

Body and Chest - Year 2011 - Volume 26 - (3 Suppl.1)
Prophylactic use of human acellular dermal matrix in pelvic reconstruction after sacrectomy and flap coverage
Prophylactic use of human acellular dermal matrix in pelvic reconstruction after sacrectomy and flap coverage
Sacrectomies for malignancy often result in large soft tissue and skeletal defects creating a communication between the surgical site and the abdominal cavity. Soft tissue reconstruction is achieved with local, pedicled, or free flap coverage. Skeletal reconstruction usually requires hardware with or without non-vascularized bone grafts or free fibular flaps. Sacral herniation of abdominal contents after sacrectomies is an uncommon but challenging complication, which can present as bowel obstruction and be of difficult recognition in this particular anatomic location. Intraoperative retraction of bowel through the sacral defect can be laborious, and the presence of adhesions in staged procedures can make the dissection arduous, increasing the risk of bowel injury.
OBJECTIVE
We present our outcomes with the prophylactic use of human acellular dermal matrix (HADM) after sacrectomies and flap coverage to reconstruct the pelvic floor in order to prevent sacral herniation and its possible intraoperative and postoperative complications.
METHODS
Fifty-nine patients who had sacral defect flap reconstruction after a primary oncological resection at the Mayo Clinic, MN (USA) between 1998 and 2008 were reviewed. The use of HADM for this indication in our institution started in 2005 and it has been used in 10 patients. Demographics, risk factors, procedural data, and outcomes were analyzed and compared regarding the presence of HADM. Statistical analysis was performed using either Fisher's exact or Pearson chi-square test.
RESULTS
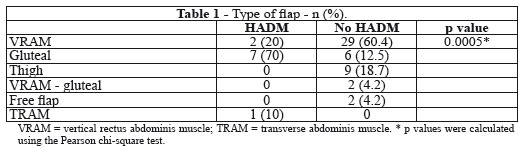
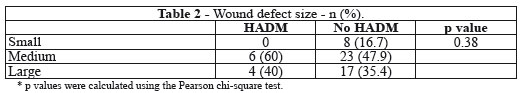
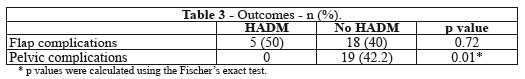
No statistically significant differences in co-morbidities, smoking status, and previous abdominal surgery were observed in the HADM and No HADM groups. The incidence of females was statistically significant (p = 0.04) higher in the HADM group. Preoperative radiation and chemotherapy had a higher incidence (p = 0.01) in the No HADM group. A statistically significant difference (p = 0.0005) in the distribution of HADM use among the different types of flaps was observed, with a higher incidence of use in the gluteal flaps (Table 1). No statistically significant difference (p = 0.38) was found in the distribution of HADM use among wound defect size groups (Table 2). No statistically significant difference was found in flap complications, but the incidence of pelvic complications, related to the cancer resection itself, was statistically significant higher (p = 0.01) in the No HADM group; 19 patients (42 %) versus zero in the HADM group (Table 3). Pelvic complications in the No HADM group included: parasacral hernia (n=1), abscess (n=9), bowel obstruction (n=1), bowel perforation (n=2), enterocutaneous fistula (n=2), hardware failure (n=5), and hematoma (n=2).
CONCLUSION
The prophylactic use of HADM in pelvic reconstruction after sacrectomies in our experience seems to be safe and reliable method to help prevent sacral herniation of abdominal contents and its possible complications, and it is associated with lower pelvic complication rates.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter