complications and other variables
There were no statistically significant associations with any other variables, including gender (p=0.874), age (p = 0.687), current smoker status (p=0.482), alcohol consumption (p=0.490), regular physical activity (p=0.789), nutritional status (p=0.544), menopause (p=0.985), contraceptive use (p=0.424), and use of hormone replacement therapy (p=0.921). Although not statistically significant, the high percentage of complications among malnourished patients stood out (75.0%), but this category could not be analyzed separately owing to the small number of patients in this category (of 4 malnourished patients, 3 had complications).
There was no statistically significant association between the presence of complications and comorbidities such as depression (p=0.278), diabetes (p=0.290), asthma (p=0.442), hypertension (p=0.256), heart problems (p= 0.866), cancer (p=0.448), and previous surgery (p=0.833).
There was also no statistically significant association with ASA classification (p=0.321), location where surgery was performed (p=0.581), type of surgery (p=0.405), percentage of operated body area (p=0.947), body location (p=0.360), type of anesthesia (p=0.651), anesthetist pre-consultation (p=0.123), drug prophylaxis for DVT (p=0.548), mechanical prophylaxis for DVT (p=0.825), and blood loss (p=0.113). Only 2 patients in this study lost more than 500mL of blood and both had complications. One of these patients had 500mL of blood loss and a surgery duration of 240 minutes. The other had 1,000mL blood loss and a surgery duration of 480 minutes.
There was a statistically significant association between the presence of a complication and two variables: having completed an associated procedure (p=0.049), and surgery duration greater than 240 minutes (p=0.049). However, the number of patients with associated procedures or surgery duration greater than 240 minutes was very low, making conclusive statistical analysis impossible.
DISCUSSION
The increasing number of plastic surgery procedures also increases the frequency of complications, as has been reported in the literature. Patient safety is arguably one of the most discussed topics at scientific meetings and in medical publications, particularly those focused on plastic surgery. Assuring patient safety requires preventing complications22.
Despite the fact that cosmetic plastic surgery procedures are generally considered safe2, there are inherent risks, as with any surgery, especially when professional conduct is lacking5,23. This suggests the importance of rigorous patient evaluation during preoperative evaluation, as well as physical and laboratory tests beyond standard intraoperative and immediate postoperative monitoring.
Although surgery duration (procedures lasting more than 6 hours) was identified as a statistically significant and major factor for complications, there is a consensus that multiple risk factors contribute to more serious complications, especially the type of surgery and the overall health of the patient22. Prophylactic measures for preventing thrombosis and pulmonary embolism should be considered in these cases4,5.
There is also consensus that the sum of multiple risk factors may precipitate and establish complications. This is why there is interest in case-control studies to better estimate the occurrence of post-plastic surgery complications in Brazil.
In this case-control study, a form was sent to 17 Accredited Services institutions in the SBCP: cases were plastic surgery complications for procedures performed during 2010-2013, and controls were patients who operated on in the same time period who did not have complications. Statistical analysis was performed using logistic regression to estimate the probability of each of the complications from the form and their relationship with independent variables, including gender, age, nutritional status, smoking, alcohol consumption, physical activity, contraceptive use, hormone replacement therapy, presence of previous surgery, ASA classification, presence of comorbidities, and surgery data, such as location where the surgery was performed, type of surgery, part of the body that was manipulated, blood loss during surgery, other associated procedures, surgery duration, post-anesthesia recovery time, type of anesthesia, and anesthetist pre-consultation.
We found that the most frequent complications in this study population were hemorrhage (34%), skin necrosis (33%), and infection (16%), followed by pulmonary embolism (6%) and thrombosis (4%), similar to findings by Byrd et al, with a prevalence of hematoma and infection.
Unfortunately, the sample size was not sufficient for further conclusions or associations between complications and risk factors present in patients in each subgroup of complications.
Similar to previous studies, the predictive factors for complications that showed statistical significance in this study were: a) malnourishment; b) associated procedures; c) surgery duration.
Patients with low BMI had a high rate of complications (75%), but the number of patients in this category was low (n = 4); proper statistical analysis for more in-depth conclusions was therefore not possible.
Similarly, the low number of patients with associated procedures prevented proper analysis of this factor.
The greatest surgical duration (more than 4 hours) proved to be the major risk factor related to the occurrence of complications in this study. Longer duration is related indirectly to several factors recognized in the literature as associated with higher risk of complications: longer-lasting hypothermia, increased use of coagulation factors, higher-volume bleeding, and associated procedures.
This analysis, including all complications, and all classic risk factors, presents an overview of the current safety situation after plastic surgery in accredited services institutions of the SBCP. However, in future analysis, specific studies for each complication or risk factor should be performed. It should be noted that no specific prior risk factor could be detected in many of the complications observed, highlighting the fact that safety and prevention measures should be observed for every patient undergoing surgical procedures.
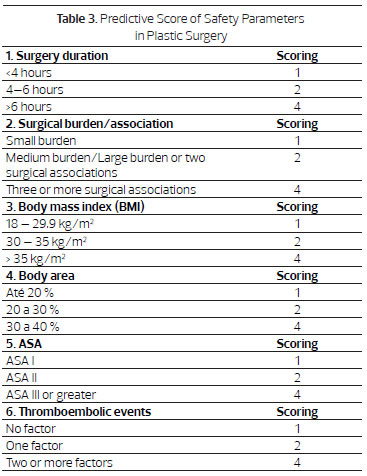
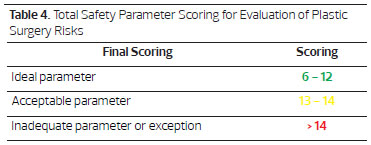
Based on the findings of this study and the literature reviewed, we suggest use of a "Predictive Score of Safety Parameters" with six (6) items (Tables 3 and 4). The choice of the six (6) items in this score was based on existing scientific evidence, including the CFM Resolution No. 1711 of 12/10/2003, especially Article 9, which established the body area limit (40%) as safety parameter for liposuction (Item 4)24.
Each item has three degrees of complexity (1, 2, and 4 points). The lowest score, six (6) points, corresponds to the sum of the lowest level of complexity for each item; the highest score, twenty-four (24 points), is represented by the sum of the greatest degree of complexity for each item. If we consider the sum of the intermediate degree of each item, twelve (12 points) is an average score and represents the limit of the ideal parameter for safety. Included as risk factors for thromboembolic events are age (older than 40 years), smoking, use of contraceptives or hormone replacement, personal or family history of thrombosis, etc.
An acceptable parameter would be five (5) items of intermediate degree and one item of maximum degree. Exceptions could be made only in special cases with the agreement of a multidisciplinary team and availability of a proper hospital environment.
This scoring system may help surgeons to perform preventive measures and make better choices to avoid these health events. It may also serve as objective guide for determining patient eligibility for surgery, thus protecting plastic surgeons against possible legal actions. After all, the safety of the patient is also the safety of the plastic surgeon.
This "score" should be seen as an alternative in borderline situations for indicating operation that is supported by scientific evidence. It should not be considered definitive, and requires further validation. The second stage of the study provides validation of this score in a prospective study, applied in hospitals and plastic surgery clinics in various regions throughout Brazil.
CONCLUSION
This literature review shows the multifactorial aspects of risk in plastic surgery procedures.
Data about surgical complications show that proper patient selection, preoperative planning, and prophylactic care during intraoperative and postoperative periods have contributed to decreased incidence of serious complications, but more work is required to further increase patient safety. The main risk factors associated with post-surgical complications were surgery durations longer than 4 hours and associated surgery.
We therefore suggest using "predictive scores" to determine safety parameters for plastic surgery procedures (Tables 3 and 4).
ACKNOWLEDGEMENTS
We are grateful to the Accredited Services Regents of the SBCP for their kind participation in providing patient data forms for the statistical analysis in this work.
They are:
Dr. Francisco de Assis Montenegro Carvalho - Instituto Dr. José Frota - CE;
Dr. José Carlos Daher - SCPH Daher Lago Sul - DF;
Dr. José Marcus Mélega - Instituto Santa Cruz - SP;
Dr. José Ronaldo de Castro Roston - SCPHM Mario Gatti - BA;
Dr. José Valber Lima Menezes - Universidade Federal da Bahia - BA;
Prof. Dra. Lydia Masako Ferreira - UNIVESP - SP;Dr. Renato Rocha Lage - Hospital da Baleia - MG;
Dr. Dr. Ognev Meireles Cosac - Hospital das Forças Armadas - DF;
Dr. Salustiano Gomes Pinho Pessoa - HU Walter Contidio - CE;
Dr. Rodrigo D'Eça Neves - SCPQ do hospital da UFSC - SC;
Dr. Ivo Salgado - Hospital Infantil de Pernambuco - PE;
Dr. Jorge Menezes - Hospital Mater Dei - MG;
Dr. José Carlos da Silva - Hospital Geral de Goiânia - GO;
Dr. Carlos Del Pino Roxo - Hospital Federal do Andaraí - SP;
Dr. Eduardo Carlos da Silveira Mendes Jr - SCP de Catanduva - SP;
Dr. Walmor Feijó - Hospital Defeitos da Face - SP;
Dra. Dulce Maria Fonseca Soares Martins - Hospital Santa Marcelina - SP - SP.
We are grateful to the members of the Department of Scientific Events (DEC) of the SBCP for their management from 2010 to 2011 and their participation in planning and discussing the "Patient Safety" forums.
They are:
Dr. Alexandre Piassi Passos;
Dr. Cláudio Cardoso de Castro;
Dr. Humberto Campos;
Dr. Níveo Steffen;
Dr. Péricles Serafim Neto.
REFERENCES
1. Iverson RE, Lynch DJ. Practice advisory on liposuction. Plast Reconstr Surg. 2004;113(5):1478-90; discussion 1491-5.
2. Byrd HS, Barton FE, Orenstein HH, Rohrich RJ, Burns AJ, Hobar PC, Haydon MS. Safety and efficacy in na accredited outpatient plastic surgery facility: a review of 5316 consecutive cases. Plast Reconstr Surg J. 2003;112(2):636-41.
