INTRODUCTION
The World Health Organization (WHO) classifies obesity as a highly complex
Chronic Noncommunicable Disease (NCD) and is considered a challenge of the 21st
century, with global repercussions. According to the Atlas of the Food and
Nutritional Situation in Brazil, published by the Ministry of Health in 2020, a
survey involving 12,776,938 adults revealed that 63% of them are overweight.
Obesity is a multifactorial condition, presenting a significant risk due to its
comorbidities and psychosocial impacts that worsen with increased weight.
Social stigma is an additional factor that harms the condition of obese
people1. Psychological disorders such
as depression, anxiety, binge eating, low self-esteem, and dissatisfaction with
body image have been frequently associated with obesity.2,3. The importance of
a multidisciplinary team in the treatment of obesity is highlighted by some
studies, since, in addition to promoting health, these professionals act as
support for the patient.4,5
Some authors agree that bariatric surgery is an effective and most common
resource worldwide to treat morbid obesity and its results can promote
psychological well-being.6 However, rapid
and significant weight loss can result in the appearance of excess skin, causing
sores and bad odors in the skin folds. This condition can be uncomfortable and
affect both physical health and self-esteem. Furthermore, the changes that occur
in the person’s life as a result of the surgery and the difficulty in adapting
between the perception of their own thin body and their self-image can lead to
psychological problems.7
Plastic surgery, being the only procedure that can remove excess skin resulting
from major weight loss, has the potential to optimize the results of bariatric
surgery. This, in turn, encourages weight control and contributes to improving
people’s self-esteem and psychological well-being.8 However, patients with psychological distress may express
dissatisfaction with the outcome of plastic surgery, even when the initially
planned goal has been achieved. Patients with Body Dysmorphic Disorder (BDD) who
undergo plastic surgery may experience a worsening of their psychological
condition, which may compromise satisfaction with the results obtained.9
This study aims to alert and raise awareness among plastic surgeons, bariatric
surgeons, and the interdisciplinary team about the relevance of the
biopsychosocial approach in the preoperative care of patients who wish to
undergo plastic surgery after bariatric surgery. During the screening phase
carried out by the plastic surgeon, psychological assessment plays two important
roles. Firstly, it allows you to explore the patient’s desires, expectations,
anxieties, and fantasies. Secondly, the assessment process, combined with
careful and transparent feedback from the doctor when the patient shows signs of
psychological distress, helps the patient to recognize the need and importance
of further psychological investigation, conducted by specialists. This initial
approach aims to understand the person’s emotional and psychological context,
promoting the patient’s mental health.
OBJECTIVE
The present study, through a scoping review, aimed to determine whether a basic
psychological assessment, conducted during plastic surgeon screening, can
identify psychological distress in patients seeking post-bariatric plastic
surgery.
METHOD
The present study is a scoping review and is part of the project entitled
“Protocolo de Atenção Biopsicossocial em Cirurgia Plástica
Pós-bariátrica” (Biopsychosocial Care Protocol in Post-bariatric
Plastic Surgery). This project was conducted during the Professional Master’s
degree in Sciences, Technology, and Management Applied to Tissue Regeneration at
the Universidade Federal de São Paulo (Unifesp). The study was approved by the
Unifesp Ethics and Research Committee, with opinion number 5825924. The
corresponding proof is 097949/2022, and the Certificate of Presentation of
Ethical Appreciation (CAAE) has the number 62914222.2.0000.5505.
Initially, the following research question was formulated using the acronym PICO:
Can biopsychosocial care for pre-operative post-bariatric plastic surgery
patients identify psychological suffering related to excess skin? Segmented into
P = Pre-operative post-bariatric plastic surgery patient, I = Biopsychosocial
care, C = Not applicable, O = Identification of psychological suffering related
to excess skin. Next, the acronym FINER was applied to assess whether the
question was well formulated.
Articles published between 2013 and 2023 were searched, in Portuguese, English,
and Spanish, on the database platforms: MEDLINE, Virtual Health Library (VHL),
and Embase, using the Health Sciences Descriptors (DECS/MeSH): psychosocial
functioning, plastic surgery, bariatric surgery and body image. The search
strategy used was: [(“psychosocial functioning” OR “bariatric surgery”) AND
(“plastic surgery” OR body image)]. The inclusion criteria for selecting the
studies were research with adults of both sexes and with bariatric surgery and
post-bariatric plastic surgery patients. The non-inclusion criteria were studies
with adolescents, comments from experts, posters, theses, and incomplete
articles. The exclusion criteria were duplicate articles and studies of plastic
and bariatric surgeries without focusing on the psychological context. To manage
references from the bibliographic survey, including identifying duplicates and
applying eligibility criteria, the Rayyan.ai and Zotero.org platforms were
used.
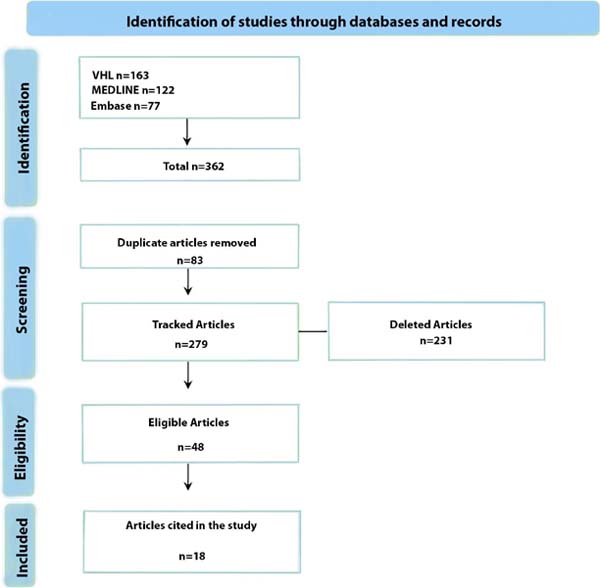
Therefore, 48 articles met the inclusion criteria. Of these selected, 18 were
cited in this study, as they were directly aligned with the relevance of the
topic in the research approach. Additionally, this study adhered to the
recommendation of the Revista Brasileira de Cirurgia Plástica
to use updated references, that is, articles published in the last 5 years. The
18 most recent references satisfactorily fulfilled the purpose established for
this study.
RESULTS
The bibliographic survey conducted retrieved a total of 362 studies. Among these,
48 were selected because they met the established inclusion criteria, as
illustrated in the flowchart in Figure 1.
Figure 1. - Flowchart of the bibliographic survey.
Figure 1. - Flowchart of the bibliographic survey.
Of these selected articles, 18 were cited and discussed in this scoping review,
as highlighted in Chart 1.
Chart 1. - Articles included in the bibliographic survey and mentioned in this
article.
| Nº |
Title |
Author |
Year |
| 1 |
Gender difference in requesting abdominoplasty, after bariatric
surgery: Based on five years of experience in two centers in
Sulaimani Governorate
|
Ahmed HO, Arif SH, Abdulhakim SA, Kakarash A, Ali Omer MA, Nuri
AM.
|
2018 |
| 2 |
Eating attitudes, perceptions of
body image, and patient quality of life before and after
bariatric surgery
|
Akkayaoğlu H, Çelik S. |
2020 |
| 3 |
Beyond Body Size: Focusing on Body Functionality to Improve
Body Image Among Women Who Have Undergone Bariatric Surgery
|
Alleva JM, Atkinson MJ, Vermeulen W, Monpellier VM, Martijn
C.
|
2023 |
| 4 |
Patient-Reported Satisfaction
Following Post-bariatric Surgery: A Systematic Review
|
Barone M, Cogliandro A, Salzillo R,
Tambone V, Persichetti P.
|
2018 |
| 5 |
Body Image Concerns and Associated Impairment Among Adults
Seeking Body Contouring Following Bariatric Surgery
|
Bennett BL, Grilo CM, Alperovich M, Ivezaj V. |
2022 |
| 6 |
Insatisfação com a imagem corporal
em indivíduos com obesidade que procuram cirurgia bariátrica:
explorando a carga de novos fatores mediadores.
|
Bianciardi, Emanuela; Di Lorenzo,
Giorgio; Niolu, Cinzia; Betro, Sophia; Zerbin, Francesca;
Gentileschi, Paulo; Siracusano, Alberto.
|
2019 |
| 7 |
Transtorno Dismórfico Corporal: revisão da literatura |
Bonfim GW, Nascimento IPC, Borges NB. |
2016 |
| 8 |
Comparing Bariatric Surgery
Patients Who Desire, Have Undergone, or Have No Desire for Body
Contouring Surgery: a 5-Year Prospective Study of Body Image and
Mental Health
|
Buer L, Kvalem IL, Bårdstu S, Mala
T.
|
2022 |
| 9 |
Atuação da equipe interdisciplinar no pós-operatório de
cirurgia bariátrica: uma revisão sistmática
|
Campos KK, Guckert SB, Gonçalves L F, Paiva KM, Stefani FM,
Haas P.
|
2022 |
| 10 |
Comorbidade entre depressão,
ansiedade e obesidade e complicações no tratamento
|
Casselli DN, Silva ESM, Figueira
GM, Demarch ME, Souza JC.
|
2021 |
| 11 |
Avaliação de imagem corporal em obesos no contexto cirúrgico de
redução de peso: revisão sistemática
|
Castro, Thiago Gomes de; Pinhatti, Marcelle Matiazo; Rodrigues,
Rodrigo Machado.
|
2017 |
| 12 |
Funcionamento interpessoal e
insatisfação com a imagem corporal em pacientes encaminhados
para cirurgia estética no SNS: Um papel mediador entre a
regulação emocional e o perfeccionismo?
|
Couper, SL; Moulton, SJ; Hogg,
FJ.
|
2021 |
| 13 |
Representações sociais do sobrepeso e da obesidade: Revisão
Sistemática
|
Couss A. |
2021 |
| 14 |
Um nuevo instrumento de evaluación
de resultados desde la perspectiva del paciente en cirugía del
contorno corporal estética y post bariátrica
|
Danilla E, S., Cuevas T, P. ,
Domínguez C, C., Jara C, R., Ríos V, M., Calderón G, M.,
Sepúlveda P, S.
|
2015 |
| 15 |
Body Contouring Surgery Improves Weight Loss after Bariatric
Surgery: A Systematic Review and Meta-Analysis
|
ElAbd R, Samargandi OA, AlGhanim K, Alhamad S, Almazeedi S,
Williams J.
|
2021 |
| 16 |
Quality of Life and Complications
in the Morbidly Obese Patient following Post-Bariatric Body
Contouring
|
Elfanagely O, Othman S, Mellia JA,
Messa CA, Fischer J P.
|
2021 |
| 17 |
Tornando-se ex-obeso: narrações sobre mudanças de identidade
antes e depois da experiência da cirurgia bariátrica
|
Faccio, E., Nardin, A. e Cipolletta, S. |
2016 |
| Nº |
Title |
Author |
Year |
| 18 |
O
psicólogo com o bisturi na mão: um estudo antropológico da
cirurgia plástica
|
Feriani D. |
2014 |
| 19 |
Aplicación del protocolo unificado
para el tratamiento transdiagnóstico de los trastornos
emocionales en pacientes post-cirugía bariátrica: estudio de
efectividad y viabilidad en formato grupal
|
Ferreres-Galán V, Quilez-Orden AB,
Osma J.
|
2022 |
| 20 |
Psychological distress among bariatric surgery candidates: The
roles of body image and emotional eating
|
Geller S, Levy S, Goldzweig G, Hamdan S, Manor A, Dahan S. |
2019 |
| 21 |
Quality of life among adults
following bariatric and body contouring surgery: a systematic
review
|
Gilmartin J, Bath-Hextall F,
Maclean J, Stanton W, Soldin M.
|
2016 |
| 22 |
Desaparecimento e novo desaparecimento: conviver com excesso de
pele e alterações intestinais após cirurgia para perda de
peso
|
Groven, KS, Råheim, M. e Engelsrud, G. |
2013 |
| 23 |
Contorno Corporal
Pós-Bariátrico
|
Herman, CK, Hoschander, AS e Wong,
A.
|
2015 |
| 24 |
The complexity of body image following bariatric surgery: a
systematic review of the literature: Bariatric surgery and body
image. Obesity Reviews
|
Ivezaj V, Grilo CM. |
2018 |
| 25 |
A systematic review of body
contouring surgery in post-bariatric patients to determine its
prevalence, effects on quality of life, desire, and
barriers
|
Jiang Z, Zhang G, Huang J, Shen C,
Cai Z, Yin X.
|
2021 |
| 26 |
Psychological Aspects of Bariatric Surgery as a Treatment for
Obesity
|
Jumbe S, Hamlet C, Meyrick J. |
2017 |
| 27 |
Avaliando resultados no contorno
corporal
|
Klassen, A F, Cano, SJ, Scott, A.,
Tsangaris, E., & Pusic, AL.
|
2014 |
| 28 |
The Impact of Bariatric Surgery on Psychological Health |
Kubik J F, Gill RS, Laffin M, Karmali S. |
2013 |
| 29 |
A Longitudinal Analysis of
Variation in Psychological Well-being and Body Image in Patients
Before and After Bariatric Surgery
|
de Meireles AJ, Carlin AM, Bonham
AJ, Cassidy R, Ross R, Stricklen A.
|
2020 |
| 30 |
Body image dissatisfaction and depression in postbariatric
patients is associated with less weight loss and a desire for
body contouring surgery
|
Monpellier VM, Antoniou EE, Mulkens S, Janssen IMC, Van Der
Molen ABM, Jansen ATM.
|
2018 |
| 31 |
Body Contouring Surgery after
Massive Weight Loss: Excess Skin, Body Satisfaction, and
Qualification for Reimbursement in a Dutch Post–Bariatric
Surgery Population
|
Monpellier VM, Antoniou EE, Mulkens
S, Janssen IMC, Jansen ATM, Mink Van Der Molen AB.
|
2019 |
| 32 |
Preoperative Evaluation of the Body Contouring Patient |
Naghshineh N, Rubin J P. |
2014 |
| 33 |
Space perception, movement, and
insight: attuning to the space of everyday life after major
weight loss
|
Natvik E, Groven KS, Råheim M,
Gjengedal E, Gallagher S.
|
2019 |
| 34 |
The long-term effect of body contouring procedures on the
quality of life in morbidly obese patients after bariatric
surgery
|
Paul MA, Opyrchał J, Knakiewicz M, Jaremków P, Duda-Barcik Ł,
Ibrahim AMS.
|
2020 |
| Nº |
Title |
Author |
Year |
| 35 |
Depressive disorders in patients who seek cosmetic surgery: a
broad and updated view
|
Paula PRD, Freitas-Júnior R, Prado M, Neves CGL, Arruda FCFD,
Vargas VEB
|
2016 |
| 36 |
Psychological and Psychiatric
Traits in Post-bariatric Patients Asking for Body-Contouring
Surgery
|
Pavan C, Marini M, De Antoni E,
Scarpa C, Brambullo T, Bassetto F.
|
2017 |
| 37 |
Patient-Reported Outcome Measures |
Poulsen L, McEvenue G, Klassen A, Hoogbergen M, Sorensen JA,
Pusic A.
|
2019 |
| 38 |
Evolution of the body image
perception of people with obesity on the pathway from bariatric
surgery to body contouring lift surgery
|
Proczko M, Postrożny D, Szymański
M, Pouwels S, Major P, Stepaniak P.
|
2022 |
| 39 |
Quality of life and predictive factors for complications in
patients undergoing abdominoplasty after gastric bypass: A
retrospective cohort. Surgery for Obesity and Related
Diseases
|
Rosa SC, Macedo JLSD, Canedo LR, Casulari LA. |
2019 |
| 40 |
Anthropometric and clinical
profiles of post-bariatric patients submitted to procedures in
plastic surgery
|
Rosa SC, Macedo JLSD, Casulari LA,
Canedo LR, Marques JVA.
|
2018 |
| 41 |
Body Image and Body Contouring Procedures |
Sarwer DB, Polonsky HM. |
2016 |
| 42 |
Access to reconstructive plastic
surgery for patients undergoing bariatric surgery in the unified
health system
|
Secanho Ms, Cintra Jr W, Carneiro
Ic, Alves Gff, Gemperli R.
|
2023 |
| 43 |
O
corpo (im)possível através da intervenção cirúrgica: uma revisão
sobre imagem corporal, obesidade e cirurgia bariátrica
|
Schakarowski FB, de Oliveira VZ. |
2014 |
| 44 |
Strategies for early detection of
psychopathologies in candidates for post-bariatric plastic
surgery
|
Silva DNE, Rosseto M, Vargas KFM,
Rezende AABM, Balbino EG, Andrade TRD.
|
2020 |
| 45 |
Educação em Saúde em Grupo no Tratamento de Obesos Grau III: um
Desafio para os Profissionais de Saúde
|
Soeiro RL, Valente GSC, Cortez EA, Mesquita LM, Xavier SCDM,
Lobo BMIDS.
|
2019 |
| 46 |
Does Body Contouring After
Bariatric Weight Loss Enhance Quality of Life? A Systematic
Review of QOL Studies
|
Toma T, Harling L, Athanasiou T,
Darzi A, Ashrafian H.
|
2018 |
| 47 |
Mais do que apenas peso corporal: o papel da imagem corporal no
funcionamento psicológico e físico
|
Wilson, RE, Latner, JD e Hayashi, K. |
2013 |
| 48 |
Preditores psicológicos de saúde
mental e qualidade de vida relacionada à saúde após cirurgia
bariátrica: uma revisão de pesquisas recentes
|
Wimmelmann, CL, Dela, F., &
Mortensen, EL.
|
2014 |
Chart 1. - Articles included in the bibliographic survey and mentioned in this
article.
DISCUSSION
The obesity treatment journey is complex and, throughout this process, the person
may face clinical comorbidities, social stigmas, and negative self-judgment,
which can affect their psychological state. Although the literature suggests a
correlation between obesity and psychiatric disorders, research does not
establish a direct connection between obesity, depression, and anxiety.
Considering the controversy, for Casselli et al.3 What can be inferred is that the presence of these disorders can
potentially increase the risk of obesity.
As obesity becomes a growing public health concern, bariatric surgery is gaining
prominence on a global scale. This procedure provides benefits that go beyond
the clinical scope, encompassing significant psychosocial advances, improved
well-being, and a more positive view of body image. However, deMeireles et
al.6 highlight a concern related to
bariatric surgery and mental health, as some preoperative psychological
assessments may be incipient. This means that psychological assessment is a
complex process that employs a variety of techniques, methods, and instruments
to collect information about a person’s psychological state. However, if the
psychologist does not collect sufficient data or apply appropriate techniques,
the depth and effectiveness of the assessment may be compromised.
An important aspect to be considered is that some patients do not follow the
recommendation to continue psychotherapy after the procedure, as advised by the
psychologist responsible for the psychological report or even by the bariatric
surgeon. In addition to the process of adapting to bariatric surgery,
interruption of psychological support can worsen the patient’s mental state.
Despite its many benefits, some studies, such as those by Poulsen et al.10 and Natvik et al.7 emphasize that the results of bariatric surgery lead to
significant weight loss, which can result in an unsatisfactory adaptation to the
new, slimmer body and discomfort due to excess skin. Monpellier et al.11 emphasize that plastic surgery is the
procedure capable of removing excess skin after massive weight loss and that
patients looking for solutions to this problem may experience psychological
suffering. Second Silva et al.9, research
has indicated that 60% of people who seek plastic surgery after bariatric
surgery have some psychological condition. Among the most common changes in this
group, depression, generalized anxiety disorder, and body dysmorphic disorder
stand out.
Considering the challenges faced in the treatment of obesity, as well as the
consequences and the adaptation process after bariatric surgery, added to the
discomfort caused by excess skin, there may be times when the patient is not
ready to undergo plastic surgery. In these cases, it is essential to refer you
for specialized mental health evaluation or treatment.
Pre-operative psychological assessment should be a fundamental element in the
initial consultation for patients seeking plastic surgery. Silva et al.9 and Ferreres-Galán et al.12 emphasize that the assessment aims to
identify psychological disorders, such as depression, anxiety, impulsivity,
binge eating, low self-esteem, and dissatisfaction with body image. A careful
investigation during medical screening is necessary, as some patients adopt an
attractive and seductive posture, influencing the course of the consultation and
the development of the surgical plan. It may happen in some cases that the
patient hides their complaints and minimizes their expectations to have their
surgery approved. Psychological assessment can prevent significant postoperative
losses.
The plastic surgeon must be prepared to conduct an initial psychological
screening of the patient. To do this, he/she can use validated psychometric
instruments that are widely applicable to health professionals from various
areas, in addition to semi-structured interviews. Attentive listening skills are
important so that the surgeon can identify signs of distress that the patient
may not have expressed explicitly. If the doctor identifies or suspects any sign
of mental disorder during the patient’s admission consultation, the recommended
course of action is to refer the patient for further evaluation with
specialists.
In psychological screening, the plastic surgeon can investigate factors that help
to understand the patient’s motivation for plastic surgery. This is important as
it can reveal possible psychological problems, especially when the motivation is
predominantly external. Motivation can be divided into intrinsic factors, such
as the desire for health, well-being, and resumption of social and work
activities, and extrinsic factors, such as pleasing others or obtaining social
benefits. Although both factors are important, the intrinsic factors, which are
linked to health and quality of life, should be more significant for the
patient.
Another aspect to be explored are social beliefs that often lead patients to seek
bodily perfection, feeding the idea that a slender body solves all problems.
Akkayaoğlu & Çelik2 point out that
studies on the concept of ego have focused on body image, which represents the
physical aspect of the ego. This relationship between the ego and self-image is
important for understanding how psychological factors can influence people’s
health and well-being. In some cases, the idealized body image appears as a way
to alleviate anguish and dissatisfaction. Complementing this view, Elfanagely et
al.13 and Bennett et al.14 highlighted the importance of
investigating patients’ expectations before and after surgery, making them aware
of the general changes that may occur after surgery.
In this context, it is important to inform the patient about the procedure,
establish realistic expectations for the recovery period, and warn about
possible complications, according to Bianciardi et al.15 Such measures can significantly contribute to reducing
patient anxiety, in addition to enhancing treatment adherence and optimizing
postoperative results. After all, a well-informed and mentally prepared patient
becomes a more active patient in their own recovery process.
Emotional support for the patient, both before and after surgery, is also
effective in managing the stress and anxiety associated with the procedure.
Additionally, collaboration with other healthcare professionals, such as
psychologists, nutritionists, and physical therapists, can be effective in
addressing all of the patient’s concerns. Another important aspect to be
discussed with the patient is the clear definition of their goals and
priorities, in addition to emphasizing the replacement of sagging skin with
scars.
This information can help the patient establish realistic expectations and
prepare more effectively for the recovery process after surgery. Psychological
screening conducted by the plastic surgeon can help identify people who are less
likely to benefit from surgery, as well as those who may need extra attention
and guidance, as highlighted by Buer et al.16 It is worth remembering that patients with body dysmorphia
regularly seek aesthetic procedures and, after carrying out these, tend to feel
dissatisfied with the results. According to Silva et al.9, in some circumstances, the patient may develop a
distorted perception of the outcome of surgery due to mental disorders. This, in
turn, can lead to legal action against the plastic surgeon, even when the
surgery achieved the planned objective and followed all established technical
criteria.
However, this study demonstrated that excess post-bariatric skin can result in
psychological distress. However, it is important to highlight that the obese
patient’s journey to the body contouring procedure is permeated by numerous
challenges, which, in a way, can also lead to mental health problems.
Thus, plastic surgery after bariatric surgery can help the patient control their
weight. Additionally, surgery has the potential to improve body image, which
can, in turn, restore or increase a person’s self-esteem and confidence. Jiang
et al.17 point out that in their
research, a significant improvement in these aspects was observed in patients
who underwent plastic surgery after bariatric surgery, especially when compared
to those who did not undergo the procedure.
Therefore, psychological research must be considered relevant and cannot be
relegated to a secondary level. Ignoring it would be contradictory to the
understanding that obesity is a disease with biopsychosocial causes and impacts.
Appropriate treatment must adopt an interdisciplinary approach, considering not
only the physical symptoms but also the psychological and social aspects
involved. This perspective is supported by studies, such as that of ElAbd et
al.18
This scoping review has a limitation: the lack of assessment of the
methodological quality of the selected articles.
CONCLUSION
The findings of this scoping review highlight the importance of incorporating
mental health assessment as a routine component in the preoperative assessment
in post-bariatric plastic surgery, as basic psychological assessment has the
potential to identify signs and symptoms of psychological distress that, If
detected early, they can prevent mental health complications, making it easier
to refer the patient to specialized mental health treatment. When the patient is
in an appropriate psychological state, they are better positioned to fully
benefit from the benefits of surgery. Furthermore, it is important that the
plastic surgeon, in addition to having extensive clinical-surgical technical
knowledge, also has a basic understanding of mental disorders.
REFERENCES
1. Proczko M, Postrożny D, Szymański M, Pouwels S, Major P, Stepaniak
P. Evolution of the body image perception of people with obesity on the pathway
from bariatric surgery to body contouring lift surgery. J Plast Reconstr Aesthet
Surg. 2022;75(2):860-9.
2. Akkayaoğlu H, Çelik S. Eating attitudes, perceptions of body image
and patient quality of life before and after bariatric surgery. Appl Nurs Res.
2020;53:151270.
3. Casselli DDN, Silva ESM, Figueira GM, Demarchi ME, Souza JC.
Comorbidade entre depressão, ansiedade e obesidade e complicações no tratamento.
Res Soc Dev. 2021;10(1):e16210111489.
4. Geller S, Levy S, Goldzweig G, Hamdan S, Manor A, Dahan S, et al.
Psychological distress among bariatric surgery candidates: The roles of body
image and emotional eating. Clin Obes. 2019;9(2):e12298.
5. Soeiro RL, Valente GSC, Cortez EA, Mesquita LM, Xavier SCM, Lobo
BMIS. Educação em Saúde em Grupo no Tratamento de Obesos Grau III: um Desafio
para os Profissionais de Saúde. Rev Bras Educ Médica. 2019;43(1 suppl
1):681-91.
6. deMeireles AJ, Carlin AM, Bonham AJ, Cassidy R, Ross R, Stricklen A,
et al. A Longitudinal Analysis of Variation in Psychological Well-being and Body
Image in Patients Before and After Bariatric Surgery. Ann Surg.
2020;271(5):885-90.
7. Natvik E, Groven KS, Råheim M, Gjengedal E, Gallagher S. Space
perception, movement, and insight: attuning to the space of everyday life after
major weight loss. Physiother Theory Pract. 2019;35(2):101-8.
8. Rosa SC, Macedo JLS, Canedo LR, Casulari LA. Quality of life and
predictive factors for complications in patients undergoing abdominoplasty after
gastric bypass: A retrospective cohort. Surg Obes Relat Dis.
2019;15(3):447-55.
9. Silva DNE, Rosseto M, Vargas KFM, Rezende AABM, Balbino EG, Andrade
TR, et al. Strategies for early detection of psychopathologies in candidates for
post-bariatric plastic surgery. Rev Bras Cir Plást.
2020;35(1):101-8.
10. Poulsen L, McEvenue G, Klassen A, Hoogbergen M, Sorensen JA, Pusic
A. Patient-Reported Outcome Measures: BODY-Q. Clin Plast Surg.
2019;46(1):15-24.
11. Monpellier VM, Antoniou EE, Mulkens S, Janssen IMC, Jansen ATM, Mink
van der Molen AB. Body Contouring Surgery after Massive Weight Loss: Excess
Skin, Body Satisfaction, and Qualification for Reimbursement in a Dutch
Post-Bariatric Surgery Population. Plast Reconstr Surg.
2019;143(5):1353-60.
12. Ferreres-Galán V, Quilez-Orden AB, Osma J. Aplicación del protocolo
unificado para el tratamiento transdiagnóstico de los trastornos emocionales en
pacientes post-cirugía bariátrica: estudio de efectividad y viabilidad en
formato grupal. An Psicol. 2022;38(2):219-31.
13. Elfanagely O, Othman S, Mellia JA, Messa CA 4th, Fischer JP. Quality
of Life and Complications in the Morbidly Obese Patient following Post-Bariatric
Body Contouring. Aesthetic Plast Surg. 2021;45(3):1105-12.
14. Bennett BL, Grilo CM, Alperovich M, Ivezaj V. Body Image Concerns
and Associated Impairment Among Adults Seeking Body Contouring Following
Bariatric Surgery. Aesthet Surg J. 2022;42(3):275-82.
15. Bianciardi E, Lorenzo GD, Niolu C, Betrò S, Zerbin F, Gentileschi P,
et al. Body image dissatisfaction in individuals with obesity seeking bariatric
surgery: exploring the burden of new mediating factors. Riv Psichiatr.
2019;54(1):8-17.
16. Buer L, Kvalem IL, Bårdstu S, Mala T. Comparing Bariatric Surgery
Patients Who Desire, Have Undergone, or Have No Desire for Body Contouring
Surgery: a 5-Year Prospective Study of Body Image and Mental Health. Obes Surg.
2022;32(9):2952-9.
17. Jiang Z, Zhang G, Huang J, Shen C, Cai Z, Yin X, et al. A systematic
review of body contouring surgery in post-bariatric patients to determine its
prevalence, effects on quality of life, desire, and barriers. Obes Rev.
2021;22(5):e13201.
18. ElAbd R, Samargandi OA, AlGhanim K, Alhamad S, Almazeedi S, Williams
J, et al. Body Contouring Surgery Improves Weight Loss after Bariatric Surgery:
A Systematic Review and Meta-Analysis. Aesthetic Plast Surg.
2021;45(3):1064-75.
1. Universidade Federal de São Paulo, Mestrado
profissional em Ciência, Tecnologia e Gestão Aplicadas à Regeneração Tecidual,
São Paulo, S P, Brazil.
Corresponding author: Angelica Cardoso Martins Rua Poanópolis, 71,
Centro, Poá, S P, Brazil. CEP: 08562-300 E-mail:
angelica.martins@unifesp.br
Article received: March 24, 2024.
Article accepted: April 30, 2024.
Conflicts of interest: none.