INTRODUCTION
In 1947, Pickrell et al. used the pectoralis major muscle to reconstruct a
post-mastectomy chest wall defect1. However, it was only in 1977 that McCraw et al.2,3 carried out anatomical studies that enabled its use as a
myocutaneous flap. The accumulated experience in using the flap and greater
knowledge of its anatomy led to the transfer of increasingly larger skin
segments4. The pedicle,
which initially included the skin, now consists only of muscles and
thoracoacromial vessels in the proximal part. This allowed the use of island
flap5.
In 2019, Rauchenwald et al.6
published a retrospective study with 23 patients who underwent reconstruction
with a pectoralis major island myocutaneous flap for fistula prophylaxis after
rescue laryngectomy, demonstrating great evolution in the operative technique
and its indications.
On the other hand, the idea of combining mammaplasty techniques to access the
myocutaneous flap of the pectoralis major muscle to cover chest wall defects
began to be described in 1996 by some authors such as de Fontaine et
al.7 and
Griffin8. In 2023,
Boodhun & Zinn9 also used
the myocutaneous flap of the pectoralis major muscle in association with
reduction mammaplasty to cover a defect in the anterior cervical region.
In the present article, we describe the case of a male patient who underwent
reconstruction of a large defect of the anterior chest wall using the islanded
myocutaneous flap of the pectoralis major muscle in association with mammoplasty
techniques.
Research Ethics Committee (CEP) and conflict of interests
The research project of this article follows the CEP of Hospital Governador
Celso Ramos, in Florianópolis-SC, and was approved under opinion number
6,305,043.
The authors declare that they have no conflict of interest.
CASE REPORT
AES, 66 years old, male, attended the Hospital Governador Celso Ramos, in
Florianópolis, SC, and presented with a skin tumor that had evolved over
approximately 10 years in the right parasternal region. During this period, he
had already undergone several cryotherapy sessions and four resections of the
same tumor in other Services. A biopsy of the lesion revealed the diagnosis of
infiltrative basal cell carcinoma.
On physical examination, the skin tumor affected the region corresponding to the
medial portion of the right clavicle, running inferiorly and parallel to the
right of the sternum. The tumor measured 13.0cm on its longest vertical axis
and
8.0cm on its longest horizontal axis. The patient also had skin retraction in
the anterior region of the neck (Figure 1).
However, there was no cervical lymph node enlargement.
Figure 1 - Extensive infiltrative and recurrent basal cell carcinoma in the
parasternal region on the right.
Figure 1 - Extensive infiltrative and recurrent basal cell carcinoma in the
parasternal region on the right.
Surgical technique
Scheduling tumor resection
The marking of the tumor piece to be resected was carried out with
lateral safety margins of 2.0cm (Figure 2). The resulting wound exposed the medial portion of the
right clavicle and the ipsilateral pectoralis major muscle (Figure 3).
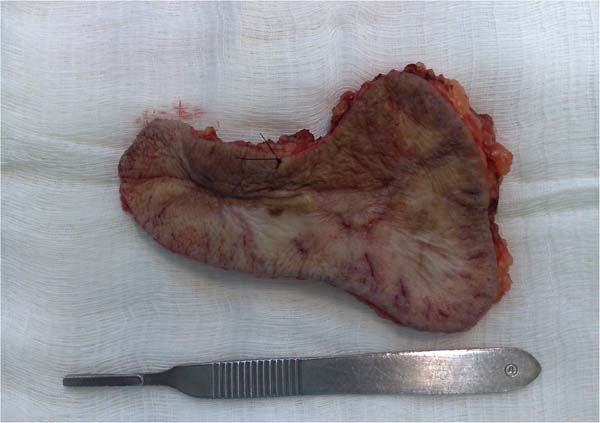
Figure 2 - A surgical specimen sent for pathological
examination.
Figure 2 - A surgical specimen sent for pathological
examination.
Figure 3 - Extensive surgical wound resulting from wide resection of
the tumor.
Figure 3 - Extensive surgical wound resulting from wide resection of
the tumor.
Marking the flap donor area
It was performed with the patient in an upright position. Point A of the
breast was defined and from there, a periareolar semicircle was drawn,
keeping the papilla in its center. The semicircle was completed at
points defined as B and C, 1.0cm from the lower limit of the areola.
The skin island of the myocutaneous flap corresponded to the medial
triangular area of the breast that would normally be resected and
discarded in a reduction mammaplasty (Figure 4).
Figure 4 - Myocutaneous island flap of the pectoralis major
muscle.
Figure 4 - Myocutaneous island flap of the pectoralis major
muscle.
Surgical description
Wide resection of the tumor was performed with the patient in the supine
position and under general anesthesia.
The skin of the right breast was infiltrated with a solution containing
200ml of 0.9% SF, 40ml of 2% xylocaine without vasoconstrictor, and 1ml
of adrenaline.
The Schwarzmann10
maneuver was performed and the medial triangle of skin and fat was
sectioned. Subcutaneous detachment of the right pectoral region was
performed, exposing the entire anterior surface of the pectoralis major
muscle up to its origin. Afterwards, its insertions on the costal arches
and sternum were sectioned and its posterior surface was also detached
to its origin. In this way, the myocutaneous flap was completely
released, allowing its subcutaneous rotation and coverage of the defect
in the right parasternal region (Figures 4 and 5).
Figure 5 - Transposition of the pectoral flap.
Figure 5 - Transposition of the pectoral flap.
After the small rise of the nipple-areola complex (NAC), the male breast
is sutured in layers. A lateral triangle of skin and fat was resected to
adjust the inverted T mammaplasty scar11,12. In the detachment area, a 4.8 suction drain was
left (Figure 6)13.
Figure 6 - Final aspect of mammaplasty and reconstruction of the
pectoral defect.
Figure 6 - Final aspect of mammaplasty and reconstruction of the
pectoral defect.
Postoperatively, the drain was removed after 7 days and there were no
complications13. The pathological examination confirmed the
diagnosis of infiltrative basal cell carcinoma and surgical margins free
of neoplasia. The patient underwent outpatient follow-up and did not
experience any further tumor recurrence (Figure 7).
Figure 7 - Three months postoperatively.
Figure 7 - Three months postoperatively.
DISCUSSION
Although skin grafting was a simpler treatment option, in this case, this
technique had some disadvantages. The majority of the defect bed was made up
of
the muscle belly, which favored the integration of the skin graft, but there
were other areas of exposed bone (clavicle) and subcutaneous cellular tissue.
There would also be greater morbidity in the skin donor area. Furthermore, the
thickness and texture of the graft skin would be different from that found in
the pectoral region.
Some local skin flaps could be planned, but they would result in large visible
scars14. In the case
of other pedicled myocutaneous flaps, there would be the latissimus dorsi and
rectus abdominis alternatives. However, they would result in more scars, longer
surgical time, and greater postoperative morbidity.
In turn, free cutaneous flaps based on the deep or superficial epigastric artery
would be good alternatives for covering the thoracic defect. However, the
patient was obese and had a bulky and protruding abdominal apron. Therefore,
dissection of the lower abdominal region would be difficult to perform and also
pose a greater chance of local postoperative complications.
On the other hand, the simplicity and low morbidity of the myocutaneous pectoral
island flap motivated its choice. Detachment of the pectoralis major muscle in
its anterior and posterior planes was simple to perform. The pivot point of
subcutaneous transposition of the skin island was the acromion and the thoracic
defect was within its arc of rotation. To repair the flap donor area,
mammaplasty techniques were used to avoid scars in unfavorable locations or
causing any unacceptable asymmetry.
Although the inverted T scar could produce the stigma of female mammaplasty, in
this case, this did not occur. As the patient had grade 4 gynecomastia and the
mammoplasty was not intended to treat this condition, the final scars on the
flap’s donor breast were not as prominent.
CONCLUSION
With the association of pectoral myocutaneous flap techniques and the closure of
the flap donor area in the form of an inverted T mammaplasty, it was possible
to
obtain a satisfactory aesthetic and functional result, in a single surgical
procedure and with low morbidity.
This surgical tactic is a simple alternative for the treatment of defects located
in the arc of rotation of the pectoralis major flap when performed by surgeons
accustomed to breast reconstruction.
| COLLABORATIONS |
| FBW |
Final manuscript approval, Realization
of operations and/or trials, Writing - Original Draft
Preparation.
|
| VE |
Final manuscript approval,
Supervision.
|
REFERENCES
1. Pickrell KL, Baker HM, Collins JP. Reconstructive surgery of the
chest wall. Surg Gynecol Obstet. 1947;84(4):465-76.
2. McCraw JB, Dibbell DG, Carraway JH. Clinical definition of
independent myocutaneous vascular territories. Plast Reconstr Surg.
1977;60(3):341-52.
3. McCraw JB, Dibbell DG. Experimental definition of independent
myocutaneous vascular territories. Plast Reconstr Surg.
1977;60(2):212-20.
4. Freeman JL, Walker EP, Wilson JS, Shaw HJ. The vascular anatomy of
the pectoralis major myocutaneous flap. Br J Plast Surg.
1981;34(1):3-10.
5. Wei WI, Lam KH, Wong J. The true pectoralis major myocutaneous
island flap: an anatomical study. Br J Plast Surg.
1984;37(4):568-73.
6. Rauchenwald T, Dejaco D, Morandi EM, Djedovic G, Wolfram D,
Riechelmann H, et al. The Pectoralis Major Island Flap: Short Scar Modified
Muscle-Sparing Harvesting Technique Improves Aesthetic Outcome in Reconstructive
Head and Neck Surgery. ORL J Otorhinolaryngol Relat Spec. 2019;81(5-6):327-37.
DOI: 10.1159/000503008
7. de Fontaine S, Devos S, Goldschmidt D. Reduction mammaplasty
combined with pectoralis major muscle flaps for median sternotomy wound closure.
Brit J Plast Surg. 1996;49(4):220-2.
8. Griffin P. Reduction mammaplasty combined with pectoralis major
muscle flaps for median sternotomy wound closure. Brit J Plast Surg.
1996;49(8):575-6.
9. Boodhun WS, Zinn R. Using a breast reduction to access a pedicled
myocutaneous pectoralis major flap for anterior neck defect reconstruction: a
case report. Australas J Plast Surg. 2023;6(1):71409. DOI:
10.34239/ajops.71409
10. Schwarzmann E. Die technik der mammaplastik. Chirurg.
1930;2:932-43.
11. Pitanguy I. Une nouvelle technique de plastie mammaire. Étude de 245
cas consécutifs et présentation d’une technique personnelle. Ann Chir Plast
(Marseille). 1962;7(3):199-208.
12. Duan W, Cao C, Wu J, Cen Y, Xu X, Liu Y. Application of modified
inferior pedicle technique with inverted T pattern for severe breast
hypertrophy. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33(3):341-4. DOI:
10.7507/1002-1892.201811076
13. Scomacao I, Cummins A, Roan E, Duraes EFR, Djohan R. The use of
surgical site drains in breast reconstruction: A systematic review. J Plast
Reconstr Aesthet Surg. 2020;73(4):651-62. DOI:
10.1016/j.bjps.2019.11.019
14. Jo GY, Yoon JM, Ki SH. Reconstruction of a large chest wall defect
using bilateral pectoralis major myocutaneous flaps and V-Y rotation advancement
flaps: a case report. Arch Plast Surg. 2022;49(1):39-42. DOI:
10.5999/aps.2021.01368
1. Hospital Governador Celso Ramos, Florianópolis,
SC, Brazil
Corresponding author: Felipe Barbieri Wohlgemuth
Rua Irmã Benwarda, 297, 8º andar, Sala 802, Centro, Florianópolis, SC, Brazil,
Zip Code: 88015-270, E-mail: felipewohlgemuth@gmail.com