3. Stevens WG, Repta R, Pacella SJ, et al. Safe and consistenbt outcomes of successfully combining breast surgery and abdominoplasty: an update Aesthet Surg J. 2009;29(2):129-34.
4. Iverson RE, ASPS task force on patient safety in office-based surgery facilities. Patient safety in office-based surgery facilities: I. Procedures in the office-based surgery setting. Plastic Reconstr Surg J. 2002;110(5):1337-42.
5. Horton JB, Janis JE, Rohrich RJ. MOC-PS CME Article: patient safety in the office-based setting. Plast Reconstr Surg. 2008 Sep;122(3):1-21.
6. Kjøller K, Holmich LR, acobsen PH, et al. Epidemiological investigation of local complications after cosmetic breast implant surgery in Denmark. Ann Plast Surg. 2002;48(3):229-37.
7. Ferreira MC. Cirurgia plástica estética: avaliação dos resultados. Rev Bras Cir Plast. 2000;15(1):55-66.
8. Araco A, Gravante G, Araco F, Delogu D. A retrospective analysis of 3,000 primary aesthetic breast augmentations: postoperative complications and associated factors. Aesthetic Plast Surg. 2007;31(5):532-9.
9. Honrado CP, Pastorek NJ. Preventing complications in facial plastic surgery. Curr Opin Otolaryngol Head Neck Surg. 2006 Aug;14(4):265-9.
10. Hvilsom GB, Holmich LR, Henriksen TF, et al. Local complications after cosmetic breast augmentation: results from the Danish Registry for Plastic Surgery of the Breast. Plast Reconstr Surg. 2009 Sep;124(3):919-25.
11. Krueger JK, Rohrich RJ. Clearing the smoke: the scientific rationale for tobacco abstention with plastic surgery. Plast Reconstr Surg. 2001;108(4):1063-73; discussion 1074-7.
12. Saldanha OR, Azevedo DM, Azevedo SF, Ribeiro DV, Nagassaki E, Gonçalves Jr P, Set al. Lipoabdominoplastia: redução das complicações em cirurgias abdominais. Rev Bras Cir Plast. 2011;26(2):275-9.
13. Coleman WP, Glougau RG, Klein J, Moy RL. Guidelines of care for liposuction. J Am Acad Dermatol. 2001;45(3):438-47.
14. www.asahq.org/.../ASA-Physical-Status-Classification Howland WS, Schweiser O. Complications associated with prolonged operation and anesthesia. Clin Anesth. 1972;9(1):1-7.
15. Fogarty BJ, Ashall KG, Leonard AG. Complications of long operations: a prospective study of morbidity associated with prolonged operative time (>6h). Br J Plast Surg. 1999 Jan;52(1):33-6.
16. Lehnhardt M, Homman HH, Daigeler A, Hauser J, Palka P, Steinau HU. Major and lethal complications of liposuction: a review of 72 cases in Germany between 1998 and 2002. Plastic Reconstr Surg J. 2008;121(6):396e-403e.
17. Hughes III CE. Reduction of lipoplasty risks and mortality: na ASAPS survey. Aesthet Surg J. 2001;21(2):120-7.
18. Matarasso A, Swift RW, Rankin M. Abdominoplasty and abdominal contour surgery: a national plastic surgery survey. Plast Reconstr Surg. 2006 May;117(6):1797-808.
19. Stevens WG, Repta R, Pacella SJ, et al. Safe and consistenbt outcomes of successfully combining breast surgery and abdominoplasty: an update. Aesthet Surg J. 2009;29(2):129-34.
20. Duarte IG, Ferreira DP. Uso de indicadores na gestão de um centro cirúrgico. Rev Adm Saúde. 2006;8(31):63-70.
21. Hensel JM, Lehman JA, Tantri MP, et al. An outcomes and analysis and satisfaction survey of 199 consecutive abdominoplasties. Ann Plast Surg. 2001;46(4):357-63.
22. Hardy K L, Davis KE, Rian SC, Chen M, Hein R, Jewell JL, et al, - The impact of operative time on complications after plastic surgery: a multivariate regression analysis of 1753 cases. Aesthet Surg J. 2014;34(4):614-22.
23. Gemperli R, Neves RL, Tuma P Jr, Bonamichi GT, Ferreira MC, Manders EK. Abdominoplasty combined with oter intraabdominal procedures. Ann Plast Surg. 1992;29(1):18-22.
1- Accredited service agent of the SBCP - Director of international relations of the SBCP
2- PhD - Coordinator of USP Cosmiatry (Cosmetic dermatology) Sector
3- MD - Resident of the "Dr. EB Souza Pinto" Plastic Surgery Service - UNISANTA
4- MD - Plastic Surgery Specialist
5- MD - Specialist in General Surgery
Institution: Clinic Saldanha.
Corresponding author:
Osvaldo Ribeiro Saldanha
Av. Washington Luiz, 142. Encruzilhada
Santos-SP - Postal Addressing Code (CEP): 11050-200
Article received: May 29, 2014
Article accepted: July 7, 2014


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter