INTRODUCTION
Breast ptosis is characterized by liposubstitution of the parenchyma and loss of elasticity
in the skin, the suspensory ligaments of the breasts, and a fall in the nipple-areolar
complex. There are several causes of ptosis, such as pregnancy, lactation, variations
in body weight, developmental deformities, gravity, aging, and the late effect of
silicone implants.
The first publication on the use of prosthesis and mastopexy at the same surgical
time was in 1960 by Gonzales-Ulloa1. In 1968, Dempsey & Latham2 presented the technique of implant inclusion in the retromuscular plane. The article
on the dual plane technique for positioning the breast implant in a concomitant retroglandular
and submuscular space was introduced by Tebetts3 in 2001. Several augmentation mastopexy techniques for correcting ptosis in a single
surgical procedure addressing this issue have been reported in the literature.
Skin sagging and sagging breasts can cause low self-esteem and emotional changes in
patients. The most used classification for breast ptosis was described by Regnault4 and is based on the position of the nipple concerning the inframammary fold. Augmentation
mastopexy elevates the breast tissue and the nipple-areola complex and removes excess
skin associated with silicone implants, seeking to correct asymmetries and preserving
the sensitivity and physiology of the breasts.
Mastopexy with an implant is a challenge for the plastic surgeon, as in the vast majority
of cases, the patient’s aesthetic demands are high in terms of shape, volume, positioning,
quality of the scars, and durability of the results.
Women suffering from severe breast ptosis require further removal due to excess skin
and consequent extensive scarring in the shape of an inverted T. Several authors have
developed techniques with reduced scars, aiming to eliminate the horizontal medial
scar, which can become hypertrophic.
We used the marking based on the Chiari Jr mammoplasty technique with a short scar
at L5,6, initially described for breast reduction and refined over time by the author7.
For patients with mild and moderate degrees of breast ptosis, mastopexy techniques
are used with circumareolar, vertical, or L-shaped scars. Silicone prostheses can
be placed in the retroglandular, subfascial, or dual-plane retromuscular space.
OBJECTIVE
This study aims to describe the experience with the L-enlargement mastopexy technique,
using implants in an anteromuscular or retromuscular dual plane position, and to analyze
the complications.
METHOD
Retrospective study of 123 women with mild to moderate breast ptosis who underwent
L-shaped mastopexy from January 2011 to November 2021. Surgeries were performed on
patients at the private clinic, and Hospital do Servidor Público Municipal de São
Paulo. Paper submitted to the Research Ethics Committee (CEP), with CAAE 54894522.6.0000.5442.
Marking
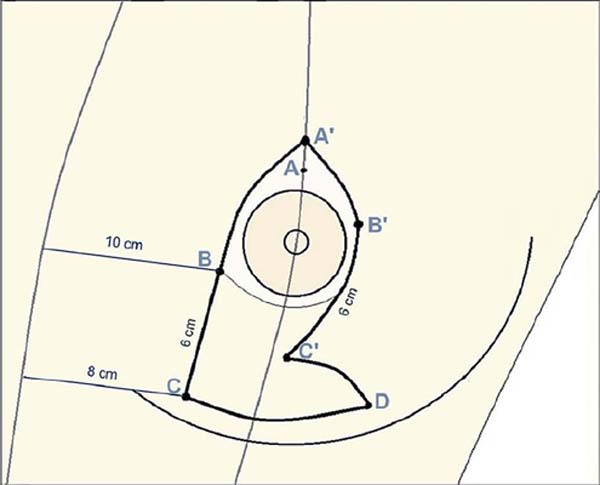
Surgery based on the Chiari Jr technique, whose preoperative marking is shown in Figure 1 and has the following order:
1st Point A’ - the sternal and mid-mammary lines are initially drawn with the patient
in an orthostatic position. Point A is placed in the reflection of the inframammary
fold, and point A’ is positioned 2cm above, usually 17-18cm from the sternal notch.
2nd Point C - with the patient lying down, the breast is pulled laterally, and point
C is defined at a distance of 8cm from the sternal line and 1cm above the inframammary
fold.
3rd Point B - positioned 6cm above point C and 10cm from the sternal line, with the skin
stretched laterally. The BC line delimits the medial column.
4th Point B’ - defined at the level of the nipple and drawn on the lateral margin of
the areola.
5th Point C’ - placed 6cm from point B’ towards C, with the skin stretched medially and
superiorly. Line B’C’ forms the lateral column and is positioned higher than line
BC.
6th Point D – by bringing lines BC and B’C’ closer together, the vertical of the breast
is obtained (6cm), and to remove the inferior cutaneous excess, point D is marked
laterally, 2cm above the inframammary fold. The line CD delimits the horizontal of
the L.
Figure 1 - Preoperative marking based on the Chiari Jr technique.
Figure 1 - Preoperative marking based on the Chiari Jr technique.
Surgical technique
Incision made on the CD line, just above the inframammary fold and prepectoral dieresis
up to the point A’, for placement of the implant in the retroglandular or subfascial
space. For inclusion in the retromuscular plane, a subglandular detachment is performed
up to the lower margin of the areola (dual-plane II), followed by an incision and
divulsion of the pectoralis major muscle and the creation of an inferolateral loop
(Figure 2). Review of hemostasis with luminous valve under direct vision.
Figure 2 - Implants in dual plane retromuscular plane, right and left breasts.
Figure 2 - Implants in dual plane retromuscular plane, right and left breasts.
The nipple-areolar complex has a pedicle with a superomedial base. Removing excess
skin and breast tissue is based on previous marking and bidigital clamping. Construction
of the nipple-areolar complex begins with Benelli’s “round block”8 using polyglecrapone 3.0 thread, followed by continuous intradermal synthesis with
polyglecrapone 4.0 thread. After reviewing the hemostasis, the vertical and horizontal
lines are closed by approximating the subcutaneous tissue with 3.0 nylon thread and
suturing the skin with 4.0 polyglecrapone thread. The mastopexy is completed, and
the scar is reduced to an L shape, as shown in Figure 3.
Figure 3 - L-shaped augmentation mastopexy, immediate postoperative period.
Figure 3 - L-shaped augmentation mastopexy, immediate postoperative period.
RESULTS
In the last ten years, 123 patients were operated on using the augmentation mastopexy
technique with the resulting L- shaped scar. Of these, 113 women (91.9%) were from
the private clinic, and another 10 patients (8.1%) were from the Hospital do Servidor
Público Municipal/SP. The age group ranged from 19 to 64 years, with an average of
35.6 years, and the patients had a body mass index below 30kg/m2 (average body weight
62kg, ranging from 51-83kg).
The breast implants used had a textured surface, round shape, cohesive silicone gel
content, high profile (32.4%), and super high profile (67.6%). The average volume
of 315ml, with a minimum of 175ml and a maximum of 600ml, and in the latter, the prostheses
were exchanged after a previous breast augmentation surgery, according to the medical
evaluation and the patient’s wishes. The implant locations occurred in the dual-plane
retromuscular space (53.5%) and anteromuscular space (46.5%).
Associated liposuction was performed in 14 patients, and an average volume of 1,800ml
of fat was removed. Combined abdominoplasty was performed in 10 patients, with a flap
removed weighing an average of 1,200g. The anesthetic techniques used were general
anesthesia (72.3%), local anesthesia (19.6%), and epidural anesthesia (8.1%). The
average operative time computed was two hours and fifty-four minutes, excluding associated
surgeries.
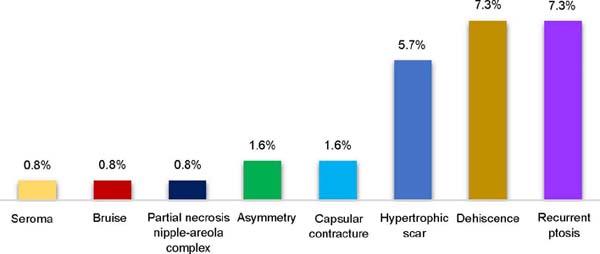
The most frequent complications were superficial dehiscence, which occurred in nine
patients (7.3%), seven cases had unsightly scars (5.7%), two patients developed capsular
contracture (1.6%), two others had breast asymmetry (1.6%), one case of seroma (0.8%),
one case of hematoma (0.8%) and one patient evolved with partial necrosis of the areola
(0.8%). Recurrence of ptosis occurred in nine cases (7.3%). There were no cases of
infection, rupture, or venous thromboembolism (Graph 1). Unaesthetic scarring and ptosis recurrence were the main reasons for reoperations,
which occurred in 12 patients (10.5%). Postoperative follow-up for an average period
of two years.
Graph 1 - Incidence of postoperative complications.
Graph 1 - Incidence of postoperative complications.
DISCUSSION
There is a considerable rate of dissatisfaction with sagging in the late postoperative
period, identified in the reduction of the upper pole and excess tissue in the lower
pole, in addition to small dehiscence and cicatricial enlargement. Several authors
have published techniques related to the anatomical positioning of the prosthesis,
with low rates of complications.
Calobrace et al.9 reported a revision rate of 23.2% in 332 cases of augmentation mastopexy. The most
reported complications were capsular contracture (3.9%), scarring (3.3%), and ptosis
recurrence (3.3%).
Stevens et al.10 published reoperation rates of 16.9% in 615 patients undergoing mastopexy with an
implant. The most common complications were healing (5.7%) and dehiscence (2.9%).
A meta-analysis study in 2014, carried out by Khavanin et al.11, of 4,856 augmentation mastopexies found rates of reoperations (10.6%), recurrent
ptosis (5.2%), unsightly scars (3.7 %), capsular contracture (2.9%), asymmetry (2.9%),
seroma (1.4%), hematoma (1.4%) and infection (0.9%).
Ono & Karner12, in 2018, published the mastopexy technique and implants in a submuscular pocket
and inferolateral loop, superomedial pedicle, and resection of the breast parenchyma.
Reoperation rate of 16% in 266 patients but reduced to less than 5% according to the
learning curve. Inferolateral muscle support is used to prevent the recurrence of
ptosis.
In the article on the submuscular double-pocket implant for augmentation mastopexy,
published by Procópio et al.13, of the 80 operated cases, there were reoperations (6.1%), epitheliolysis at the
junction of the vertical and horizontal scars (2.5%), hematoma (1.3%), capsular contracture
(1.3%) and seroma (1.3%).
Graça Neto & Daniel14 present the original technique of muscle support in the lower pole of the breast,
where the implant is placed in a double space, with the lower part of the prosthesis
retromuscular and the upper part in the subglandular plane. Out of 640 operated patients,
the main complications were excess skin (3%), unsightly scars (3%), and partial necrosis
of the areola (2%).
Sgarbi et al.15 reported 21 complications (22.8%) in 192 patients who underwent the mastopexy technique
with the splitting of the upper pectoral muscle and lower muscle band, seroma (3.6%),
unsightly scars (2.6%), breast asymmetries (2.6%) and suffering from nipple-areola
complex (1.5%) were the observed complications.
In the present study, several women had the implants placed in the retroglandular
space under an inferior muscular belt, following the approach described by Daniel.
There is a current tendency to place the prosthesis in a dual-plane retromuscular
space, which offers better coverage and vascularization, provides low rates of capsular
contracture, lower rates of visualization or palpation of the implant (“rippling”)
together with the elaboration of the inferolateral pectoral loop, the technique disclosed
by Ono, which provides muscle support and less implant migration.
To reduce the incidence of postoperative pseudoptosis, complete the length of the
vertical scar at 6 cm. The excess skin on the lower pole of the breast is removed,
leaving an L-shaped final scar.
Most of the women in this study had symmetrical breasts with adequate volume and shape
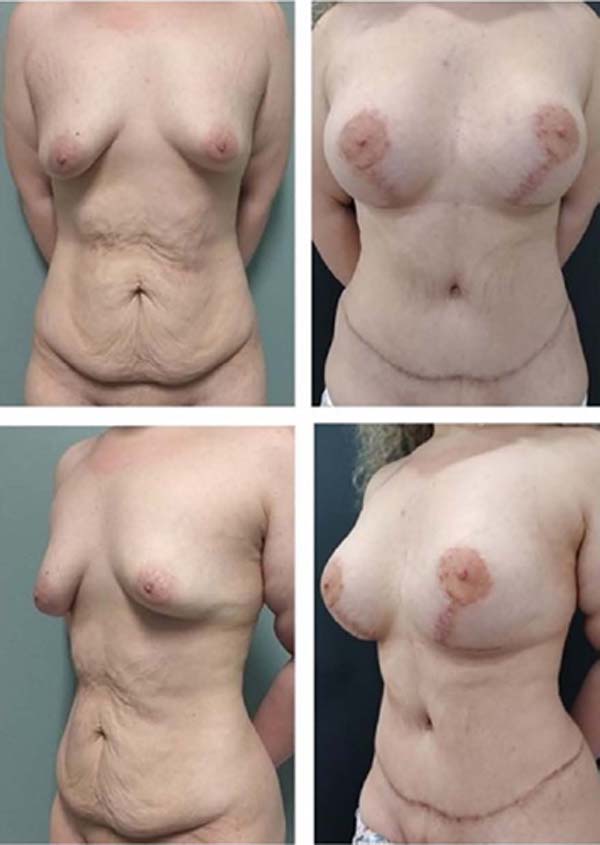
(Figures 4, 5, 6, 7, 8, 9). The continuous improvement of technique and the excellence of the surgeon favor
the success of the operation16.
Figure 4 - Patient 24 years old, immediate postoperative period (350ml, retroglandular).
Figure 4 - Patient 24 years old, immediate postoperative period (350ml, retroglandular).
Figure 5 - Patient 43 years old, immediate postoperative period (300ml, retromuscular dual-plane).
Figure 5 - Patient 43 years old, immediate postoperative period (300ml, retromuscular dual-plane).
Figure 6 - Patient 27 years old, 12th month after surgery - L-shaped mastopexy (375ml, retroglandular).
Figure 6 - Patient 27 years old, 12th month after surgery - L-shaped mastopexy (375ml, retroglandular).
Figure 7 - 31-year-old patient, ninth month after surgery - L augmentation mastopexy (330ml,
dual-plane retromuscular).
Figure 7 - 31-year-old patient, ninth month after surgery - L augmentation mastopexy (330ml,
dual-plane retromuscular).
Figure 8 - 34-year-old patient, third month after surgery - liposculpture and L-shaped mastopexy
(295ml, retroglandular).
Figure 8 - 34-year-old patient, third month after surgery - liposculpture and L-shaped mastopexy
(295ml, retroglandular).
Figure 9 - Patient 22 years old, 12th month after surgery - abdominoplasty and L-shaped augmentation
mastopexy (480ml, dual-plane retromuscular).
Figure 9 - Patient 22 years old, 12th month after surgery - abdominoplasty and L-shaped augmentation
mastopexy (480ml, dual-plane retromuscular).
CONCLUSION
L-mastopexy is safe and reproducible, with complication rates consistent with the
literature. This technique effectively corrected mild to moderate ptosis, promoting
projected breasts with well-positioned and reduced scars.
2. Hospital do Servidor Público Municipal, Preceptor de Residência em Cirurgia Plástica,
São Paulo, SP, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, Membro Titular, São Paulo, SP, Brazil
Corresponding author: Roberto Luiz Sodré Rua Antonio Alves Barril, 355/191, J. Anália Franco, São Paulo, S P, Brazil. Zip
code: 03338-000 E-mail: roberto.sodre@uol.com.br