

Articles - Year 2003 - Volume 18 - Issue 1
A Prevention Protocol for Deep Vein Thrombosis in Plastic Surgery
Um Protocolo de Prevenção de Trombose Venosa Profunda em Cirurgia Plástica
ABSTRACT
Deep vein thrombosis is increasingly being discussed in plastic surgery. Although the incidence is low, there are major repercussions due to its complications. After reviewing the literature, the authors realized that there is no specific protocol for the condition that can be a basis for assessment and management. The authors propose a specific protocol with risk factors assessed within a scoring system, that once totaled, translates the level of risk that may be low, moderate or high. Prevention, pharmacological and non-pharmacological measures are suggested for each level. The authors conclude that the protocol is easy to use in clinical practice, can be copied and repeated, and can also work as a parameter for evaluating future studies.
Keywords: Deep vein thrombosis; anticoagulants; pulmonary embolism; prophylaxis
RESUMO
A ocorrência de trombose venosa profunda tem sido cada vez mais discutida na cirurgia plástica. Embora os seus índices sejam pequenos, a repercussão de suas complicações é importante. Após rever a literatura, os autores constataram não haver um protocolo específico para esta especialidade que possa servir de base de avaliação e conduta. Os autores propõem um protocolo específico com fatores de risco avaliados em sistema de pontos que, uma vez somados, conferem o grau de risco, que pode ser pequeno, médio e alto. Para cada nível de risco são sugeridas medidas de prevenção farmacológicas e não farmacológicas. Os autores concluem que este protocolo é de fácil execução na rotina clínica, pode ser copiado e repetido e, também, servir de parâmetro de avaliação para futuras pesquisas.
Palavras-chave: Trombose venosa profunda; anticoagulantes; embolia pulmonar; profilaxia
The complications of deep vein thrombosis (DVT) and pulmonary embolism have been the center of a certain amount of attention in plastic surgery in recent years (1-4).
Even so, there are few studies on the incidence of DVT in plastic surgery. Teimourian in 1989 and Reinisch in 1998, reported results from questionnaire surveys sent to American plastic surgeons. Reinish reported 0.39% of DVT and 0.16% of pulmonary vein embolism after esthetic face surgery(5). Some cases of embolism due to fat or vein thrombosis were described in abdominal dermolipectomy alone or associated with liposuction(6).
Scientific studies in other medical specialties have increasingly attempted to standardize prophylaxis procedures for DVT Various kinds of protocols have been reported and tested(7).
In the case of plastic surgery, the American Society of Plastic Surgery organized a Task Force, whose results were published in 1999 by McDevitt(3). The publication discusses risk factors and indicates some prophylactic measures, although there did not exist a protocol that could be repeated in various centers, which would have helped compare clinical trials and give actual data on the incidence and morbidity of DVT in plastic surgery.
When, in 1999, surgical protocols for the most frequent plastic surgeries performed at Hospital Israelita Albert Einstein, in São Paulo, Brazil were implemented, we realized that there was no specific protocol for DVT prophylaxis in plastic surgery. A Study Group consisting of plastic surgeons and intensive care physicians was created in order to investigate and identify patients with a possible risk for DVT in plastic surgery, especially in surgeries considered primarily esthetic(8). Once the risk was acknowledged, we studied prophylaxis care according to the level of risk of the patient.
The main objective was to create a simple, objective and easy-toconsult protocol, in which the plastic surgeon could identify and quantify risk factors during the preoperative period, and which could also help him/her indicate the best management to avoid DVT and its complications. The protocol was meant to be completely repeatable by other medical centers to allow for comparison of data obtained.
RESULTS
The risk factors that lead to DVT are common to any patient. However, if we only analyze elective plastic surgery, we will rarely find the conditions that will require the greater clinical care pre established in medical literature, because many clinical conditions that increase the risk of DVT will themselves be a contraindication for the procedure, although there are exceptions, as in urgencies or reconstructions.
On the other hand, certain surgeries or measures are specific to plastic surgery and increase the risk of DVT, due to the type of position and time the patient remains in surgery, the duration of the surgical procedure, physiopathologic consequences of surgical trauma, and limitations of activity in the postoperative period.
Other risk conditions are very frequent in our specialty, such as the fact that most esthetic surgery patients are women in age groups that frequently utilize contraceptives or hormone replacement therapy, situations that are acknowledged as increasing the risk for DVT(9).
That is why we decided to design a Risk Factors Table specific to plastic surgery, according to the scenarios we may fmd in our routine work. It consists of two distinct groups: one for factors considered clinical, also comprising medication that may facilitate DVT, and another group comprising surgical events and management during the intra and postoperative periods, that seem to facilitate the occurrence of DVT Many of the factors are specific to plastic surgery and will rarely be encountered in other specialties (Table I) .
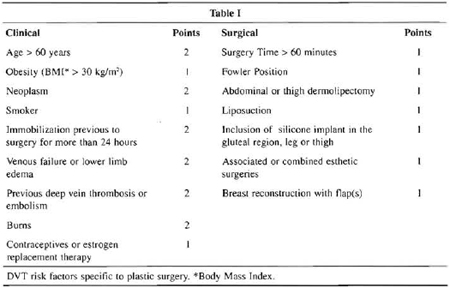
Risk assessment was based on a scoring system reported by Weinman in 1994, that ascribes a certain number of points to each item according to the level of risk(10). The total number of points identifies the level of risk, classified as low, moderate or high. The classification and quantification of the level of risk make it easier to categorize management, which we have divided into pharmacological and non-pharmacological measures (Table II).

The patient risk is classified as low, moderate or high according to the final score in Table I. Adequate prophylaxis is indicated in Table II.
Non-pharmacological measures do not represent major clinical side effects, though they increase the cost of the procedure. The basic aim is to activate blood return to lower limbs. It is acknowledged that more than 95% of thrombi are formed in the legs as a result of lack of movement of calf muscles, which is important for blood return. In longer surgical procedures with completely inactive lower limbs, the likelihood of stasis and thrombosis gradually increases with time. Once DVT occurs, there is a large chance of loosening a proximal part of a thrombus and of it embolizing, mainly from the lung, frequently hours after the end of the surgery, when the lower limb is finally mobilized(10-12) .
In longer procedures, handling lower limbs and early walking are very important (Fig. 1). Whenever there is a greater level of risk, it is important to use intermittent pneumatic compression (Fig. 2), from the beginning of anesthesia to recovery and initial walking, and the device should follow the patient to his inpatient bed.

Fig. 1 - Flexion of the foot during surgery for activating calf muscles when intermittent compression devices cannot be used.

Fig. 2 - Pneumatic compression device for lower limbs.
Elastic stockings with graded pressure are recommended for patients with a previous history of venous failure or thromboembolic phenomena. The stockings are widely used in General Surgery, Neurosurgery and in Intensive Care patients (Fig. 3) (7). The use should be continued for a few days, especially when the surgery involves lower limbs, as is the case of liposuction and prosthetic implants.
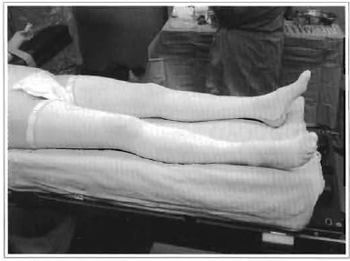
Fig. 3 - Elastic stockings with graded pressure.
Pharmacological measures include those most frequently indicated in DVT prophylaxis. Their use, however, is debatable due to the lack of objective data on changes in blood clotting during and after surgery. It is important to mention that there are no scientific reports on the possible consequences that they may have on plastic surgery(3). It is important to use all non-pharmacological and accessible means of prevention, especially in moderate risk cases, to try to avoid using anti-coagulants, until their utilization has been standardized.
The decision to use anti-coagulants should also take into account the kind of anesthesia to be performed. Spinal anesthesia is avoided whenever prophylactic anti-coagulants are used. Others consider general anesthesia in prolonged surgeries with inactive lower limbs to be a risk factor that could be avoided if routine care measures are performed (5).
In conclusion, we consider the present protocol as progress in relation to the measures suggested by ASPS, in which there is a long description and classification of risk factors not directly connected to the necessary clinical measures, in addition to not allowing the creation of a database that could be entirely repeated, favoring comparative reports (3). It is important that we have an effective assessment of the DVT index in plastic surgery in order to increasingly decrease the incidence of complications.
REFERENCES
1. Few JW, Marcus JR, Placik OJ. Deep vein thrombosis prophylaxis in the moderate to highrisk patient undergoing lower extremity liposuction [letter]. 1999;104:309.
2. Jewell ML. Prevention of deep vein thrombosis in aesthetic surgery patients. Aesth Plast Surg. 2001;21:161-3.
3. McDevitt NB. Deep vein thrombosis prophylaxis. Plast Reconstr Surg. 1999;104: 1923-8.
4. Teimourian B, Rogers WBIII. A national survey of complications associated with suction lipectomy: A comparative study. Plast Reconstr Surg. 1989;84:628-31.
5. Reinish JF, Rosso RF, Bresnick SD. Deep vein thrombosis and pulmonary embolus following face lift: A study on incidence and prophylaxis. Plast Surg Forum. 1998;21:159.
6. Rao RB, Ely SF, Hoffman RS. Deaths related to liposuction. N Engl J Med. 1999;340(19):14715.
7. Baruzzi ACA, Knobel E. Profilaxia da trombose venosa profunda. Rev Bras Clin Terap. 1996;22:61-4.
8. Hospital Israelita Albert Einstein. Protocol os de Conduta. São Paulo; 1999.
9. Daly E, Vessey MP, Hawkins MM, Carson JL, Gough P, Marsh S. Risk of venous thromboembolism in users of hormone replacement therapy. Lancet. 1996;348:977-80.
10. Weinmann EE, Salzman EW. Deep-vein thrombosis. N Engl J Med. 1994;331:1630-45.
11. Huber 0, Bounameaux H, Borst F, Rohner A. Postoperative pulmonary embolism after hospital discharge : an underestimated risk. Arch Surg. 1992;127:310-3.
12. Kakkar VV, Howe CT, Flanc C, Clarke ME. Natural history of postoperative deep-vein thrombosis. Lancet. 1969;2:230-2.
I - Plastic surgeon of the Plastic Surgery Reference Team of Hospital Israelita Albert Einstein. Plastic surgeon of Instituto Dante Pazzanese de Cardiologia de São Paulo.
II - Cardiologist of the Adult Intensive Care Unit of Hospital Israelita Albert Einstein - São Paulo.
III - Head Physician of the Adult Intensive Care Unit of Hospital Israelita Albert Einstein - São Paulo.
Address for correspondence:
Jaime Anger, MD
Av. Brigadeiro Luiz Antonio, 3889
01401-001 -São Paulo -SP Brazil
Phone: (55 11) 3887-8524
e-mail: janger@link.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter