INTRODUCTION
Surgical breast reconstruction, after locoregional cancer treatment, is related to
patients’ quality of life1.
However, in a country like Brazil, access to this type of procedure for the vast
majority of women affected by breast cancer is very limited, considering that
more
than one intervention is often necessary to achieve the expected aesthetic
result.
Thinking about the accessibility of breast repair surgery in the Brazilian public
health system, Law No. 9,797, of May 6, 1999, defined the obligation of this type
of
procedure by the network of units that are part of the Unified Health System (SUS)
in cases of mutilation resulting from cancer treatment2. This legislation was modified in 2013 (by Law No.
12,802), establishing that aesthetic repair should be performed at the same surgical
time as cancer treatment, and when this was impossible, breast reconstruction
would
be guaranteed in a second stage3;
and by ordinance GM/MS nº 127, of February 2023, which decided to install an
exceptional strategy to expand access to breast reconstruction4.
There are numerous surgical treatment options for breast cancer, and the technique
used depends on several factors, which include the biological characteristics
of the
breast neoplasm, the volume of the breast, the dimensions of the primary lesion,
the
response to neoadjuvant systemic treatment and the stage of the disease at the
time
of diagnosis, among others5. Also,
with greater access to genetic tests to check the presence of pathogenic variants
of
genes related to a greater predisposition to breast cancer, such as
BRCA1 and BRCA2, the indication for
prophylactic adenomastectomies has increased6.
Fat grafting (or lipofilling) is an autologous graft of adipose tissue cells, widely
used as an adjuvant method in breast reconstruction after oncological surgery
and/or
radiotherapy to correct volume and irregularities7. Recently, it was demonstrated that the use of fat grafting
is safe, including in conservative surgeries for the treatment of breast cancer,
and
can be used at the same surgical time as the excision of breast neoplasia8,9. Associated with the indications for this technique in the
oncology area, it is also used in numerous aesthetic procedures in the face and
breast region, in remodeling contours in different anatomical sites, in addition
to
being used to alleviate scar contractures in large burns10,11.
This type of graft is a complementary method that allows obtaining large quantities
of mesenchymal stem cells derived from subcutaneous adipose tissue (ADMSCs), which
are the cells responsible for colonization and tissue formation in the recipient
area12,13. Currently, ADMSCs are the most used as a cell
renewal strategy, as they have a similar capacity to stem cells originating from
the
bone marrow, in addition to being obtained through a less traumatic and invasive
technique. However, the procedure has limitations, as part of the volume of fat
applied is reabsorbed, compromising the result14.
In breast reconstruction, fat grafting is performed immediately after liposuction
of
small volumes of cellular fraction, with no preservation of material for subsequent
grafts, with the surplus discarded. In situations where there is a need for larger
volumes of fat grafting, several sequential fat grafting procedures are performed
until the expected aesthetic result is achieved15. This increases operating costs, in addition to generating
greater surgical risks for the patient.
The possibility of using cell cryopreservation techniques could help in this process,
as the ADMSCs would be preserved at low temperatures, for an indefinite period
and
be thawed in fractions depending on the surgical planning16. Cell cryopreservation seeks to ensure adequate
cell viability rates while maintaining their biological potential. To achieve
this,
it is necessary to use cryopreservatives during freezing techniques, with dimethyl
sulfoxide (DMSO) being the substance most used in conventional protocols in
experimental studies, as it provides good cell viability after thawing17. However, the use of
cryopreservation of ADMSCs with DMSO in clinical practice is limited, as this
solvent is toxic to human cells18.
Considering the importance of ADMSCs in post-mastectomy breast reconstruction, among
other indications in aesthetic surgery, the search for non-toxic and effective
cryopreservatives would allow the conservation of ADMSCs and, consequently, the
planning of serial fat grafts.
OBJECTIVE
Verify the cell viability of ADMSCs after cryopreservation of lipoaspirates with the
combination of L-proline and trehalose, substances that have no documented cellular
toxicity, in addition to having a low operational cost.
METHOD
Experimental cross-sectional descriptive study in which lipoaspirated tissue samples
were collected from female patients over 18 years of age who signed the Free and
Informed Consent Form (FICF) and chose to donate part of the lipoaspirate that
would
be discarded after the aesthetic liposuction procedure; carried out by 4 plastic
surgeons in hospitals in the city of Chapecó-SC, between June 2021 and March
2022.
Seeking to compare the effectiveness of cryopreservatives against different freezing
times, 90mL of lipoaspirated material was collected from each patient, which was
then allocated into 6 15mL Falcon® tubes. The material was centrifuged at
3000 rpm for 3 minutes, washed with 0.9% saline solution, and centrifuged again
with
the same parameters. Successively, collagenase IA (C2674 - Sigma®) was
added at a concentration of 0.075% in a proportion of 1:100, followed by incubation
in a water bath at 37ºC for 30 minutes, with homogenization every 10 minutes.
Collagenase inactivation was carried out with the addition of DMEM (Dulbecco’s
Modified Eagle’s Medium) + 10% fetal bovine serum (FBS) in a 1:1 ratio, and the
content was then centrifuged at 1600rpm for 10 minutes. The supernatant was
discarded, and the cell pellet was transferred to a new tube and resuspended in
2mL
of phosphate buffered saline (PBS- Phosphate Buffered Saline) for subsequent cell
counting in a Neubauer chamber. The cell set was divided into 6 tubes, and DMSO
was
added to 3 of them for a final concentration of 10% + 10% FBS. In the remaining
tubes, 1.5M L-proline and 0.2M trehalose dissolved in PBS buffer were added. The
samples were then frozen at -80ºC (Figure 1).
Figure 1 - Steps of the methodology for cryopreservation of lipoaspirates
containing mesenchymal stem cells derived from subcutaneous adipose
tissue.
Figure 1 - Steps of the methodology for cryopreservation of lipoaspirates
containing mesenchymal stem cells derived from subcutaneous adipose
tissue.
The sample thawing process in a water bath at 37ºC took place after 30 and 90 days.
In samples containing DMSO, removal was performed by dilution and washing with
PBS
buffer. L-proline and trehalose did not require removal. The samples were cultured
in triplicate in sterile 12-well plates at a concentration of 106 cells per well.
2mL of DMEM containing 10% FBS and 1% penicillin + 1% streptomycin were added
to
each well. The samples were incubated in a CO2-free oven at 37ºC for 24 hours.
Cell viability was performed using the 3-(4,5 - dimethylthiazol-2yl)-2,5
diphenyltetrazolium bromide (MTT) assay. The content contained in the wells was
transferred to 1.5mL microtubes, which were centrifuged at 3000rpm for 15 minutes.
The supernatant portion was discarded, and 300uL of PBS + 20uL of MTT were added
to
the cell pellet and incubated again at 37ºC for 1 hour. Subsequently, the samples
were centrifuged with the same parameters as in the previous step, then 75uL of
each
sample was discarded, and the same volume of DMSO was added. The samples were
homogenized and transferred to a 96-well plate for absorbance evaluation by
spectrophotometry at 560ηm (Figure 2).
Figure 2 - Steps of the methodology for thawing material cryopreserved with
L-proline associated with trehalose and evaluating cell viability. Step
carried out at 30 days and 90 days of cryopreservation.
Figure 2 - Steps of the methodology for thawing material cryopreserved with
L-proline associated with trehalose and evaluating cell viability. Step
carried out at 30 days and 90 days of cryopreservation.
The cell viability data generated were tabulated in a Microsoft® Office
Excel spreadsheet, and a two-way ANOVA test was then performed using GraphPad
Prism
6.0, considering the results significant when p<0.05.
The initial research project was approved by the Unochapecó Research Ethics
Committee, under CAAE 23243519.7.0000.0116, and opinion number 4,822,999, and
by the
institutions involved.
RESULTS
Samples were processed and frozen from 9 female patients, self-declared as white,
and
who underwent a third generation ultrasonic assisted liposuction procedure (Vaser).
The lipoaspirates were cryopreserved and analyzed in two moments, after 30 and
90
days of freezing. The average age of the liposuction donor patients was 35.7 years,
while the average body mass index (BMI) was 25kg/m2.
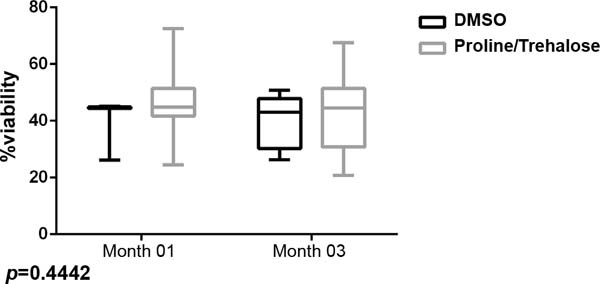
The main collection site was in the abdominal region and the cannula number most used
was 3.7mm. The assessment of cell viability after one and three months of freezing
indicated that samples cryopreserved with L-proline + trehalose showed cell
viability similar to those containing DMSO + SBF (p=0.4442) (Figure 3). Furthermore, in relation to freezing
time, samples that were frozen for 90 days maintained viable ADMSCs when compared
to
samples thawed in the first month (p=0.5301), noting that, in
addition to the type of cryopreservative, the freezing time also did not seem
to
interfere with cell viability.
Figure 3 - Comparison of cell viability obtained after freezing with DMSO/SFB
and with L-proline associated with trehalose.
Figure 3 - Comparison of cell viability obtained after freezing with DMSO/SFB
and with L-proline associated with trehalose.
DISCUSSION
Several factors can influence the viability of ADMSCs, including lipoaspirate
extraction and injection methodologies, centrifugation speed, use of anesthetic
and/or saline solutions, the volume of aspirated content, location and biological
characteristics of the adipose tissue in the donor area, among others12,19. Furthermore, there is no consensus on the best way to
process fat for later use as a graft11,17.
Clinical and phenotypic characteristics of patients can influence the quality of the
adipose material aspirated. As in BMI, where, in patients with values greater
than
25kg/m2, there is an indirect relationship with the capacity for cell
proliferation and differentiation; that is, the patient’s excess weight can
contribute to unsatisfactory results when using ADMSCs in reconstructive
surgeries20.
The patient’s age is also a relevant factor due to the changes caused by aging in
ADMSCs. This is due to several cellular events, such as the shortening of telomeres
and weakening of the antioxidant protection system associated with oxidative stress
and accumulated damage to the DNA repair system21,22.
In the present study, these factors probably did not interfere in the assessment of
cell viability, as the average values found for these two variables in the group
of
patients studied were within the range of results described in the reviewed
literature19-21.
Another aspect verified in the literature that could interfere with cell viability
would be the diameter of the cannula used both in collecting the lipoaspirate
in the
donor area and in injecting the fraction containing the ADMSCs in the recipient
area23. In a review
article, it was shown that most authors use cannulas ranging from 2mm to
6mm24, but cell viability
is greater when liposuction is performed with cannulas with diameters greater
than
3mm25. These results can
be explained by obtaining aspirates with a large number of cells from the stromal
vascular fraction, compared to the use of cannulas with smaller diameters25,26.
Most authors use cannulas with a diameter smaller than 2mm to inject the intermediate
fraction of the lipoaspirate, as this reduces the chance of material extravasation,
in addition to minimizing the possibility of injecting the content
intravascularly27. In the
present study, samples obtained with 3mm, 3.7mm, 4mm, and 5mm cannulas were used,
with the 3.7mm being the most prevalent. Fat grafting was not performed in any
of
the procedures.
The way the lipoaspirate components are separated can be via decantation or
centrifugation. The centrifugation technique allows you to concentrate fat and
increase the number of cells per milliliter while separating the liquefied fat
and
blood cell components28. Studies
indicate that the ADMSCs present in the sediment, obtained after washing the
centrifuged material, have greater viability since they are not contaminated with
blood cell residues, which is common in samples treated only by decantation, in
addition to there being greater disruption of the adipocyte walls and a greater
number of ADMSCs12,29,30.
In the publication in which we compared different centrifugation speeds, we
documented the methodology described by Coleman (3000rpm for three minutes) and
found greater maintenance of the biological characteristics of ADMSCs necessary
for
cell colonization in graft recipient areas12,29. This is because
centrifuging the samples makes the fat cells more concentrated, in addition to
separating them from the blood cells30.
Likewise, in the present study, the samples were centrifuged to separate the tissue
fractions into three well-defined portions: a lower layer of blood cells, an
intermediate layer containing stromal cells and adipose tissue, and a superficial
layer of liquefied fat. As a result, there was no interference from blood cell
debris and liquefied fat in the cultivation and cryopreservation of ADMSCs.
Cell viability after a period of cryopreservation may also vary depending on the
number of cells stored in each microtube31. Goh et al.16 used four cell concentrations and noted that the concentration
of 5x105 cells/mL presented a viability rate of 81.10%, while at a
concentration of 1x106 cells/mL, the viability was 77.9%. Few studies
described in the literature have documented the viability of ADMSCs as significant
as the one published by De Rosa et al.32, in which a rate of 92.5% of viable cells was described;
however, the cell concentration was 6x103 cells/mL.
For this research, the concentration of cells used in each microtube was
5x105 cells/mL, and the viability rates in cells frozen with both
L-proline and trehalose and the DMSO control were close to 60%. Comparing these
results, it is possible to infer that a smaller number of cells stored in each
microtube is related to a higher viability rate, probably due to the more adequate
space for the physiological maintenance of ADMSCs.
Considering the temperature used to freeze the samples, we kept the cells frozen at
-80ºC, using the rapid cooling technique, which was also used by Ray et
al.33. However, currently,
the most frequently described temperature for cell storage would be -196ºC (via
liquid nitrogen), as the use of a -80ºC freezer would be related to the greater
formation of ice crystals, which could cause damage to the cryopreserved material.
However, the use of liquid nitrogen is a technique that requires high maintenance
costs31,34.
In relation to cryopreservatives, DMSO is the substance most used in various
protocols for cell preservation, as it is related to maintaining the viability
of
CTAS11. However, it is a
toxic substance causing negative changes in cellular processes such as metabolism,
citric acid cycle pathways, respiratory electron transport, glucose, lipid, and
lipoprotein metabolism. It is also related to changes in mitochondrial pathways,
the
production of reactive oxygen species, and the generation of cellular ATP35.
In the present research, we chose to use two low-cost natural cryopreservatives,
which are alternatives to DMSO. Trehalose is a non-reducing disaccharide made
up of
two glucose units, while L-proline is a natural amino acid formed through
biosynthesis from L-glutamate. Both do not cause toxicity in the cell and are
a
source of studies in the search for a suitable cryopreservative36.
In a study carried out with red blood cells cryopreserved with different
concentrations of L-proline and trehalose, maintenance of cellular structure was
observed, in addition to not having altered the activity of the Na +/K +-ATPase
pumps, whose function is to maintain the concentrations of intracellular ions,
very
relevant for signal transduction and cellular metabolism, in addition to DNA
methylation not being altered22,37. Furthermore, because L-proline
and trehalose are not toxic to cells, there is no need to remove cryoprotectants,
reducing cell loss, as is done when DMSO23 is used.
According to studies by Dovgan et al.38, which used a cryopreservation protocol with only trehalose
(0.25M), there was comparable cell viability of the non-toxic agent in relation
to
DMSO; it was also observed that trehalose concentrations have a positive correlation
in relation to cell viability. In another study, it was demonstrated that ADMSCs
from lipoaspirate, when cryopreserved for 6 months with trehalose at a concentration
of 0.35M, are able to maintain biological activity, almost at the same rate as
fresh
tissue39. In the present
study, the association of L-proline and trehalose showed cell vitality levels
comparable to the use of DMSO in the cryopreservation of ADMSCs.
Cell cryopreservation time has also been studied31,34,40. De Rosa et al.32 kept the cells frozen for up to 12 months, using
trehalose, DMSO, and SBF, and found significant cell viability data, with more
than
80% of cells recovered. Also, it has already been documented that, when leaving
the
cells cryopreserved for 6 months, the cell proliferation and differentiation
potential was similar to the group of non-cryopreserved cells39,41. In the present study, it was possible to demonstrate that
ADMSC samples frozen for 90 days showed cell viability similar to those frozen
for
30 days. In other words, cryopreservation for long periods can be a feasible
methodology, for the fractional use of ADMSCs in multiple surgical times with
the
use of sufficient volumes for surgical corrections, whether aesthetic or repair.
CONCLUSION
Cryopreservation of ADMSCs with the combined use of L-proline and trehalose resulted
in cell viability equivalent to the use of DMSO. Furthermore, cells frozen for
90
days maintained viability rates similar to those stored for a shorter period.
Considering the data found and those reviewed in the literature, the use of the
combination of L-proline and trehalose may be an option for DMSO, avoiding cellular
toxicity. This methodology can be an alternative to avoid multiple liposuction
collections in surgical procedures that require several fat grafting sessions,
especially in breast reconstruction after surgical treatment of breast cancer.
ACKNOWLEDGMENTS
To all fellow researchers in the research group “Molecular Biology and Biotechnology
in Health” at the Universidade Comunitária da Região de Chapecó (Unochapecó) and
the
research group “Biological and Clinical Studies in Human Pathologies” at the
Universidade Federal da Fronteira Sul (UFFS) Chapecó-SC campus. To plastic surgeons
Dr. Gustavo Colonheze, Dr. Jorge Diego Valentini, Dr. Rafael de Almeida Tirapelle,
and Dr. Tainara Cassol, who kindly agreed to participate in the initial contact
of
the patients and welcome the team of researchers.
REFERENCES
1. Fanakidou I, Zyga S, Alikari V, Tsironi M, Stathoulis J, Theofilou
P. Mental health, loneliness, and illness perception outcomes in quality of life
among young breast cancer patients after mastectomy: the role of breast
reconstruction. Qual Life Res. 2018;27(2):539-43.
2. Brasil. Presidência da República. Lei Nº 9.797, de 6 de maio de
1999. Dispõe sobre a obrigatoriedade da cirurgia plástica reparadora da mama
pela rede de unidades integrantes do Sistema Único de Saúde - SUS nos casos de
mutilação decorrentes de tratamento de câncer. Brasília: Presidência da
República; 1999. [Internet]. Disponível em: https://legislacao.presidencia.gov.br/atos/?tipo=LEI&numero=9797&ano=1999&ato=b04cXRE9keNpWT174
3. Brasil. Presidência da República. Lei Nº 12.802, de 24 de abril de
2013. Altera a Lei nº 9.797, de 6 de maio de 1999, que “dispõe sobre a
obrigatoriedade da cirurgia plástica reparadora da mama pela rede de unidades
integrantes do sistema único de saúde - SUS nos casos de mutilação decorrentes
de tratamento de câncer”, para dispor sobre o momento da reconstrução mamária.
[Internet]. Brasília: Presidência da República; 2013. Disponível em: https://legislacao.presidencia.gov.br/atos/?tipo=LEI&numero=12802&ano=2013&ato=97cATRU50MVpWTabf
4. Brasil. Ministério da Saúde. Portaria GM/MS nº 127, de 13 de
fevereiro de 2023. Institui estratégia excepcional de ampliação do acesso à
reconstrução mamária em caso de mulheres com diagnóstico de câncer de mama, no
âmbito do Sistema Único de Saúde -SUS. [Internet]. Brasília: Ministério da
Saúde; 2023. Disponível em: https://www.gov.br/saude/pt-br/composicao/saes/legislacao/portaria-gm-ms-no-127-de-13-de-fevereiro-de-2023/view
5. Loibl S, Poortmans P, Morrow M, Denkert C, Curigliano G. Breast
cancer. Lancet. 2021;397(10286):1750-69.
6. Petrucelli N, Daly MB, Pal T. BRCA1- and BRCA2-Associated Hereditary
Breast and Ovarian Cancer: Synonym: BRCA1- and BRCA2-Associated HBOC [Internet].
2022 [acesso 2022 nov 11]. Disponível em: https://www.ncbi.nlm.nih.gov/books/NBK1247/
7. Tan SS, Loh W. The utility of adipose-derived stem cells and stromal
vascular fraction for oncologic soft tissue reconstruction: Is it safe? A matter
for debate. Surgeon. 2017;15(4):186-9.
8. Stumpf CC, Zucatto ÂE, Cavalheiro JAC, de Melo MP, Cericato R, Damin
APS, et al. Oncologic safety of immediate autologous fat grafting for
reconstruction in breast-conserving surgery. Breast Cancer Res Treat.
2020;180(2):301-9.
9. Krastev TK, Schop SJ, Hommes J, Piatkowski AA, Heuts EM, van der
Hulst RRWJ. Meta-analysis of the oncological safety of autologous fat transfer
after breast cancer. Br J Surg. 2018;105(9):1082-97.
10. He X, Zhang J, Luo L, Shi J, Hu D. New Progress of Adipose-derived
Stem Cells in the Therapy of Hypertrophic Scars. Curr Stem Cell Res Ther.
2020;15(1):77-85.
11. Zuk P. Adipose-Derived Stem Cells in Tissue Regeneration: A Review.
Int Sch Res Notices. 2013;2013:1-35.
12. Moreno M, Schmidt JC, Gazzoni CD, Dal-Magro L, Bonadiman BDSR,
Kosvoski GC, et al. Viability of mesenchymal stem cells of adipose tissue from
human liposuction. Rev Bras Cir Plást. 2021;36(1):9-14.
13. da Silva A, do Prado J, Pignataro J, Moreno M. Lipoenxertia. In:
Bagnoli F, Postiglione F, Palermo F, Pedrini JL, Freitas Júnior R, Marques V.
Mastologia: do diagnóstico ao tratamento. 2ª ed. Goiânia: Conexão Soluções
Corporativas; 2022.
14. Arshad Z, Karmen L, Choudhary R, Smith JA, Branford OA, Brindley DA,
et al. Cell assisted lipotransfer in breast augmentation and reconstruction:
A
systematic review of safety, efficacy, use of patient reported outcomes and
study quality. JPRAS Open. 2016;10:5-20.
15. Piffer A, Aubry G, Cannistra C, Popescu N, Nikpayam M, Koskas M, et
al. Breast Reconstruction by Exclusive Lipofilling after Total Mastectomy for
Breast Cancer: Description of the Technique and Evaluation of Quality of Life.
J
Pers Med. 2022;12(2):153.
16. Goh BC, Thirumala S, Kilroy G, Devireddy RV, Gimble JM.
Cryopreservation characteristics of adipose-derived stem cells: maintenance of
differentiation potential and viability. J Tissue Eng Regen Med.
2007;1(4):322-4.
17. Lee JE, Kim I, Kim M. Adipogenic differentiation of human adipose
tissue-derived stem cells obtained from cryopreserved adipose aspirates.
Dermatol Surg. 2010;36(7):1078-83.
18. Wang C, Xiao R, Cao YL, Yin HY. Evaluation of human platelet lysate
and dimethyl sulfoxide as cryoprotectants for the cryopreservation of human
adipose-derived stem cells. Biochem Biophys Res Commun.
2017;491(1):198-203.
19. Kim IH, Yang JD, Lee DG, Chung HY, Cho BC. Evaluation of
centrifugation technique and effect of epinephrine on fat cell viability in
autologous fat injection. Aesthet Surg J. 2009;29(1):35-9.
20. Frazier TP, Gimble JM, Devay JW, Tucker HA, Chiu ES, Rowan BG. Body
mass index affects proliferation and osteogenic differentiation of human
subcutaneous adipose tissue-derived stem cells. BMC Cell Biol.
2013;14:34.
21. Efimenko AY, Kochegura TN, Akopyan ZA, Parfyonova YV. Autologous
Stem Cell Therapy: How Aging and Chronic Diseases Affect Stem and Progenitor
Cells. Biores Open Access. 2015;4(1):26-38.
22. Zhang TY, Tan PC, Xie Y, Zhang XJ, Zhang PQ, Gao YM, et al. The
combination of trehalose and glycerol: an effective and non-toxic recipe for
cryopreservation of human adipose-derived stem cells. Stem Cell Res Ther.
2020;11(1):460.
23. Toledo LS, Mauad R. Fat injection: a 20-year revision. Clin Plast
Surg. 2006;33(1):47-53.
24. Piccotti F, Rybinska I, Scoccia E, Morasso C, Ricciardi A, Signati
L, et al. Lipofilling in Breast Oncological Surgery: A Safe Opportunity or Risk
for Cancer Recurrence? Int J Mol Sci. 2021;22(7):3737.
25. Becker H, Vazquez OA, Rosen T. Cannula Size Effect on Stromal
Vascular Fraction Content of Fat Grafts. Plast Reconstr Surg Glob Open.
2021;9(3):e3471.
26. Tong Y, Liu P, Wang Y, Geng C, Han X, Ma J, et al. The Effect of
Liposuction Cannula Diameter on Fat Retention-Based on a Rheological Simulation.
Plast Reconstr Surg Glob Open. 2018;6(11):e2021.
27. Biazus JV, Falcão CC, Parizotto AC, Stumpf CC, Cavalheiro JA, Schuh
F, et al. Immediate Reconstruction with Autologous fat Transfer Following
Breast-Conserving Surgery. Breast J. 2015;21(3):268-75.
28. Condé-Green A, de Amorim NF, Pitanguy I. Influence of decantation,
washing and centrifugation on adipocyte and mesenchymal stem cell content of
aspirated adipose tissue: a comparative study. J Plast Reconstr Aesthet Surg.
2010;63(8):1375-81.
29. Coleman SR. Long-term survival of fat transplants: controlled
demonstrations. Aesthetic Plast Surg. 1995;19(5):421-5.
30. Ladeira PRS, Isaac C, Nakamura YM, Tutihashi RMC, Paggiaro AO,
Ferreira MC. Cultivo de células-tronco derivadas de tecido adiposo: uma análise
crítica. Rev Med (São Paulo). 2012;91(4):246-52.
31. Irioda AC. Avaliação da integridade das células-tronco mesenquimais
derivadas do tecido adiposo humano após o bioprocesso de criopreservação
[Dissertação de mestrado]. Curitiba: Universidade Federal do Paraná; 2010.
Disponível em: http://hdl.handle.net/1884/26521
32. De Rosa A, De Francesco F, Tirino V, Ferraro GA, Desiderio V, Paino
F, et al. A new method for cryopreserving adipose-derived stem cells: an
attractive and suitable large-scale and long-term cell banking technology.
Tissue Eng Part C Methods. 2009;15(4):659-67.
33. Ray SS, Pramanik K, Sarangi SK, Jain N. Serum-free non-toxic
freezing solution for cryopreservation of human adipose tissue-derived
mesenchymal stem cells. Biotechnol Lett. 2016;38(8):1397-404.
34. Ginani F, Soares DM, Barboza CAG. Influência de um protocolo de
criopreservação no rendimento in vitro de células-tronco derivadas do tecido
adiposo. Rev Bras Cir Plást. 2012;27(3):359-63.
35. Verheijen M, Lienhard M, Schrooders Y, Clayton O, Nudischer R,
Boerno S, et al. DMSO induces drastic changes in human cellular processes and
epigenetic landscape in vitro. Sci Rep. 2019;9(1):4641.
36. Kennelly P, Rodwell V. Aminoácidos e Peptídeos. In: Rodwell VW,
Bender D, Botham KM, Kennelly PJ, Weil PA. Bioquímica Ilustrada de Harper. 31ª
ed. Porto Alegre: AMGH Editora; 2021.
37. Dou M, Lu C, Sun Z, Rao W. Natural cryoprotectants combinations of
l-proline and trehalose for red blood cells cryopreservation. Cryobiology.
2019;91:23-9.
38. Dovgan B, Miklavčič D, Knežević M, Zupan J, Barlič A. Intracellular
delivery of trehalose renders mesenchymal stromal cells viable and
immunomodulatory competent after cryopreservation. Cytotechnology.
2021;73(3):391-411.
39. Dalmagro JP. Isolamento e caracterização das células-tronco
mesenquimais provenientes do tecido adiposo e avaliação da sua viabilidade
tecidual após criopreservação [Monografia]. Porto Alegre: Universidade Federal
do Rio Grande do Sul; 2019.
40. Lenoch CY. Estratégias para criopreservação de células tronco
mesenquimais de tecido adiposo bovino [Dissertação de mestrado]. Lages:
Universidade do Estado de Santa Catarina; 2015.
41. Gonda K, Shigeura T, Sato T, Matsumoto D, Suga H, Inoue K, et al.
Preserved proliferative capacity and multipotency of human adipose-derived stem
cells after long-term cryopreservation. Plast Reconstr Surg.
2008;121(2):401-10.
1. Universidade Federal da Fronteira Sul, Chapecó,
SC, Brazil
2. Universidade Comunitária da Região de Chapecó,
Chapecó, SC, Brazil
Corresponding author: Marcelo Moreno Rodovia SC
484, Km 02, Bloco dos professores, Chapecó, SC, Brazil, Zip Code: 89815-899,
E-mail: marcelo.moreno@uffs.edu.br
Article received: May 15, 2023.
Article accepted: August 20, 2023.
Conflicts of interest: none.