INTRODUCTION
Burns are tissue injuries resulting from various sources capable of producing
heat1 and are a global public health
problem responsible for approximately 180,000 deaths/year in low- and
middle-income countries and considered the fifth cause of death in the
world2. In children, burns are
responsible for negative impacts due to their severity, management difficulties,
potential mortality, and physical and psychological consequences, both for the
victim and their family environment3.
They have different etiologies, including scalds, flames, electrical voltage,
acidic or basic chemicals, and ultraviolet radiation4, responsible for small burns, easily treated, or
high-grade injuries, with irreversible consequences5. The organism responds locally or systemically, the first
due to direct damage to the tissue, while the second results from indirect
damage, that is, several physiological mechanisms try to contain the injury6. The severity and degree of injuries are
directly related to the etiological agent, the intensity of the heat, the
location affected, and the exposure time7,8.
In childhood, burns are the second most common cause of accidents, the fifth
cause of non-fatal pediatric injuries2,9, and the third cause of
death9. More than 111 thousand
children are hospitalized due to accidents or unintentional injuries, such as
burns, which cause around 3.6 thousand deaths/year10 and represent approximately 6% of deaths among the age
groups from 0 to 14 years old11.
Younger children are more vulnerable to domestic accidents such as burns due to
less motor coordination caused by physical immaturity, heightened curiosity, and
greater dependence on parents and caregivers12. Males have an increased risk in all age groups, with 1.5 boys
for every girl suffering from burns, and 53.4% of boys, from the first year of
life, have twice the chance of suffering injuries13. This higher proportion may be associated with behavior and
cultural factors, which determine greater freedom for boys, who expose
themselves to risky games14,15.
In the United States of America (USA), burns are the fourth leading cause of
death from trauma3,16 and, in children under 16 years of age, according to the
National Burn Repository, hospitalizations account for 20%17. In Brazil, around 1 million people suffer accidents
involving burns and only 100,000 seek medical help after the incident18.
Financial costs vary depending on the extent of the injury, length of stay,
number of interventions, and treatment method19. Treating burns requires a great economic burden, according to
clinical and surgical management, which includes a trained multidisciplinary
team, and long hospitalization time, associated with procedures, medications,
and equipment20.
In the USA, the direct costs of caring for children suffering from burns are more
than US$211 million, between 3000 and 5000 dollars/day, and corresponds to
approximately 23% of the total cost of treatment2. In Brazil, approximately R$450 million was spent on
hospitalizations due to burns in the last decade21. However, there are not enough studies that evaluate details of
the cost of hospitalization of burn victims22. A study that analyzed 180 burn patients for 5,207 days estimated
that the direct daily treatment costs were US$1,330.48 and the total
hospitalization cost was US$39,594.9019.
Furthermore, burn survivors spend less than non-survivors and, between direct
and indirect costs, each patient costs US$88,21819,22.
In addition to the financial cost, burns have social costs from indirect causes
such as unemployment, prolonged care, emotional trauma, and family
assistance2. The stigma caused by
burns is considered an obstacle by patients, as it interferes with
self-perception and self-esteem and leads victims to feelings of
self-depreciation23. Approximately
half of burns occur in children and adolescents, which has individual and social
consequences24.
According to the World Health Organization, burn injuries are more frequent in
underdeveloped countries, given that there is more medical care among children
of lower socioeconomic status and that public policies, prevention measures
implemented by the government, and low social, economic, and cultural factors
are reasons for the higher prevalence in these locations2,24.
Therefore, knowing the temporal trend of hospitalizations for pediatric burns in
all Brazilian regions could contribute to the planning of public policies aimed
at preventing and reducing social and financial costs for hospital
admissions.
OBJECTIVE
Thus, the objective of the study was to investigate the temporal trend of
hospitalizations for pediatric burns, in the age group from 0 to 14 years, in
Brazil, between 2012 and 2022.
METHOD
This is an ecological time series study with information regarding hospital
admissions for pediatric burns in Brazil. The data were obtained from the public
domain website Hospital Information System of the Unified Health System
(SIH-SUS), available at the Information Technology Department of the Unified
Health System (DATASUS). Information about hospital admissions in the SUS is
stored based on data from the Hospital Admissions Authorization (AIH). The data
were exported in comma-separated values (CSV) format and saved in an Excel
spreadsheet to calculate the rates.
Population demographic information was collected on the website of the Brazilian
Institute of Geography and Statistics, using the 2000 and 2010 censuses, in
addition to their intercensal estimates. Data from 91,091 children of under 14
years of age, both sexes, residing in the Brazilian regions (North, Northeast,
South, Southeast, and Central-West), victims of burns (International Statistical
Classification of Diseases and Problems Related to Health T20-T32) between the
years 2012-2022. The variables analyzed were sex (male and female), age group
(< 1 year; 1 – 4 years; 5 – 9 years and 10 – 14 years), region (North,
Northeast, South, Southeast, and Central-West) and years analyzed
(2012-2022).
The variables used in the study that fall into the dependent category were:
general hospitalization rate, hospitalization rate by sex, age group rate by
sex, and region. The independent variable was the years used for the study.
For each year of the period under study, the rates of hospitalizations for burns
were calculated according to the dependent variables, for every 100,000
inhabitants based on the ratio between the total number of hospitalizations for
pediatric burns and the population referring to sex, age group/sex, and
regions.
To analyze the temporal trend study of hospitalizations for pediatric burns,
standardized coefficients and the method of simple linear regression, using the
Statistical Package for the Social Sciences (SPSS) version 20.0. In this method,
standardized hospitalization rates were considered dependent variables and the
years of the study period as an independent variable, obtaining a model
estimated according to the formula Y = b0 + b1X, where Y = standardized
coefficient, b0 = mean coefficient of the period, b1 = mean annual increment and
X = year. The analysis of behavior (increase, decrease, or stability) and the
mean annual variation in the hospitalization coefficient was carried out based
on the evaluation of the value of the regression coefficient (P). The
statistical significance considered was p≤0.05.
As it is a research with secondary data, in the public domain and free access,
following Resolution of the National Health Council (CNS) no. 466, of December
12, 2012, and under the guidelines and standards of Resolution 510 /2016 of the
National Health Council, Article 1, Sole Paragraph, Items II, III and V, there
was no need for approval by the Ethics and Research Committee.
RESULTS
Data from 91,091 hospital admissions due to burns in children aged 0 to 14 years,
in Brazil, between 2012 and 2022 were analyzed. There was a trend towards
stability in the general hospitalization rate in Brazil, with an initial rate of
18.51 and a final rate of 18.73 hospitalizations/100,000 inhabitants (mean rate
17.963; β = 0.119; p = 0.163).
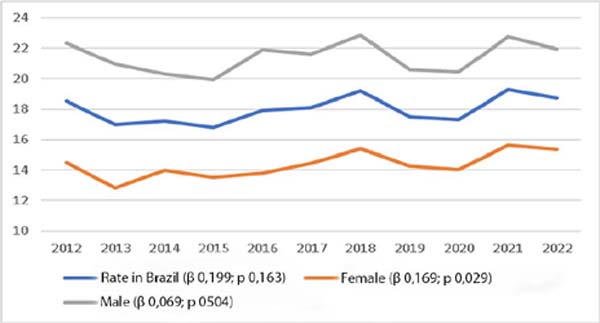
Concerning stratification by sex, the same stability behavior was observed in
males (mean rate of 21.42; β = 0.069; p =
0.504). The male hospitalization rate started at 22.33/100,000 inhabitants and,
at the end of the period, reduced to 21.95/100,000 inhabitants, resulting in a
1.7% reduction. In females, the behavior was an increase (mean rate 14.346;
β = 0.169; p = 0.029) in
hospitalizations/100,000 inhabitants, with an initial rate of 14.53, ending the
study period with 15.35/100,000 inhabitants, characterizing 5.5% increase (Table 1, Figure 1).
Table 1 - Temporal trend of hospitalizations due to burns, in the age group 0
-14 years, in 2012-2022, according to sex, age group, and
regions.
| Variables |
Mean Rate |
R (*) |
R2 (†) |
B (‡) |
95% CI |
p-value |
Trend |
| General Rate Sex |
17,963 |
0.451 |
0.204 |
0.119 |
(-0.580; 0.295) |
0.163 |
Stability |
| Masculine |
21,426 |
0.226 |
0.051 |
0.069 |
(-0.155; 0.293) |
0.504 |
Stability |
| Feminine |
14,346 |
0.654 |
0.427 |
0.169 |
(0.021; 0.316) |
0.029 |
Increase |
| Female Age Group |
|
|
|
|
|
|
|
| 4
years
|
29,281 |
0.698 |
0.488 |
0.407 |
(0.093; 0.722) |
0.170 |
Stability |
| 5 - 9 years |
9,614 |
0.286 |
0.082 |
0.084 |
(-0.127; 0.294) |
0.393 |
Stability |
| 10
- 14 years
|
5,684 |
0.195 |
0.038 |
0.034 |
(-0.095; 0.163) |
0.565 |
Stability |
| Male Age Group |
|
|
|
|
|
|
|
| 4
years
|
42,264 |
0.798 |
0.637 |
0.613 |
(0.265; 0.962) |
0.003 |
Increase |
| 5 – 9 years |
14,189 |
0.057 |
0.003 |
-0.210 |
(-0.300; 0.257) |
0.867 |
Stability |
| 10
– 14 years
|
9,871 |
0.754 |
0.569 |
-0.328 |
(-0.543; -0.113) |
0.007 |
Reduction |
| Regions |
|
|
|
|
|
|
|
| South |
26,952 |
0.861 |
0.741 |
1,091 |
(0.605; 1.577) |
0.001 |
Increase |
| Southeast |
13,748 |
0.615 |
0.378 |
0.172 |
(0.006; 0.338) |
0.440 |
Stability |
| Midwest |
23,689 |
0.004 |
0.000 |
0.006 |
(-1.133; 1.146) |
0.990 |
Stability |
| North |
12,267 |
0.082 |
0.007 |
-0.022 |
(-0.226; 0.182) |
0.600 |
Stability |
| North East |
19,881 |
0.638 |
0.407 |
-0.291 |
(-0.557; -0.026) |
0.350 |
Stability |
Table 1 - Temporal trend of hospitalizations due to burns, in the age group 0
-14 years, in 2012-2022, according to sex, age group, and
regions.
Figure 1 - Temporal trend of hospitalization for burns in Brazil, in the age
group 0-14 years, between 2012 and 2022, according to general rate
and sex.
Figure 1 - Temporal trend of hospitalization for burns in Brazil, in the age
group 0-14 years, between 2012 and 2022, according to general rate
and sex.
Table 1 presents the mean rate, the
coefficient of determination (R2), the mean annual variation (P), the value of
p, and the trend stratified by sex, age group, and region.
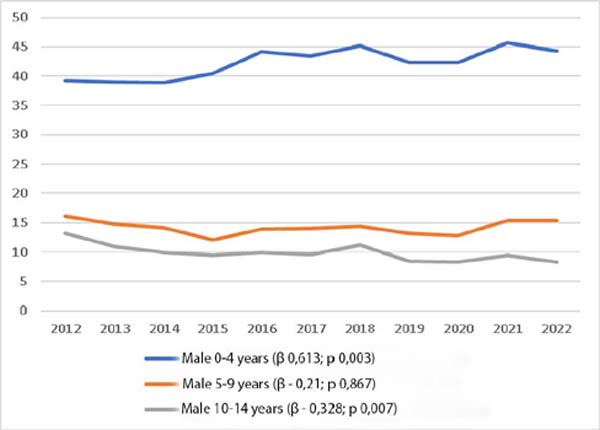
When analyzing the male age group, there was a tendency for an increase in
hospitalizations in the age group of 0 to 4 years (mean rate 42.264;
β = 0.613; p = 0.003), with an initial
rate of 39.23 and a final rate of 44.31, representing an increase of 13%. In the
age groups of 5 to 9 years and 10 to 14 years, there was stability (mean rate
14.189; β = -0.21; p = 0.867) and reduction
(mean rate 9.871; β = -0.328; p = 0.007) in
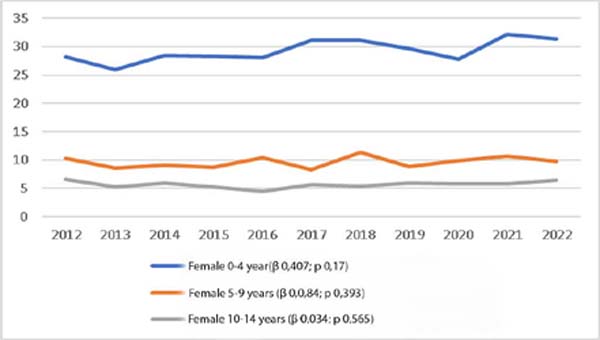
hospitalizations per 100,000 inhabitants, respectively (Table 1; Figure 2). In
the age groups by female sex, there was a stable trend in all age groups. In the
age group 0-4 years, there was an increase of 11.5%, with an initial rate of
28.14 and a final rate of 31.38 hospitalizations/100,000 inhabitants, with
stable behavior (Table 1; Figure 3).
Figure 2 - Temporal trend of hospitalization for burns in Brazil, among
males, according to age group.
Figure 2 - Temporal trend of hospitalization for burns in Brazil, among
males, according to age group.
Figure 3 - Temporal trend of hospitalization for burns in Brazil, among
females, according to age group.
Figure 3 - Temporal trend of hospitalization for burns in Brazil, among
females, according to age group.
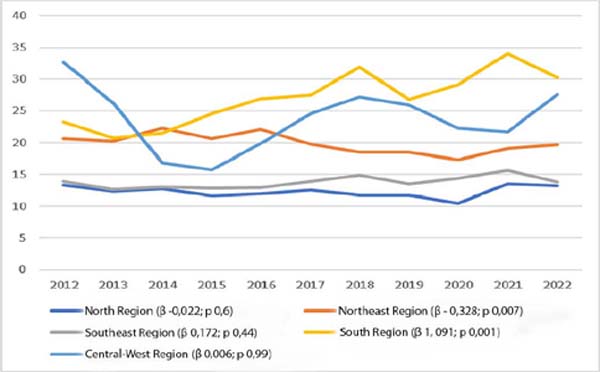
Regarding hospitalizations by region, an increase was observed in the South
Region (mean rate of 23.952; β = 1.091; p =
0.001), with 23.28 hospitalizations/100,000 inhabitants in the initial period of
the study and 30.21/100,000 inhabitants in the final period, reflecting a 29.8%
increase. The other regions showed stability behavior: North Region (mean rate
12.267; β = -0.022; p = 0.600), Northeast
Region (mean rate 19.881; β = -0.291; p = 0.035), Southeast
Region (mean rate 13.748; β = 0.172; p = 0.44)
and Central-West Region (mean rate 23.689; β = 0.006;
p = 0.99). The Central-West Region had the highest mean
rate of hospitalizations per 100,000 inhabitants at the beginning of the studied
period, with a value of 32.68/100,000 inhabitants.
The lowest mean rate of hospitalizations per 100,000 inhabitants, in the initial
period of the study, was obtained by the North Region, with a value of
13.29/100,000 inhabitants. At the end of the study period, except for the South
Region, which showed an increase in the mean hospitalization rate per 100,000
inhabitants, all regions behaved similarly with stability in mean
hospitalization rates (Table 1, Figure 4).
Figure 4 - Temporal trend in the hospitalization rate for burns in Brazil,
in the age group 0-14 years, between 2012 and 2022, according to
regions.
Figure 4 - Temporal trend in the hospitalization rate for burns in Brazil,
in the age group 0-14 years, between 2012 and 2022, according to
regions.
DISCUSSION
Studies on pediatric hospitalizations in the age group 0-14 years by region in
Brazil are scarce. The study under discussion verified a temporal trend of
stability in hospitalizations for pediatric burns in Brazil during the analyzed
period. On the other hand, a study of hospital admissions in Brazil in children
under 14 years of age, between 2008 and 2015, showed a downward trend in
hospitalizations25, with a reduction
of 28.14% for males and 22.2% for females, demonstrating behavior that diverges
from the current study.
The stability trend found in the present study can be explained by the adoption
of prevention measures such as the National Policy for Reducing Morbidity and
Mortality from Accidents and Violence (2001), the ban on the sale of liquid
alcohol to the general population (2002) and the creation of Accident and
Violence Prevention Centers in the Unified Health System (2004)25,26. Together, such actions receive support for the promotion of safe
and healthy behaviors and environments25,
supporting stability and a possible decrease in the trend of hospitalizations
over the years.
When analyzing the hospitalization rate for males, a stable behavior was observed
during the period studied, which differs from the literature, which shows an
increase in hospitalizations for males, with 61.4% of hospitalizations due to
burns in the age group of 0-14 years in the regions of Brazil in males between
2008-201525, as well as 69.4% of male
admissions to Burn Treatment Centers in children aged 7-12 years in the period
2011-201418. The observed behavior
may be a reflection of educational measures25,26 associated with the
child’s learning about the notion of danger, in addition to gaining strength and
agility according to their psychomotor development27.
As for females, there was a tendency for the general rate to increase, with
statistically significant data. In the literature, similar behavior occurred
only in the South Region, with a 23.25% increase in hospitalizations due to
burns25. The increase in the rate of
female hospitalization can be associated with domestic accidents and domestic or
self-inflicted violence18, since, due to
the complex interaction between family habits, cultural norms, socioeconomic
environment, and secular behaviors16,
females are often more likely to collaborate with household chores, susceptible
to greater contact with potentially flammable chemical substances.
Both males and females showed increases in the general rate of hospitalizations
in 2021. This increase may be associated with the COVID-19 pandemic period,
which encouraged children to remain at home, in which childhood burns
predominantly occur17, as well as other
accidents, most of which are unintentional and avoidable28.
Furthermore, with the COVID-19 pandemic, in 2020, the sale of 70º GL ethyl
alcohol in one-liter packages29 was
authorized for the hygiene of hands, surfaces, and objects; the sale of alcohol
with a strength greater than 54º GL was prohibited since 200225. Alcohol, among flammable agents, was
the one that caused the most burns in Brazil10,25 and with the ban on its
sale, there was a considerable reduction in these accidents, however, the
resumption of sales increased incidence again8.
There was a tendency towards stability in all age groups among females. Among
males, there was an increasing trend in the age group of 0-4 years, with
statistically significant data. This increase in this age group corroborates the
literature, which shows that the highest rates occurred in preschool children
aged 1-4 years, with 57.05% of hospitalizations, and mostly in males, with an
incidence of 63.04%26.
The increase in male hospitalizations in the 0-4 age group may be related to
increased curiosity and intellectual and cognitive development not accompanied
by the motor development of children at this age25, associated with the greater freedom provided to them12,18. Pediatric burns are the second most frequent cause of accidents
and the third cause of death among 0-14 years old11.
Concerning hospitalizations by region, the South Region was the only one that
presented statistically significant data, demonstrating an increase in the rate
of hospitalizations for pediatric burns, with an increase of 29.8% in
hospitalizations during the study period. The other regions showed stable
behavior. Therefore, the present study is in line with a similar study that
demonstrated an increase in hospitalizations for pediatric burns in the South
Region, in both sexes (males p = 0.050; females p = 0.033)25.
This fact may be related to the increase in notifications and better access to
specialized services that include rigor in hospitalizations in the pediatric age
group and availability of beds in the Burn Treatment Unit (BTU) of Hospital
Infantil Joana de Gusmão (HIJG) in Florianópolis, which is the only pediatric
BTU in southern Brazil25,28. Furthermore, it is pertinent to
highlight that some regions, such as the North, have large territorial
extensions, which can make access between the population and hospital care
difficult, as well as there are no units specialized in highly complex
burns25.
Regarding limitations, as the data were collected from hospital admission records
available in DATASUS, underreporting of hospitalizations due to burns or
erroneous notifications in the system may have occurred. Furthermore, since
DATASUS presents information relating to the Unified Health System,
hospitalizations for pediatric burns that occurred in the private network were
not included in the study analysis.
This study contributed to the identification of the temporal trend in
hospitalization rates for burns in the period 2012-2022 in the regions of Brazil
in the age groups of 0-14 years through the analysis of age group, sex, and
regions. In the literature, there is only one temporal trend study on
hospitalizations for pediatric burns by region, hence the relevance of this
study, when comparing hospitalization rates for burns between Brazilian regions.
Furthermore, the data found can contribute to the development of public health
policies, aiming at prevention and care at secondary and tertiary levels for the
populations studied.
CONCLUSION
In the period 2012 to 2022, there were 91,091 hospitalizations due to burns in
children aged 0-14 years in Brazil. Most of these occurred in the male
population 60.97% (n = 55,539) and in the age group 0-4 years 62.33% (n =
56,778). During the period studied, there was a stable trend in hospital
admissions for burns in Brazil in the population aged 0-14 years in males and an
increase in females.
Females behaved with stability at all ages, while males showed an increase in the
0-4 age group, stability in the 5-9 age group, and a reduction in the 10-14 age
group.
The regions behaved with stability in hospital admissions for pediatric burns,
except for the South Region, which showed an increase.
REFERENCES
1. Souza LRP, Lima MFAB, Dias RO, Cardoso EG, Briere AL, Silva JO. O
tratamento de queimaduras: uma revisão bibliográfica. Braz J Develop.
2021;7(4):37061-74.
2. World Health Organization (WHO). Burns. Geneva: WHO; 2018 [Acesso em
01 set 2022]. Disponível em: https://www.who.int/news-room/fact-sheets/detail/burns.
3. Hernández CMC, Núñez V P, Suárez FAP, Banqueris R F, García MS,
Mendoza D P. Queimaduras e sua prevenção em crianças. Rev Bras Queimaduras.
2020;19(1):84-8.
4. Kartal S P, Bayramgurler D. Hot Topics in Burn Injuries. IntechOpen.
2018;128.
5. Fé DSM, Germino C, Mendonça IB, Manso MEG. Queimadura: Efeitos
psicossociais nas vítimas. In: IV Congresso Médico Universitário São Camilo;
2018 Out 08-09; São Paulo, Brasil. Blucher Medical Proceedings; 2018. p.
170-92.
6. Sociedade Brasileira de Queimaduras; Escola Superior de Ciências da
Saúde, Liga de Emergência e Trauma da ESCS. Manual de queimaduras para
estudantes. Brasília: Sociedade Brasileira de Queimaduras;
2021.
7. Mehrotra S, Misir A. Special Traumatized Populations: Burns
Injuries. Curr Pediatr Rev. 2018;14(1):64-9.
8. Rosa Z, Lima TH. Perfil epidemiológico de pacientes vítimas de
queimadura. Braz J Health Rev. 2021;4(5):19832-53.
9. Gurgel AKC, Monteiro AI. Prevenção de acidentes domésticos infantis:
susceptibilidade percebida pelas cuidadoras. J Res Fundam Care Online.
2016;8(4):5126-35.
10. Santos G P, Freitas NA, Bastos VD, Carvalho F F. Perfil
epidemiológico do adulto internado em um centro de referência em tratamento de
queimaduras. Rev Bras Queimaduras. 2017;16(2):81-6.
11. American Burn Association. National Burn Repository 2019 Update.
Report of data from 2009-2018. Chicago: American Burn Association;
2019.
12. https://bvsms.saude.gov.br/contra-queimaduras-prevencao-e-a-vacina-06-6-dia- nacional-de-luta-contra-queimaduras/
13. Barcellos LG, Silva APP, Piva J P, Rech L, Brondani TG.
Characteristics and outcome of burned children admitted to a pediatric intensive
care unit. Rev Bras Ter Intensiva. 2018;30(3):333-7.
14. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde;
Departamento de Análise em Saúde e Vigilância de Doenças Não Transmissíveis.
Viva Inquérito 2017: Vigilância de Violências e Acidentes em Serviços Sentinelas
de Urgência e Emergência - Capitais e Municípios. Brasília: Ministério da Saúde;
2019.
15. Sociedade Brasileira de Queimaduras (SBQ). Secretaria de Justiça e
Cidadania. Casa segura, criança protegida: prevenção de acidentes domésticos com
crianças e adolescentes. Brasília: Sociedade Brasileira de Queimaduras;
2021.
16. Blank D. Controle de injúrias sob a ótica da pediatria contextual. J
Pediatr (Rio J). 2005;81(5 Suppl):S123-36.
17. Francisconi MHG, Itakussu EY, Valenciano PJ, Fujisawa DS, Trelha CS.
Perfil epidemiológico das crianças com queimaduras hospitalizadas em um Centro
de Tratamento de Queimados. Rev Bras Queimaduras.
2016;15(3):137-41.
18. Daga H, Morais IH, Prestes MA. Perfil dos acidentes por queimaduras
em crianças atendidas no Hospital Universitário Evangélico de Curitiba. Rev Bras
Queimaduras. 2015;14(4):268-72.
19. Anami EHT, Zampar E F, Tanita MT, Cardoso LTQ, Matsuo T, Grion CMC.
Treatment costs of burn victims in a university hospital. Burns.
2017;43(2):350-6.
20. Oliveira APBS, Peripato LA. A cobertura ideal para tratamento em
paciente queimado: uma revisão integrativa da literatura. Rev Bras Queimaduras.
2017;16(3):188-93.
21. Vieira VLM, Aquino DW, Siqueira L F, Silva JVS, Zanatta TG, Bender
CL, et al. A Média de permanência hospitalar por queimaduras e sua relação com
as despesas hospitalares no Brasil: uma análise epidemiológica da última década.
Rev Bras Queimaduras. 2021;20(Suppl 1):6.
22. Saavedra PAE. Perfil epidemiológico e estimativas de custos
hospitalares de vítimas de queimaduras [Tese de doutorado]. Brasília:
Universidade de Brasília Faculdade de Ceilândia; 2021. 149 p.
23. Emerick MFB, Batista KT. Principle of non-discrimination and
non-stigmatization: considerations for improving the quality of life of people
with burn sequelae. Rev Bras Cir Plást. 2022;37(2):218-27.
24. Correia DS, Chagas RRS, Costa JG, Oliveira JR, França NPA, Taveira
MGMM. Perfil de crianças e adolescentes internados no centro de terapia de
queimados. Rev Enferm UFPE On Line. 2019;13(5):1361-9.
25. Pereima MJL, Vendramin RR, Cicogna JR, Feijó R. Internações
hospitalares por queimaduras em pacientes pediátricos no Brasil: tendência
temporal de 2008 a 2015. Rev Bras Queimaduras.
2019;18(2):113-9.
26. Souza TG, Souza KMD. Série temporal das internações hospitalares por
queimaduras em pacientes pediátricos na Região Sul do Brasil no período de 2016
a 2020. Rev Bras Cir Plást. 2022;37(4):438-44.
27. Carvalho B F. Análise dos óbitos de crianças internadas por
queimaduras no Hospital Infantil Joana de Gusmão no período de janeiro de 1991 a
março de 2019 [Trabalho de conclusão de curso]. Florianópolis: Universidade
Federal de Santa Catarina; 2019.
28. Favassa MT, Vietta GG, Nazário NO. Tendência temporal de internação
por queimadura no Sul do Brasil. Rev Bras Queimaduras.
2017;16(3):163-8.
29. http://tiny.cc/ anvisanotatecnica
1. Universidade do Sul de Santa Catarina (UNISUL),
Campus Pedra Branca, Medicina, Palhoça, SC, Brazil
Corresponding author: Luzieli
Portaluppi Universidade do Sul de Santa Catarina (UNISUL), Campus
Pedra Branca Av. Pedra Branca, 25, Palhoça, SC, Brazil. CEP: 88137-270 E-mail:
luzieliportaluppi@gmail.com
Article received: November 23, 2023.
Article accepted: April 30, 2024.
Conflicts of interest: none.