

Original Article - Year 2011 - Volume 26 -
Comparative analysis of mammaplasty techniques based on the long-term effect on the nipple-areolar-complex to inframammary crease distance
Avaliação das técnicas de mamoplastia quanto a sua influência tardia na distância do complexo areolopapilar ao sulco inframamário
ABSTRACT
BACKGROUND: Breast cosmetic surgery has focused on the correction of breast volume, suspension, and shape. In most of the breast reduction and mastopexy techniques currently in use, the vascular pedicles responsible for the blood supply to the nipple areolar complex (NAC) are of particular importance. The objective of the present study was to evaluate the results obtained with different techniques and pedicle choices with regard to the maintenance of lower breast pole shape during a postoperative 6-month follow-up period.
METHODS: A total of 20 female patients (40 breasts) with a body mass index (BMI) ranging from 22 to 25 and ages between 21 and 54 years who underwent breast lift and reduction surgery at the Plastic Surgery and Burns Department of Hospital do Servidor Público Estadual de São Paulo were retrospectively analyzed. The superior medial pedicle and Liacyr Ribeiro type I pedicle techniques for mammary reduction were used. The distance between the vertical scar of the NAC and the inframammary crease was measured in the immediate postoperative period and after 6 months to compare the effect of each pedicle on vertical distance maintenance. Statistical analyses were performed by Student's t test, and P values < 0.005 were considered statistically significant.
RESULTS: The pedicles used were superior (n = 16), medial (n = 20), and Liacyr Ribeiro type I (n = 4). The vertical scar (NAC-inframammary crease) measured between 5 cm and 6 cm (mean = 5.6 cm) during the immediate postoperative period, while later postoperative measurements ranged between 5.5 cm and 8 cm (mean = 6.6 cm). The differences in the NAC-inframammary crease distance between the Liacyr Ribeiro type I pedicle (P = 0.2048), superior pedicle (P = 0.0012), and medial pedicle (P = 0.0057) based surgeries only reached statistical significance in the superior pedicle surgery with respect to an increase in this measurement.
CONCLUSIONS: Measurement of the vertical distance between the most caudal portion of the NAC and the inframammary crease scar is simple and might contribute to our understanding of the effect of different pedicle techniques on the long-term results of mammaplasty.
Keywords: Mammaplasty. Breast/surgery. Plastic surgery/methods.
RESUMO
INTRODUÇÃO: A cirurgia plástica mamária tem como foco adequação do volume, suspensão e forma da mama. Diversas técnicas são utilizadas para redução e mastopexia, com grande atenção ao pedículo responsável pelo suprimento vascular do complexo areolopapilar (CAP). O objetivo deste trabalho é avaliar a técnica e a escolha do pedículo na manutenção da forma do polo inferior da mama no seguimento pós-operatório de 6 meses.
MÉTODO: Foi realizada análise prospectiva de 20 pacientes do sexo feminino, totalizando 40 mamas, com índice de massa corporal (IMC) entre 22 e 25 e idade variando de 21 anos a 54 anos, submetidas a mamoplastia (redutora e mastopexia) no Serviço de Cirurgia Plástica e Queimaduras do Hospital do Servidor Público Estadual de São Paulo. Foram empregadas técnicas baseadas em pedículos superior e medial e pedículo tipo I de Liacyr Ribeiro. A distância entre a cicatriz vertical do CAP e o sulco inframamário foi mensurada no pós-operatório imediato e depois de 6 meses, a fim de comparar o efeito de cada pedículo na manutenção da distância vertical. A análise estatística foi feita pelo teste t de Student, considerando significativos valores de P < 0,005.
RESULTADOS: Os pedículos utilizados foram superior (n = 16), medial (n = 20) e tipo I de Liacyr Ribeiro (n = 4). A distância da cicatriz vertical (CAP-sulco inframamário), no pós-operatório imediato, variou de 5 cm a 6 cm, com média de 5,6 cm. As medidas pós-operatórias tardias variaram entre 5,5 cm e 8 cm, com média de 6,6 cm. No que se refere às variações na medida da distância CAP-sulco inframamário quando relacionadas às técnicas de pedículo tipo I de Liacyr Ribeiro (P = 0,2048), de pedículo superior (P = 0,0012) e de pedículo medial (P = 0,0057), apenas o pedículo superior apresentou significância quanto ao alargamento dessa distância.
CONCLUSÕES: A medida da distância vertical entre a porção mais caudal do CAP e a cicatriz horizontal posicionada no sulco inframamário (CAP-sulco inframamário) pode ser obtida de forma simples, a fim de entender a influência de cada pedículo no resultado tardio das mamoplastias.
Palavras-chave: Mamoplastia. Mama/cirurgia. Cirurgia plástica/métodos.
The objective of breast plastic surgery is to restore the youthful and graceful form of the breast. The objectives of this type of surgery range from the decrease of excess glandular tissue in the case of hypertrophy to breast cone remodeling in ptosis. Therefore, the focus of breast reduction surgery is to achieve an adequate volume, and to attain adequate suspension and a new shape of the breast in mastopexies1. Several techniques are currently in use for breast reduction and mastopexy, and the vascular pedicles responsible for the blood supply to the nipple areolar complex (NAC) are particularly important in these procedures.
Breast hypertrophy can be a source of emotional and psychological distress for patients, as well as the cause of multiple problems related to the effects of the excess weight (tissue and glandular weight) on the lumbar area and shoulders as a result of gravity. Although several classification methods for breast hypertrophy have been proposed, there is currently no universal classification system due to the complexity of this condition.
Reduction mammaplasty techniques aim to preserve glandular physiology and a long-term improvement of breast shape while minimizing scars and maintaining the sensitivity of the mammary complex. Reaching these objectives requires a reduction of the excess breast and glandular tissue, a remodeling of the mammary complex, repositioning of the NAC, and resection of excess skin associated with different incisions and scars.
Several techniques have been described and used in recent years. They are based on specific blood supply pedicles that correspond to axial flaps and ensure adequate blood supply to the NAC as well as its displacement to a new position without affecting the new shape of the breast. Such pedicles can be central, lateral, medial, superior, inferior, or combined. With regard to the most commonly used techniques, the method described by Pitanguy in 1961 was based on the use of the superior pedicle, which is supplied by the internal thoracic artery perforators medially and the external thoracic artery laterally2-7. Breast tissue resection is performed by means of digital clamping and estimation of the excess tissue; the NAC is elevated to the point of greatest projection of the breast cone previously identified as point A, and breast crease projection over the midclavicular line. The remaining lateral and medial glandular pillars are then sutured, resulting in a final scar with an inverted T shape.
Reduction mammaplasty using the medial pedicle and the internal thoracic artery perforators is based on a different approach than the classical Pitanguy technique: NAC rotation and elevation are performed with greater safety, without the excessive removal of skin, which can damage NAC flow via the subdermal plexus. Skin resection markings and breast reconstruction are similar to those of the Pitanguy technique, while the pedicle design is different because it requires a base measuring 6 to 10 cm, with 1:1 proportions depending on the case.
Mammary ptosis is characterized by sagging caused by excess skin that is contained and not associated with the volume of its parenchymal content. In the majority of cases, these effects are time-dependent and can be associated with previous pregnancies or significant weight loss. In addition, the breast lipo-substitution process that occurs as a consequence of age and hormonal changes is important as the glandular parenchyma atrophies and is replaced by adipose tissue, accompanied by the failure of the supporting structure of the breast cone via Cooper ligaments.
Mammary ptosis can be classified according to the Regnault or Lalardie scales; the first ranks mammary ptosis as small, moderate, large, glandular, and pseudoptosis, and the second system uses degrees of ptosis.
The treatment of mammary ptosis is aimed at the removal of excess skin while preserving as much tissue as possible in the absence of hypertrophy, thus resulting in satisfactory shape, projection, and dimensions and minimizing long-term scars8-20.
The effect of sagging skin on the shape of the breast content vs. its support is important to keep in mind, in particular with respect to the effect of gravity on the lower pole of the vertical scar.
The technique proposed by Liacyr Ribeiro9 uses a flap of non-areolated inferior pedicle associated with the superior pedicle. This author classified this type of pedicle as type I, in which the dermal-glandular content is used to fill the upper breast pole, commonly empty in patients with mammary ptosis. Pedicle irrigation is derived from the perforating branches of the fourth, fifth, sixth, and seventh intercostal spaces via the internal thoracic artery.
The type I pedicle technique of Liacyr Ribeiro uses the resection markings for breast tissue excess described by Pitanguy, and a bi-digital clamping maneuver that preserves the superior pedicle and consequently the NAC. The inferior dermo-lipo-glandular pedicle flap is used to increase upper pole projection and fullness. The suturing of glandular pillars is performed according to Pitanguy's technique, and the resulting scars also have an inverted T shape.
This work aims to assess the techniques described and analyze the role played by each pedicle on the effect of breast weight on the lower pole during the late postoperative period. The effect on recurrent or residual ptosis can be quantified by comparison between the vertical distances during the early and late postoperative periods.
METHODS
A total of 20 female patients (40 breasts) aged between 21 and 54 years and with a body mass index (BMI) of 22 to 25 who underwent breast lift and reduction surgery at the Plastic Surgery and Burns Department of Hospital do Servidor Público Estadual de São Paulo in 2009 were retrospectively analyzed. The study was approved by the Ethics Committee of the institution. Patients were operated on by a single surgeon, using techniques based on superior, medial, and inferior type I pedicles according to Liacyr Ribeiro's classification. Surgical markings were performed according to the Pitanguy technique.
The patients were photographed in the preoperative period using standardized techniques. The surgeries were performed in a surgical center under general anesthesia, following the standard marking method described by Pitanguy, with bi-digital clamping and a vertical scar. The distance between point A (the projection of the inframammary crease on the midclavicular line) and the position of the most cephalic portion of the NAC determined whether superior or medial areolated pedicles were required. The selection was based on the pedicle mobility and rotation that minimized tension and decreased the risk of vascular impairment.
Non-areolated inferior Liacyr Ribeiro type I pedicles were used in patients with moderate ptosis and decreased upper pole fullness, which was not observed in any of the mammary hypertrophy cases.
The surgical procedure involved resection of excess glandular tissue in cases of breast hypertrophy, and reduction of excess skin in cases of ptosis. The lateral and medial pillars were sutured using 2.0 nylon sutures. Measurements were taken after the final sutures were completed and the NAC was positioned.
During the immediate postoperative period, the length of the vertical scar was measured as the distance between the most inferior point of the NAC and the horizontal scar resulting from the procedure (corresponding to the mammary crease). These values, which ranged from 5 to 6 cm, enabled satisfactory appearance of the breast cone and adequate breast projection.
The measurements were repeated after 6 months to compare the effect of the different techniques on the maintenance of vertical distance, and consequently the shape of the inferior pole. A millimeter ruler was used by an independent evaluator to measure the distance between the caudal end of the NAC and the cephalic portion of the horizontal scar corresponding to the inframammary crease (Figure 1). Notably, patients with enlarged and hypertrophic scars were excluded from the study to avoid bias in the measurement of vertical scars. All patients were photographed in the postoperative period.
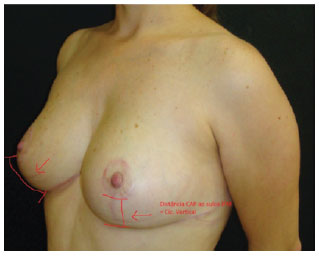
Figure 1 - Distance from the nipple areolar complex to the inframammary crease.
Statistical analysis was carried out to analyze variations in both early and late post-operative vertical distance measurements in relation to the type of pedicle used. The Student's t test was used, and a P value of <0.005 was considered statistically significant.
RESULTS
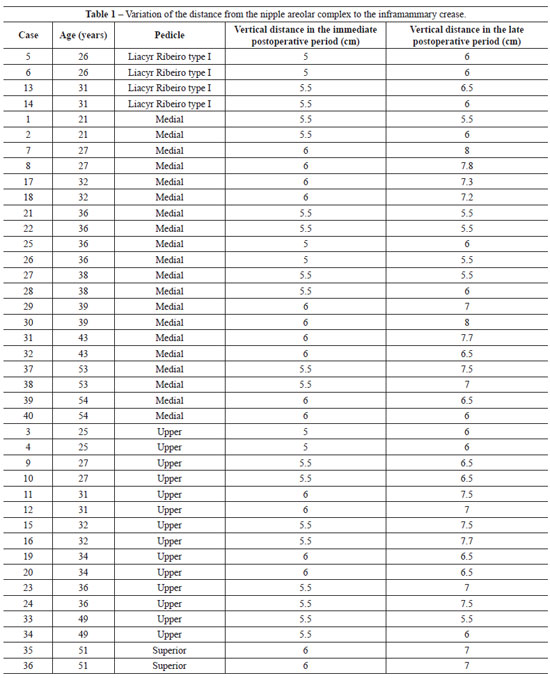
The patients included in the study had moderate breast hypertrophy and ptosis, and all participants were satisfied with the outcome of surgery (Figure 2).
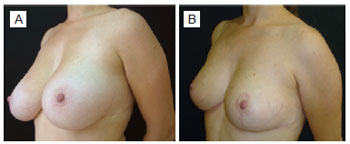
Figure 2 - A, preoperative period. B, postoperative period.
No complications related to the procedure, such as hematomas, seromas, necrosis, or dehiscence, were observed. Patients with hypertrophy or scar enlargement were excluded from the study due to bias in the measurement of the distance between the most caudal portion of the NAC and the horizontal scar corresponding to the mammary crease.
Superior (n = 16), medial (n = 20), and type I Liacyr Ribeiro pedicles (n = 4) were used in the study and each breast was evaluated separately.
The length of the vertical scar (NAC-mammary crease) as measured during the immediate postoperative period ranged from 5 to 6 cm, with an average length of 5.6 cm. Long-term postoperative measurements ranged between 5.5 and 8 cm, with an average of 6.6 cm. The statistical significance of the differences in the NAC-inframammary crease distance in relationship to the surgical technique was as follows: type I pedicle of Liacyr Ribeiro, P = 0.2048; superior pedicle, P = 0.0012; and medial pedicle, P = 0.0057. These results indicate that only superior pedicle surgery resulted in a statistically significant increase in this vertical distance in the lower breast pole (Table 1).
DISCUSSION
There are several surgical techniques for breast reduction and ptosis correction based on specific vascular pedicles that are currently in use, and the choice of a method depends on the specific case. In our service, extensive experience with the use of superior and medial pedicles in mammaplasties and the ensured viability of the NAC makes governs their use in almost all cases. Our technique alternates between the use of the superior and medial pedicles based on the need for elevating the NAC up to a new position at the intersection between the midclavicular line and the mammary crease projection, which we call point A.
In patients requiring an elevation greater than 3 cm, we use the medial pedicle, while the superior pedicle is used when an elevation of less than 3 cm is required. Therefore, all reduction mammaplasties are performed using the medial or superior pedicles.
Breast sagging without associated hypertrophy is corrected with a mastopexy, which consists of the removal of excess skin and tissue and breast lift performed according to the Liacyr Ribeiro type I pedicle technique. This technique is based on the use of a non-areolated dermo-lipo-glandular inferior pedicle in addition to the superior pedicle proposed by Pitanguy to retain volume and upper breast pole filling, which normally shows sagging and ptosis. This approach was used in patients with light to moderate breast ptosis, as well as in Liacyr Ribeiro type I pedicle cases.
Despite the achievement of good short-term results, these techniques should be evaluated with regard to postoperative evolution and the long-term maintenance of the outcome, e.g., shape, NAC positioning, and volume. The vertical distance from the most caudal portion of the NAC to the most cranial portion of the horizontal scar corresponding to the mammary crease is easy to measure during both the immediate and late postoperative periods. This measurement enables an objective assessment of residual and recurrent ptosis because the weight of the glandular tissue at the scar can increase the vertical distance, and this effect varies with each technique. Therefore, each pedicle type and location can exert a different type of pressure on the lower pole, thus expanding the vertical scar in a specific manner in each case. This simple, objective, and practical measure may aid in assessing the results.
Statistically significant differences were not detected among the 20 breasts showing mild to moderate hypertrophy that were corrected using the medial pedicle, which demonstrates the effect of rotational maintenance of the pedicle in a superior position (Figure 3).
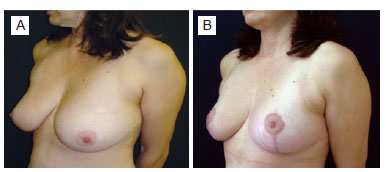
Figure 3 - A, preoperative period. B, postoperative period of mammaplasty with the medial pedicle.
The isolated superior pedicle was used in 16 breasts without complications. The results with respect to the observed vertical scar enlargement were statistically significant. These results could be attributed to a more intense lever effect caused by the lowering of the superior pole to a more caudal position, which could lead to increased pressure on the lower pole. In this context, it is possible to observe an increase in the length of the vertical scar, resulting in a slight change in the appearance of the breast (Figure 4).
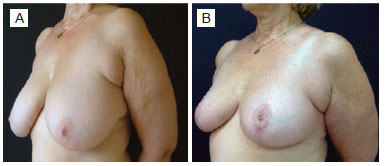
Figure 4 - A, preoperative period. B, postoperative period of mammaplasty with the superior pedicle.
To counter-balance these changes, the upper breast pole was filled using the same areolated superior pedicle added to a dermo-lipo-glandular inferior pedicle, which resulted in the absence of significant variation in the length of the vertical scar. The results obtained, as analyzed on postoperative photographs, confirm the preservation of the upper breast pole and the absence of excessive movement, which enabled the conservation of the shape of the breast and the preservation of the appearance in both poles (Figure 5).
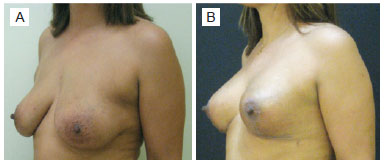
Figure 5 - A, preoperative period. B, postoperative period of mammaplasty with Liacyr Ribeiro type I pedicle.
CONCLUSIONS
Measurement of the vertical distance between the most caudal portion of the NAC and the horizontal scar in the inframammary crease (NAC-inframammary crease) can be performed in a simple manner, both during the immediate and late postoperative periods. This measurement can contribute to our understanding of the influence of each pedicle on the long-term results of mammaplasties. Therefore, it is possible to develop strategies for ensuring long-lasting results by means of objective measures.
REFERENCES
1. Arié G. Una nueva técnica de mastoplastia. Rev Latinoam Cir Plast. 1957;3(1):23-31.
2. Pitanguy I. Surgical treatment of breast hypertrophy. Br J Plast Surg. 1967;20(1):78-85.
3. Pitanguy I. The breast. In: Pitanguy I, ed. Aesthetic plastic surgery of head and body. Berlin:Springer;1981.
4. Pitanguy I. Reduction mammaplasty by the personal technique. In: Chang WHJ, ed. The breast: an atlas of reconstruction. Baltimore: Williams and Wilkins; 1984. p. 75-160.
5. Pitanguy I. Reduction mammaplasty: a personal odyssey. In: Goldwyn RM, ed. Reduction mammaplasty. Boston: Little, Brown; 1990. p. 95.
6. Pitanguy I, Radwanski HN. Philosophy and principles in the correction of breast hypertrophy. In: Mang WL, Bull HG, eds. Ästhetische chirurgie. Berlin: Einhorn Presse; 1996. p. 216-32.
7. Pitanguy I. Evaluation of body contouring surgery today: a 30-year perspective. Plast Reconstr Surg. 2000;105(4):1499-514.
8. Baroudi R. Preoperative evaluation for breast surgery. In: Georgiade ND, ed. Aesthetic surgery of the breast. Philadelphia: Saunders; 1990. p. 19.
9. Ribeiro L. Cirurgia plástica da mama. Rio de Janeiro: Medsi; 1989.
10. Hidalgo DA. Improving safety and aesthetic results in inverted T scar breast reduction. Plast Reconstr Surg. 1999;103(3):874-86.
11. Hidalgo DA, Elliot LF, Palumbo S, Casas L, Hammond D. Current trends in breast reduction. Plast Reconstr Surg. 1999;104(3):806-15.
12. Jackson IT, Bayramicli M, Gupta M, Yavuzer R. Importance of the pedicle length measurement in reduction mammaplasty. Plast Reconstr Surg. 1999;104(2):398-400.
13. Kakagia D, Tripsiannis G, Tsoutsos D. Breastfeeding after reduction mammaplasty: a comparison of 3 techniques. Ann Plast Surg. 2005;55(4):343-5.
14. Kreithen J, Caffee H, Rosenberg J, Chin G, Clayman M, Lawson M, et al. A comparison of the LeJour and Wise pattern methods of breast reduction. Ann Plast Surg. 2005;54(3):236-41.
15. Lacerna M, Spears J, Mitra A, Medina C, McCampbell E, Kiran R, et al. Avoiding free nipple grafts during reduction mammaplasty in patients with gigantomastia. Ann Plast Surg. 2005;55(1):21-4.
16. Lassus C. Breast reduction: evolution of a technique--a single vertical scar. Aesthetic Plast Surg. 1987;11(2):107-12.
17. Lassus C. A 30-year experience with vertical mammaplasty. Plast Reconstr Surg. 1996;97(2):373-80.
18. Lejour M. Vertical mammaplasty and liposuction of the breast. Plast Reconstr Surg. 1994;94(1):100-14.
19. Lejour M. Vertical mammaplasty: early complications after 250 personal consecutive cases. Plast Reconstr Surg. 1999;104(3):764-70.
20. Lista F, Ahmad J. Vertical scar reduction mammaplasty: a 15-year experience including a review of 250 consecutive cases. Plast Reconstr Surg. 2006;117(7):2152-65.
1. Plastic Surgeon, associate member of the Brazilian Society of Plastic Surgery (SBCP), physician and post-graduate student (Masters degree) at the Plastic Surgery and Burns Department of Hospital do Servidor Público Estadual de São Paulo (HSPE-SP), São Paulo, SP, Brazil.
2. Plastic surgeon, PhD, full member of SBCP, head of the Plastic Surgery and Burns Department of HSPE-SP, São Paulo, SP, Brazil.
3. Plastic surgeon, full member of SBCP, assistant physician of the Plastic Surgery and Burns Department of HSPE-SP, São Paulo, SP, Brazil.
4. Resident physician at the Plastic Surgery and Burns Department of HSPE-SP, São Paulo, SP, Brazil.
Correspondence to:
Alexandre Andrade Souza
Rua Tancredo Serra e Silva, 2.049 - ap. 304 - bl. 6 - Horto
Teresina, PI, Brazil - CEP 64052-475
E-mail: alex_andrade@hotmail.com
Paper submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: August 25, 2011
Paper accepted: October 31, 2011
Study conducted at the Plastic Surgery and Burns Department of Hospital do Servidor Público Estadual de São Paulo (HSPE-SP), São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter