ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Lipoabdominoplasty - Saldanha's Technique
Lipoabdominoplastia - Técnica Saldanha
Articles -
Year2003 -
Volume18 -
Issue
1
Osvaldo Ribeiro SaldanhaI, Ewaldo Bolivar de Souza PintoII, Wilson Novaes Matos Jr.III, Reynaldo Luís LuconIV, Felipe MagalhãesIV, Erika Mônica Lopes BelloIV, Madeleine Ramos dos SantosIV
ABSTRACT
The objective of this paper is to present a new surgical concept for the aesthetic treatment of the abdominal region, combining the principles of liposuction and traditional abdominoplasty, without flap detachment. Following the idea of not carrying out traditional supraumbilical detachment and using superficial liposuction, the authors peiformed lipoabdominoplasty, thus preserving, abdominal perforans vessels, and reducing vascular damages to the skin of the abdominal flap. Moreover, the improvement in shape should be noted, wi a younger-looking abdomen, and uniformity of the flap with the pubis.
Keywords:
Liposuction; abdominoplasty; lipoabdominoplasty
RESUMO
O objetivo deste trabalho é apresentar um novo conceito cirúrgico para o tratamento estético da região abdominal, utilizando os princípios da lipoaspiração e da abdominoplastia tradicional, sem descolamento do retalho. Seguindo a idéia de não se fazer o descolamento tradicional da região supra-umbilical e utilizando a lipoaspiração superficial, os autores executam a lipoabdominoplastia, preservando, assim, os vasos perfurantes abdominais, diminuindo o comprometimento vascular da pele do retalho abdominal. Atentam ainda para a melhoria da forma, com a aparência mais jovem do abdome, e a uniformidade do retalho com o púbis.
Palavras-chave:
Lipoaspiração; abdominoplastia; lipoabdominoplastia
INTRODUCTION
Since 1980, with the origin of liposuction, introduced by Illouz(l), there has been major progress in the approaches to the abdominal region, with changes in the indication for abdominoplasties, which have been sub-divided into liposuction, liposuction with minor resection of the suprapubic skin, and traditional abdominoplasty with additional liposuction of the back and flanks.
In 1985, Hakme(2) described miniabdominoplasty, combined with the technique of liposuction, with resection of excess skin from the suprapubic region, for selected cases.
Recently, in 2000, Avelar(3) presented a study in which he partially removed the suprapubic skin, similarly to Hakme, but did not detach the infraumbilical flap, nor resect the panniculus or the connective tissue, thus preserving the umbilical scar.
Within this evolution, a major breakthrough was the superficial liposuction described by Souza Pinto(4,5), which proposed the treatment of superficial and deep fat, thus providing greater skin retraction.
In spite of technical advances in the treatment of the abdominal region, classical abdominoplasty(6,7) remains a surgical procedure which statistically presents a large number of complications, like hematomas, seromas, epitheliosis and skin necrosis, besides additional interventions to correct scars and "ears" in the late postoperative period. The major detachment of the abdominal flap is, undoubtedly, mainly to blame for the high incidence of seromas, epitheliosis, and skin necrosis, especially for smoking patients.
Some surgeons (8) perform liposuction and abdominoplasty in a single operation, although most of them perform these two procedures in two separate operations (generally six months apart), due to the risk of vascular damage.
In 1992, Illouz(9) published an abdominoplasty technique without detachment, indicated for patients with apron abdomen or supra umbilical abdominoplasties, in which a block above the umbilical scar was resected, followed by upper liposuction and neoumbilicoplasty, which could also be followed by a limited plicature of the rectoabdominal muscle.
Lipoabdominoplasty, as we suggest, provides access to that technique to a wider range of patients. Today we use it for all cases with an indication for classical abdominoplasty. Resection is limited to the infraumbilical skin, thus preserving lymphatic circulation and the connective tissues, and fat is aspirated. The umbilical scar is also treated differently, which we do traditionally, following the star-shaped omphaloplasty (10), and, in cases with diastasis of the rectus abdominis muscles, plicature is performed in the median line from the pubis to the xiphoid process.
The objective of this paper is to present a new surgical concept for the aesthetic treatment of the abdominal region, combining the principles of Liposuction and traditional abdominoplasty, without flap detachment. The supraumbilical skin is slid towards the pubic region widely and naturally, due to the undermining produced by the liposuction cannulas. The abdominal perforans vessels are thus preserved, reducing vascular damage in the skin of the abdominal flap.
CASES AND METHOD
From January 2000 to February 2002, sixty-five female patients were operated; their ages ranged from 28 to 52 years.
Patients who had been referred for classical abdominoplasty were selected to undergo lipoabdominoplasty, including patients with diastasis of the rectoabdominal muscles.
SURGICAL TECHNIQUE
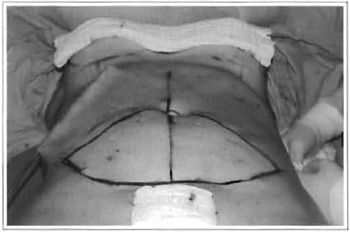
Ater marking, the abdominal region was infiltrated with saline solution with adrenaline at 1:1,000,000 (Fig. 1).
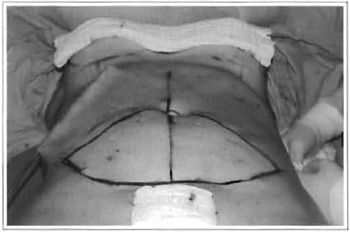
Fig. 1 - Marking and liposuction in the upper abdomen.
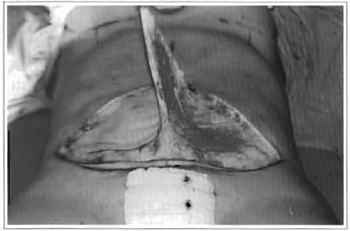
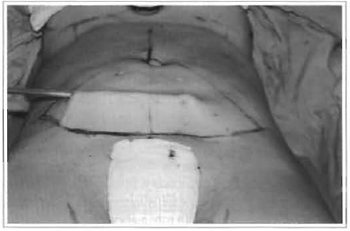
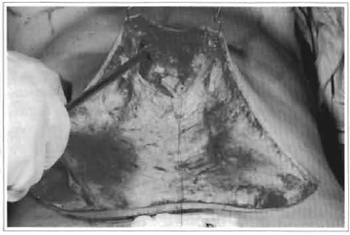
Aspiration started in the supraumbilical region (Fig. 1), moving on to the flanks and then to the infraumbilical region (Fig. 2). Once liposuction was completed, the navel was isolated and only infraumbilical skin was resected (Fig. 3) (similar to classical abdominoplasty), but preserving the thin remaining panniculus, as well as lymphatic, arterial and venous vessels (Fig. 4). If necessary, additional open liposuction is performed. Then, two hooks are used to lift the flap to complete the liposuction of the upper abdomen, uniformizing runnels (Fig. 4). In order to better lift the navel, divulsion of the supra-umbilical fat is performed.
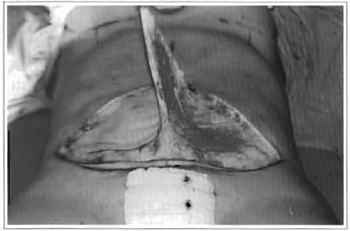
Fig. 2 - Liposuctjon in the lower abdomen.
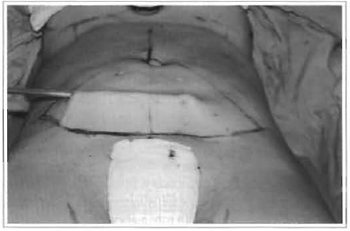
Fig. 3 - Skin resection.
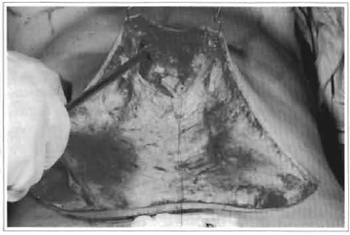
Fig. 4 - Preserved vessels and additional liposuction (upper abdomen).
For patients with indication for plicature of the rectus abdominis, divulsion or detachment of the subcutaneous tissue is performed over the median line, avoiding going beyond the internal borders of these muscles, thus preserving abdominal perforans vessels (Fig. 5). In the infra umbilical portion, the fat tissue is resected at the median line, and then conventional plicature of the aponeurosis is performed.

Fig. 5 - Marking the plicature.
Star-shaped omphaloplasty is performed, which consists of marking a "cross" on the abdominal skin.
The navel is then pulled out at its cardinal points with a forceps, and then small triangular resections are performed between these points, so that the navel fits into the cross-shaped incision on the skin, to be then fixed with subdermal sutures with Nylon 5-0.
The abdomen is closed at two levels, with mononylon 3-0 for the subcutaneous cellular tissue, and 5-0 for the subdermis. Suction drains are used in all cases, and then removed on the 5th postoperative day (Fig. 6).

Fig. 6 - Vacuum drainage and final aspect.
RESULTS
The 65 patients treated with this technique presented good outcomes, both according to our assessment and according to their own opinions. In one case, we noted the presence of a seroma on the 12th postoperative day; this was solved satisfactorily with sessions of syringe suction. There were no complications such as hematomas, suture dehiscence, epitheliosis, necrosis, or infection.
The borders of the flap accommodated better in the suprapubic region, due to the homogeneous thickness of the fat tissue, provided by liposuction. Consequently, the "dog ears" occurred less frequently than they do in the traditional technique, in addition to a smaller fmal scar.
Shape and contour also improved, with a younger-looking abdomen (Fig. 7).

Fig. 7a - Preoperative: 39 years old.

Fig. 7b - Postoperative: 3 months.

Fig. 7c - Preoperative: 39 years old.

Fig. 7d - Postoperative: 3 months.
DISCUSSION
Classical abdominal plastic surgery presents high morbidity, due to the need for major detachment, which damages the lymphatic and perforans vessels that supply the abdominal flap.
The fundamentals of the lipoabdominoplasty technique are based on not detaching the abdominal flap, so as to preserve the perforans and lymphatic vessels, and reduce the complications caused by large detachments, like seromas, hematomas, epitheliosis, and skin necrosis.
This technique treats localized fat in all abdominal regions, with wider traction in the higher portions of the upper abdomen, thus providing a more harmonious abdominal silhouette (Fig. 8).

Fig. 8a - Preoperative: 36 years old.

Fig. 8b - Postoperative: 6 months.

Fig. 8c - Preoperative: 36 years old.

Fig. 8d - Postoperative: 6 months.
Even though nearly all surgeons perform plicature of the rectus abdominis on a routine basis, there are studies that question its effectiveness for the less severe cases of diastasis(11), considering the capacity of musculoaponeurotic contention, which is reinforced by postoperative fibrosis.
CONCLUSION
The search for better results and reduced complication rates is, undoubtedly, the major concern of plastic surgeons.
With lipoabdominoplasty we believe we have found a safer manner to treat the abdominal region, with reduced morbidity, and more harmonious results. This new approach provides a younger-looking abdominal silhouette, better accommodation of the flap in the suprapubic region and smaller more aesthetic scars.
REFERENCES
1. Illouz YG. Study of subcutaneous fat. Aesth Plast Surg. 1990; 14(3):165-77.
2. Hakme F. Technical details in the Lipoaspiration associated with liposuction. Rev Bras Cir. 1985; 75(5):331-7.
3. Avelar JM. Abdominoplasty: a new technique without undermining and fat layer removal. Arq Catarin Med. 2000; 29:147-9.
4. Souza Pinto EB, Almeida AE, Knudsen AF, Andrade SM, de Medeiros Jc. A new methodology in abdominal aesthetic surgery. Aesrh Plast Surg. 1987;11(4):213-22.
5. Souza Pinto EB. Superficial Liposuction. Rio de Janeiro: Revinter; 1999.01-04.
6. Pitanguy I, Gontijo de Amorim NF, Radwanski HN. Contour surgery in the patient with great weight loss. Aesth Plast Surg. 2000; 24(6) :406-11.
7. Pitanguy I. Abdominoplaty: Classification and surgical techniques. Rev Bras Cir. 1995; 85:2344.
8. Dellerud E. Abdominoplasty combined with suction lipoplasty: a study of complication, revisions, and risk factors in 487 cases. Ann Plast Surg. 1990; 25(5):333-8.
9. Illouz YG. A new sate and aesthetic approach to suction abdominoplasry. Aesth Plast Surg. 1992; 16(3) :237-45.
10. Saldanha O. Star-Shaped onfhaloplasry, 498: Annals of The International Symposium RAPS/90. 1990 Mar; Sao Paulo, Brazil.
11. Marques A. Abdominoplasry without muscle plication. Rev Soc Bras Cir Plast. 1993; 8 (2):103-8.
I - Head of the plastic surgery service "Dr. Ewaldo Bolivar de Souza Pinto", Santos, SP
II - Director of the post-graduate course in Plastic Surgery of UNISANTA, Santos, SP
III - Assistant professor of the plastic surgery service "Dr. Ewaldo Bolivar de Souza Pinto".
IV - Resident physician of the plastic surgery service "Dr. Ewaldo Bolivar de Souza Pinto".
Address for correspondence:
Osvaldo Ribeiro Saldanha, MD
Av. Washington Luiz, 142 - Encruzilhada
11050-200 -Santos -SP Brazil
e-mail: dinica@dinicasaldanha.com.br
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license