

Original Article - Year 2023 - Volume 38 -
Medial plantar flap for reconstruction of heel defects after resection of acral lentiginous melanoma: A series of seven cases
Retalho plantar medial para reconstrução de defeitos em calcanhar após ressecção de melanoma lentiginoso acral: Uma série de 7 casos
ABSTRACT
Introduction: Resurfacing the sole is still one of the great challenges of reconstructive plastic surgery. The tissues on the sole of the foot have unique characteristics essential for maintaining the limbs functionality. The heel has the most significant weight support and is subjected to the entire soles greatest impact. The medial plantar artery flap is one of the reconstructive options, as it represents similar tissue and maintains sensitivity to the recipient area.
Methods: A retrospective study was performed by collecting data from medical records of patients who underwent reconstructions of the heel with a medial plantar artery flap from July 2013 to September 2019. The study was approved by the Ethics Committee for Analysis of Research Projects of HCFMUSP (CAAE number: 56849422.0.0000.0068).
Results: Heel reconstruction was performed in 7 patients after acral lentiginous melanoma excision. Surgical complications were observed in 3 patients, all of whom were aged over 50 years or have associated comorbidity. There were 57.1% of complications, 37.5% related to the flap, and 12.5% related to the donor area. There were three total flap necroses (42.9%) and one total graft loss in the donor area (14.3%).
Conclusion: The medial plantar flap presents itself as a good alternative for performing oncological reconstructions of defects in the plantar region of the foot. However, the choice of the ideal patient should be considered and we must remember that the dissection of its vascular pedicle is not easily executed.
Keywords: Melanoma; Skin neoplasms; Surgical flaps; Reconstructive surgical procedures; Heel.
RESUMO
Introdução: A reconstrução da região plantar ainda é um dos grandes desafios da cirurgia
plástica reconstrutiva. Os tecidos dessa região apresentam características
únicas e que são essenciais para a manutenção da funcionalidade do membro.
De toda a região plantar, a região do calcanhar é a área de maior
sustentação do peso e submetida ao maior impacto. O retalho fasciocutâneo
plantar medial é uma das opções reconstrutivas, pois representa tecido
semelhante e mantém a sensibilidade para a área receptora.
Método: Foi realizado um estudo retrospectivo através da coleta de dados de
prontuário de pacientes que realizaram reconstruções da região do calcanhar
com retalho plantar medial, no período de julho de 2013 a setembro de 2019.
O estudo foi aprovado pelo Comitê de Ética para Análise de Projetos de
Pesquisa do HCFMUSP (Número CAAE: 56849422.0.0000.0068).
Resultados: A reconstrução de calcanhar após ressecção de melanoma lentiginoso acral foi
realizada em 7 pacientes. Complicações cirúrgicas foram observadas em 3
pacientes, sendo que todos eles tinham idade acima de 50 anos e/ou alguma
comorbidade associada. Houve 57,1% de complicações, sendo 37,5% relacionadas
ao retalho e 12,5% relacionadas à área doadora. Ocorreram 3 necroses totais
de retalho (42,9%) e 1 perda total de enxerto na área doadora (14,3%).
Conclusão: O retalho plantar medial se apresenta como uma boa alternativa para a
realização de reconstruções oncológicas de defeitos na região plantar do pé.
Contudo, deve-se ponderar a escolha do paciente ideal e lembrar que a
dissecção do seu pedículo vascular não é de fácil execução.
Palavras-chave: Melanoma; Neoplasias cutâneas; Retalhos cirúrgicos; Procedimentos cirúrgicos reconstrutivos; Calcanhar
INTRODUCTION
Reconstruction of the plantar region is still one of the greatest challenges in reconstructive plastic surgery1,2. The tissues in this region have unique characteristics essential for maintaining the functionality of the limb. We can mention local characteristics: strong adhesion between the skin and deep structures, providing stability when walking; the presence of a thick cushion, allowing impact absorption when walking.
Of the entire plantar region, the heel region is the area with the greatest weight-bearing and subjected to the greatest impact. To this end, it is richly vascularized and has fibrous septa that connect the dermis to the periosteum of the calcaneal bone, forming fat compartments3-7.
We must, therefore, look for tissues with similar characteristics for the reconstruction of plantar defects in the heel8.
There are several methods of reconstruction of the plantar region, ranging from skin grafting to microsurgical flaps, but few meet all of these needs1,2,8-14.
The medial plantar fasciocutaneous flap is an excellent option, as it represents similar tissue and maintains sensitivity to the recipient area15,16.
Initially described in 1981 by Harrison & Morgan9, the medial plantar flap is based on the medial plantar artery and maintains local sensitivity through cutaneous branches of the medial plantar nerve17. Since then, several studies have been described in the literature, but few evaluate its use in cancer patients18,19.
OBJECTIVE
To describe a series of 7 cases of reconstruction of heel defects after resection of acral lentiginous melanoma, performed at the Plastic Surgery Service of the Instituto do Câncer of the State of São Paulo, from July 2013 to September 2019.
METHOD
A retrospective study collected data from medical records of patients who underwent reconstruction of the heel region with a medial plantar flap from July 2013 to September 2019.
Patients were selected according to the type of reconstruction used after resection of acral lentiginous melanoma by the Sarcoma and Melanoma Group at the Instituto do Câncer of the State of São Paulo. The inclusion criteria for the study were: patients admitted to the Instituto do Câncer of the State of São Paulo for resection of acral lentiginous melanoma of the heel region, undergoing reconstruction with a medial plantar flap.
Of the 7 patients, 3 (42.8%) were female, and 4 (57.1%) were male (Table 1). Six patients (85.7%) had some associated comorbidity, with smoking and systemic arterial hypertension being the most prevalent comorbidities. The average age of the patients was 57.3 years, ranging from 45 to 73 years.
| Age | Sex | Histologic Type |
Comorbidities | Additional
local reconstruction |
Donor area | Retail complications |
Donor
area complications |
|
|---|---|---|---|---|---|---|---|---|
| 1 | 58 | M | Acral Melanoma |
Smoking, SAH | No | Partial skin grafting | Necrosis | No |
| 2 | 53 | M | Acral Melanoma |
Smoking, hypertension, DM |
No | Partial skin grafting | Necrosis | No |
| 3 | 64 | M | Acral Melanoma |
Smoking, hypertension, alcoholism, CKD |
No | Partial skin grafting | No | No |
| 4 | 73 | M | Acral Melanoma |
Smoking, hypertension, previous AMI |
No | Partial skin grafting | No | No |
| 5 | 51 | F | Acral Melanoma |
Smoking, rheumatoid arthritis |
Total
skin grafting |
Partial skin grafting | Não | Graft loss |
| 6 | 45 | F | Acral Melanoma |
No | Partial skin grafting | No | No | |
| 7 | 57 | F | Acral Melanoma |
SAH | No | Partial skin grafting | Necrosis | No |
M: Masculine; F: Female; SAH: Systemic Arterial Hypertension; DM: Diabetes Mellitus; CKD: Chronic Kidney Disease; AMI: Acute Myocardial Infarction.
The HCFMUSP Ethics Committee approved the study for Analysis of Research Projects (CAAE Number: 56849422.0.0000.0068).
Surgical technique
The posterior tibial artery is identified through palpation posterior to the medial malleolus, and a broken line demarcation is made just above this region.
The skin island is demarcated according to the size of the defect in the heel region and can extend across the entire area outside of plantar support.
The incision begins with the demarcation posterior to the medial malleolus, and the posterior tibial artery is identified. The medial edge of the flap is incised, and the artery is dissected until its bifurcation. The medial branch is identified between the abductor hallucis and flexor digitorum brevis muscles. The flap is then elevated by including the plantar fascia and the lateral branch of the medial plantar nerve, sparing the medial innervation of the hallux.
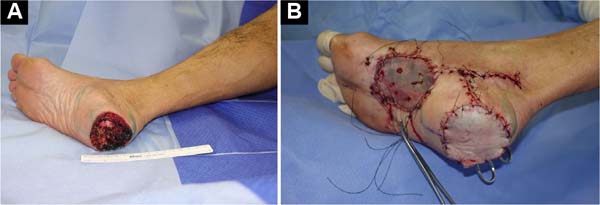
The lateral, distal, and proximal edges are incised as the dissection progresses. The flap is transposed to the heel defect, and the donor area is reconstructed with a partial skin graft from the ipsilateral thigh (Figures 1 and 2).
RESULTS
One patient required additional reconstruction with local skin grafting; in the others, the medial plantar flap was sufficient to cover the dry areas. In all cases, partial skin grafting was performed in the flap donor area.
Lymphadenectomy was performed in 3 patients (42.8%), 2 (28.6%) in the left inguinal region, and 1 (14.3%) in the left inguinal region associated with the left iliac-obturator region. Among the 7 patients, 2 had metastatic disease (28.6%).
Surgical complications were observed in 3 patients, all over 50 years old and/or had some associated comorbidity. The flap survival rate was 57%. Regarding complications, there were 3 total flap necrosis (42.9%) and 1 total graft loss in the donor area (14.3%). Of the 3 patients with flap necrosis, 2 required subsequent local reconstruction with an anterolateral fasciocutaneous microsurgical thigh flap and 1 with a lateral fasciocutaneous microsurgical arm flap.
One of the patients with total necrosis of the medial plantar flap underwent resection of acral lentiginous melanoma on the left lower limb, with immediate reconstruction with a medial plantar flap. He progressed well during hospitalization and was discharged on the seventh postoperative day. He returned for an outpatient consultation on the 11th postoperative day, presenting a flap with signs of distress at the edges. We opted for expectant treatment of the complication, and the flap presented total necrosis on the 26th postoperative day. Debridement and reconstruction with an anterolateral thigh microsurgical flap were performed. Currently, the patient presents a good appearance of the flap and good functionality of the left lower limb.
DISCUSSION
Reconstruction of the soft tissues of the heel still represents a challenge for plastic surgeons due to the scarcity of local tissues and the complexity of this reconstruction to preserve functionality.
During surgical planning, it is important to assess whether the plantar injury is located in a support area, as grafts in this region can develop complications such as ulceration, scar retraction, pain, bone deformities, and inability to walk.
Initially described in 1981, the medial plantar flap still represents one of the best options for reconstruction of the heel region, especially on its plantar surface9. Among its advantages, the following stand out: similar local tissue and preserved innervation.
The local tissue is formed by a thick pad of skin without hair follicles, which provides adequate coverage for the pressure area and support for the patient’s weight and is aesthetically more favorable. Innervation through the cutaneous branch of the medial plantar nerve allows the patient to maintain sufficient tactile sensitivity for adequate ambulation and limb protection.
As a disadvantage of the medial plantar flap, we can mention the morbidity of the donor area, located in the plantar cavity region, which constitutes an area of non-support and where partial skin grafting is necessary. Despite the section of the medial plantar artery, the foot maintains its adequate vascularization through the deep plantar arch, formed by the foot’s lateral and dorsal plantar arteries.
The medial plantar flap has the following limitations: size and depth of the area to be reconstructed, limited to smaller defects. Larger resections should preferably be reconstructed with fasciocutaneous or musculocutaneous microsurgical flaps, and alternatively, they can be reconstructed with the reverse sural flap.
Although the medial plantar flap is described in the literature with low complication rates, most published studies describe the medial plantar flap in patients suffering from trauma or pressure ulcers, with a lower average age4,8,11,16,17,20,21. This work focused on cancer patients, who typically have multiple comorbidities, advanced age, and, therefore, atheromatosis, a selection bias that could explain the higher rate of complications in this study. Furthermore, the study was carried out in a teaching hospital, where the surgical procedures were performed by different surgeons still on the learning curve.
CONCLUSION
The medial plantar flap is versatile and has a well-known vascular anatomy. Today, it presents itself as a great alternative for conducting oncological reconstructions of defects in the plantar region of the foot. However, the choice of the ideal patient must be considered, and remember that the dissection of the vascular pedicle is not easy to perform.
1. Instituto do Câncer do Estado de São Paulo, São
Paulo, SP, Brazil
2. Hospital das Clínicas, Faculdade de Medicina,
Universidade de São Paulo, São Paulo, SP, Brazil
Corresponding author: Giulia Godoy Takahashi Rua Arruda Alvim, 423, apto 51, Pinheiros, São Paulo, SP, Brazil, Zip Code: 05410-020, E-mail: giu.godoy@gmail.com







 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter