INTRODUCTION
Abdominoplasty is among the most popular cosmetic procedures in plastic surgery
in recent years1. Their search
not only impacts body contouring issues, but also improves patients’ quality
of
life and self-esteem of patients2.
From the perspective of body image, the navel is a key part since it has a
definitive role in the aesthetics of the abdominal wall. Its absence,
distortion, or poor healing compromises the surgical outcome3.
Due to its importance, the construction of the neoumbilicus, which aims to seek a
natural position, in the midline, at the level of the superior iliac crests,
with a minimal evident scar3,
and 1.5 to 2 cm in diameter4, is a determining factor for postoperative
success5,6.
Several techniques have been described in the literature, but all with their
limitations7-10.
More recent options, which try to deepen the scar, not making it visible, present
complications, such as a flattened navel11.
Furthermore, neo-umbilical stenosis is a frequent complication in surgical
tactics that aim to construct a small umbilicus or result in circular or
concentric scars12-15.
When the umbilical stump is long, it needs to be shortened, which may result in
other complications, such as stenosis or discharge from the
neoumbilicus16.
Due to the complexity of the issue and the search to improve and develop a
surgical tactic with better results, Viterbo17 (1998) described the H-shaped technique for
omphaloplasty. In it, using four rectangular flaps, there is the reconstruction
of the lateral walls of the navel, with good results and lower rates of
aesthetic complications.
OBJECTIVE
This article summarizes the surgical possibilities presented in the Revista
Brasileira de Cirurgia Plástica (RBCP) in the last 20 years and reintroduces
the
surgical technique in H.
METHOD
In order to carry out a qualitative review of the literature, a study of
publications in the RBCP from 2000 to 2021 was carried out.
Analysis of RBCP articles
The research was carried out in articles with the descriptors
“omphaloplasty,” “umbilicus,” “neoumbilicus,” “umbilicoplasty,” and
“umbilical scar” in September 2021 on the RBCP website.
Surgical technique
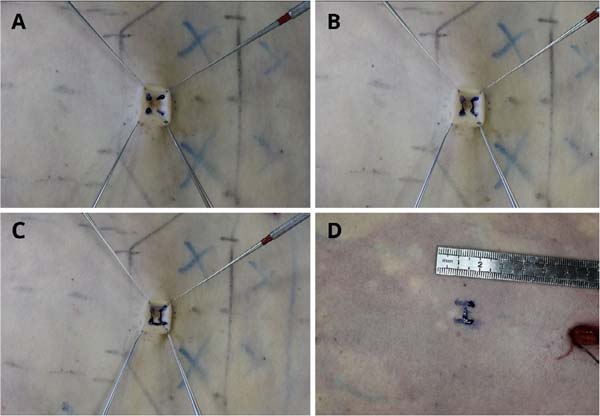
In the navel, which will be removed from the abdomen, we mark four lines in
the longitudinal direction, from the bottom to the edges, creating a
division of four equal parts in the umbilical circumference (Figure 1A). Next, two transverse lateral
lines are drawn, deeply connecting the longitudinal lines, in order to
delimit two lateral flaps, with the base having ¼ of the circumference of
the umbilicus and the length half of the base, and these values may vary,
for correct very deep navels (Figure 1B). Then, two more transversal lines are drawn, superficially
joining the longitudinal lines (Figure 1C).
Figure 1 - Right side view: Four longitudinal lines are drawn from the
bottom to the edges (A); two lateral transverse lines are drawn
in a vertical plane, deeply joining the longitudinal lines (B);
two transverse lines are drawn, superficially joining the
longitudinal lines in a horizontal plane (C); a capital letter
“H” is drawn where the new navel will emerge (D).
Figure 1 - Right side view: Four longitudinal lines are drawn from the
bottom to the edges (A); two lateral transverse lines are drawn
in a vertical plane, deeply joining the longitudinal lines (B);
two transverse lines are drawn, superficially joining the
longitudinal lines in a horizontal plane (C); a capital letter
“H” is drawn where the new navel will emerge (D).
After making the incisions, we will release the navel as a “bow-tie,” with a
central part and two lateral flaps. Then, a simple stitch is applied,
leaving the thread long for easy flap location.
After displacement, traction, resection, and suture of the abdominal flap, we
mark the place where the umbilicus will emerge, the design of the capital
letter “H” inside a square that will have dimensions of ¼ of the umbilicus
circumference (Figure 1D).
After incising the skin, we will have two flaps, one on the upper base and
the other on the lower base. These flaps will have the same dimensions as
the navel flaps, that is, a base equal to ¼ of the circumference of the
navel and a length equal to half the base.
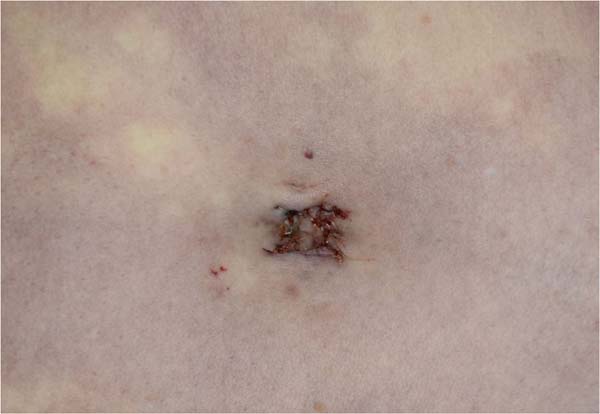
The abdominal wall and umbilicus flaps will be sutured to be perfectly
interposed (Figure 2).
Figure 2 - Appearance at the end of the procedure in right lateral view:
suture of the abdominal wall and umbilicus flaps (preferably
with non-absorbable monofilament thread).
Figure 2 - Appearance at the end of the procedure in right lateral view:
suture of the abdominal wall and umbilicus flaps (preferably
with non-absorbable monofilament thread).
Article inclusion criteria
Articles published in the RBCP and available on its website were included,
describing a proposal for umbilicoplasty, referring to the number of
patients, age, follow-up time, assessment of patient satisfaction, and
complications.
Article exclusion criteria
Articles that performed umbilicoplasty for non-aesthetic purposes, patients
after major weight loss, or did not adequately detail the above data were
excluded.
CEP
The research complies with the Helsinki recommendations and the Research
Ethics Committee (CEP) of the Hospital das Clínicas of the Faculdade de
Medicina de Botucatu, being approved under opinion number 4,961,829.
RESULTS
RBCP Articles
For the sum of the descriptors “omphaloplasty,” “umbilicus,” “neoumbilicus,”
or “umbilicoplasty,” “umbilical scar,” or “neo-omphaloplasty,” 38 articles
were found.
By analyzing the titles and abstracts, 7 articles were excluded, as they
focused on post-great weight loss and pathological alterations of the navel
or mini-abdominoplasty.
Due to the small number of articles that fit the 5 inclusion criteria, we
decided to conduct a qualitative review, allowing the inclusion of articles
with at least three of the five inclusion criteria.
Among those selected for abstract evaluation, 20 articles were excluded for
not including at least three of the following criteria: patients’ age,
follow-up time, description of the technique, complications, and report of
satisfaction; in addition to excluding those that were just case reports or
predominantly included patients after major weight loss.
In the end, 11 articles18-28 were included for full
reading and analysis by two independent researchers (BFMN and LVM), with
only 7 having all five criteria, 1 having four criteria, and 3 having three.
The summary of the data found is in Table 1.
Table 1 - Summary of article data included for full reading and
analysis.
| Article |
No.
of
patients
|
Age |
Time
to
follow-up
|
Satisfaction |
Complications |
| Technique
for umbilicoplasty, avoiding one of the main stigmas of
abdominoplasties18 |
100 |
X |
+ 3
months
|
Full of
patient - 89%;
Full of surgeon -
85%;
Reasonable of patient - 11%;
Reasonable
for the surgeon - 13%;
Patient dissatisfaction - 0%;
Surgeon dissatisfaction - 2%.
|
2 cases -
circular contracture of the new navel (2%).
|
| Routine neo-omphaloplasty in
abdominoplasties19 |
46 |
X |
2 to 19 months |
X |
1 case - erasure of the scar (keloid scar)
(2.1%);
3 cases - dehiscence (6.5%).
|
| Triangular
umbilicoplasty with dermal flap20 |
194 |
X |
X |
188
patients (96.91%) Had
positive
satisfaction;
In 186 cases (95.88%)
the surgeons had positive satisfaction.
|
5 cases -
Epidermolysis in umbilical stump (10.8%);
3 cases -
umbilical narrowing due to scar retraction (6.5%).
|
| Technique with umbilical pedicle in a “kite”
and incision of the skin of the abdomen in a “Y”21 |
31 |
28 and 57 years |
6 months |
bad 0;
reasonable 3.2%;
good
6.5%;
very good 12.9%;
Excellent 77.4%.
|
5 cases - epidermolysis of the stump
(16.1%);
1 case - necrosis of the retail
(3.2%);
3 cases - epidermolysis of creases
(9.6%);
1 case - stenosis stigma (3.2%);
1
case - visible scar (3.2%).
|
| Vertical
incision umbilicoplasty: description of the technique and
evaluation of satisfaction22 |
128 |
25
to
62
years
|
40
months
|
92.2% of
the patients were very satisfied, and the technical
evaluation by the evaluating surgeon attested to a degree of
88.8% satisfaction.
|
2 cases -
umbilical scar suture dehiscence (1.5%);
4 cases -
hypertrophic scar (3.1%);
2 cases - Stenosis
(1.5%);
1 case - umbilicus necrosis (0.7%).
|
| Omphaloplasty: Y/V technique23 |
88 |
27 to
62
years
|
36 months |
It does not explain patient
satisfaction.
|
3 cases - Suture dehiscence in
(3.4%);
1 case - umbilical stenosis (1.13%);
4
cases - chromic alterations of the scar (4.54%);
2
cases - scars with
keloid (2.27%).
|
| Cosmetic and
functional surgery of the umbilicus: transumbilical
plication technique24 |
30 |
26
to
59
years
|
X |
X |
Hassle-free. |
| Omphaloplasty: “infinity” technique25 |
418 |
21 to
73
years
|
120 months |
91% satisfaction. |
9 cases - partial dehiscence (2.1%);
7
cases - stenoses (1.5%);
5 cases - keloids
(1.1%).
|
| Neo-omphaloplasty without a scar26 |
127 |
31 to
50
years
|
4 to 10
months
|
“All
patients monitored and evaluated presented results
considered good by the
themselves and by the
surgeon”.
|
It does
not describe the numbers: partial erasure of the umbilical
depression; epidermolysis of the flap dermis.
|
| Isosceles triangle omphaloplasty with double
fixation in abdominoplasty27 |
97 |
25 to 65
years
|
Up to 12 months |
82.5% if felt very satisfied;
10.3%
satisfied;
7.2% not very satisfied.
|
3 cases - stenoses (3%);
2 cases -
hypertrophic (2%);
2 cases - atrophic (2%).
|
Neo-omphaloplasty with X incision in 401
consecutive abdominoplasties28 |
401 |
23 to
67
years
|
5 to 36
months
|
43
patients rated their result:
67.4% -
Excellent;
23.2% - Very good;
9.3% -
Good.
Evaluation of surgeons:
77%
-Excellent;
18% - Very good;
5% - Good.
|
16 cases -
Infection (3.9%);
11 cases - seroma (2.7%);
6
cases - necrosis (1.5%);
4 cases - hematoma
(1%);
2 cases - dehiscence (0.5%).
|
Table 1 - Summary of article data included for full reading and
analysis.
Due to the lack of standardization and the use of systematic evaluation
methods, it was impossible to carry out statistical analyses regarding the
inclusion criteria.
DISCUSSION
Even after the most varied surgical techniques, Umbilical reconstruction remains
an important challenge for plastic surgeons. Attention should be given to the
umbilical anatomical units and their maintenance or creation - bun, mamelon,
and
umbilical sulcus4,29. For many, the ideal shape
sought is an oval or “T” navel with a vertical orientation of small dimensions,
similar to that of young women22,30.
The absence of anatomical patterns or the presence of distortions, pathological
scarring, and stenosis, among other complications, can lead to dissatisfaction
with the result, in addition to having difficult surgical correction31.
Vernon32 (1957) was the first
surgeon to describe the transposition technique for creating a new navel in
abdominoplasty. The surgery described consisted of a circular technique. Other
authors continued to develop new approaches, but still in circular
scars33. Grazer &
Goldwyn34 (1977), in a
study of 10,574 patients who underwent abdominoplasty, reported that 45% claimed
to have stenosis or cicatricial contracture in the navel. Rosique et
al.35 (2009) reported
a seven times greater chance of these complications when using the
circumferential tactic.
Intending to seek better results, Avelar36 (1978) described a technique with an internal scar by
creating a star-shaped flap, in which the resulting scar presented variation
in
direction, thus reducing complications such as stenosis and cicatricial
retraction. Other techniques based on non-circular scars were developed after
these, but with aesthetic results that are often unsatisfactory11.
Despite the various umbilicoplasty options described in the literature, the
senior author sought an alternative that would provide more satisfactory
results. Thus, in 1998, he published the “H” technique, in which four
rectangular flaps are interposed alternately, and the resulting scar presents
eight 90-degree changes in direction. Thus, the great advantage of this tactic
is the possibility of avoiding tensions and superficializations and being safe
regarding the presence of retractions. Furthermore, the technique allows the
superficializing or deepening of the navel, with the variation of the
perpendicular lines that delimit the flap.
When observed in an orthostatic position, the horizontal scar of the lower flap
is deeply positioned unapparent. The more superficial scars are arranged
longitudinally in the lateral flaps, and to avoid the appearance of these, also
reducing the risk of the navel becoming flat, it must be attached to the
aponeurosis.
Neo-omphaloplasty with the H-shaped technique presents a surgical tactic that
provides a satisfactory aesthetic result with a deeply located horizontal scar,
making it an excellent option in the plastic surgeon’s arsenal (Figures 3 to 5).
Figure 3 - Female patient, 35 years old, 11 years before and after
surgery.
Figure 3 - Female patient, 35 years old, 11 years before and after
surgery.
Figure 4 - Female patient, 29 years old, preand 2 years after
surgery.
Figure 4 - Female patient, 29 years old, preand 2 years after
surgery.
Figure 5 - Female patient, 35 years old, preand 6-month postoperative
period.
Figure 5 - Female patient, 35 years old, preand 6-month postoperative
period.
CONCLUSION
Omphaloplasty in abdominoplasties can be performed in several ways, providing
surgeons with a wide range of alternatives.
The H technique is one of these tools which can be widely used and bring
consistent results.
1. Hospital das Clínicas da Faculdade de Medicina
de Botucatu, Botucatu, SP, Brazil
Corresponding author: Balduino Ferreira de Menezes
Neto Rua Doutor Adolfo Pardini Filho, 1028, Chácara Recreio Vista
Alegre, Botucatu, SP, Brazil, Zip Code: 18608-760, E-mail:
balduinofmneto@gmail.com