INTRODUCTION
Reduction mammoplasty is one of the most common plastic surgeries in the world. According
to data from the American Society of Plastic Surgeons, there were more than 40,000
procedures in the United States in 20181.
Unlike many surgical procedures, reduction mammoplasty has a long and established
history. Since the end of the 19th century and the beginning of the 20th century, numerous techniques have been described
for breast tissue reduction, seeking the best aesthetic result and greater safety
in terms of vascularization and areolar innervation2. Thorek, in 1922, described amputation of the lower pole of the breast and free graft
from the nipple3.
In 1956, when introducing his standard skin resection, Wise4 used preoperative marking, geometric parenchymal resections, and positioning of the
nipple- areolar complex (NAC). Wise’s model has become one of the most popular techniques
to date2.
The 1960s and 1970s presented several options to improve the pedicle in reduction
mammoplasty2. Strombeck5, in 1960, used a bipedicled horizontal flap to maintain the nipple-areola complex,
based on the medial and lateral perforators for perfusion associated with the dermoglandular
pedicle described by Schwartzman around 19306. The superolateral dermoglandular pedicle was described by Skoog7 in 1963, while Pitanguy and Weiner described the dermoglandular pedicle based on
the superior pedicle about 10 years later, in 19738. McKissock9,10, a year earlier, transformed Strombeck’s horizontal bipedicular technique into a
vertical bipedicular technique.
Many other surgeons worldwide began to develop reduction mammoplasty techniques using
a small scar and based on the superior pedicle throughout the 1980s and 1990s2.
Despite the various studies and techniques described in the literature that address
reduction mammoplasty, there is a lack of current studies that describe procedures
that use two or more pedicles to reduce breast tissue, as well as consistent results,
success rates, and complications1.
The purpose of this study is to describe a new technique for bipedicled and structured
reduction mammoplasty: safe, mainly due to greater preservation of breast irrigation,
easy understanding and reproducibility, low learning curve, and promising aesthetic
results. Furthermore, above all, maintaining the natural shape of the breast brings
satisfaction to patients.
OBJECTIVE
To present and describe a new bipedicled and structured mammoplasty technique for
treating breast tissue excess, flaccidity, and ptosis that is easily reproducible,
simple, safe, and efficient.
METHOD
As of January 2015, the authors began to use the technique described below in their
mammoplasties, with a progressive increase in the frequency of its use. As of 2016,
they started to use the technique in all their cases of mastopexy without prosthesis
and reduction mammoplasty.
From January 2015 to August 2021, 86 patients underwent surgical treatment of mammoplasty
using the technique in question. During this period, the authors performed the technique
in clinical and hospital settings. Patients who required the use of silicone implants
were excluded from the data analysis.
The analysis of the cases was carried out retrospectively through analysis of medical
records and review of pre- and postoperative photographs. The elaboration of the article
followed the principles of Helsinki.
The volume removed from each breast ranged from zero grams to 1200 grams. The rise
of the nipple- areolar complex ranged from 3 to 15 cm, with the marking of point A
showing a mean distance to the sternal notch of 19.6 cm.
Technique description
The structured bipedicle mammoplasty technique basically consists of dividing the
breast into three parts – which we will call pillars. Thus, the breast is divided
into a lateral pillar (L), a medial pillar (M), and an intermediate pillar (I). In
this sense, the intermediate portion will be fixed and structured through suture points.
The lateral and medial will similarly involve the intermediate, which is already structured.
Marking: we marked the rise of the nipple-areola complex using a bidigital maneuver
and Strombeck- Wise molds5. We believe that the type of reduction mammoplasty marking used is not influential
in the technique.
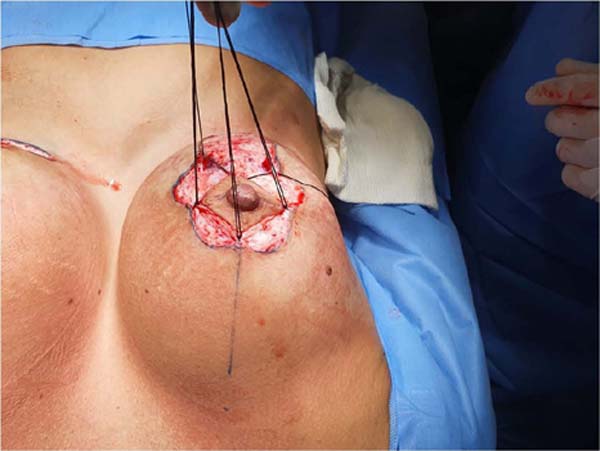
The surgery begins with periareolar de - epidermization, according to Schwartzman6, preserving the innervation and circulation coming from the subdermal plexus, and
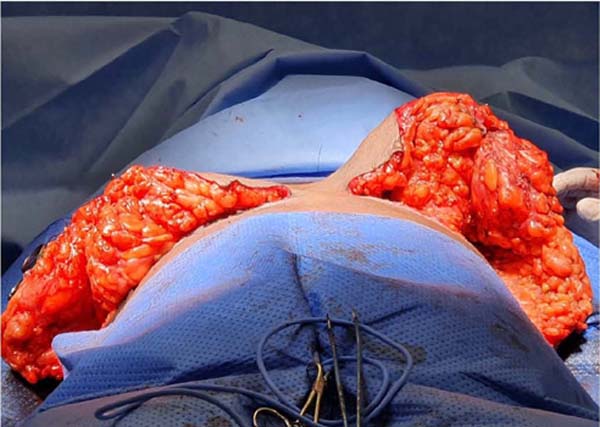
the superior pedicle areolar flap described by Pitanguy8 is made (Figure 1).
Figure 1 - De-epidermization.
Figure 1 - De-epidermization.
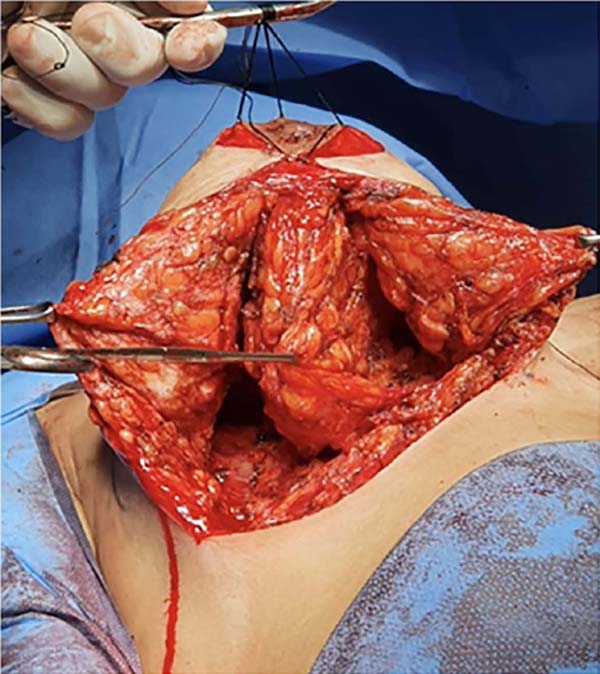
Next, a transverse incision is made 3 cm caudal to the areola, joining the other two
longitudinal incisions in this caudal ptosed flap to be resected. These incisions
go down to the base of the breast in the inferior mammary fold. At this moment, the
entire lower pole exceeding the breast is resected when there are excesses or if you
want to reduce the volume (Figure 2). The retroglandular detachment must be limited to the inframammary region and not
reach the fifth intercostal space cranially. Thus, the central (or glandular) pedicle
containing the intercostal perforating arteries is preserved to irrigate the nipple-
areolar complex. In addition, the fourth intercostal nerve, which is of fundamental
importance for NAC sensitivity, is preserved11. What remains is a single block running from the clavicular musculature to the fifth
intercostal space.
Figure 2 - Lower pole resected.
Figure 2 - Lower pole resected.
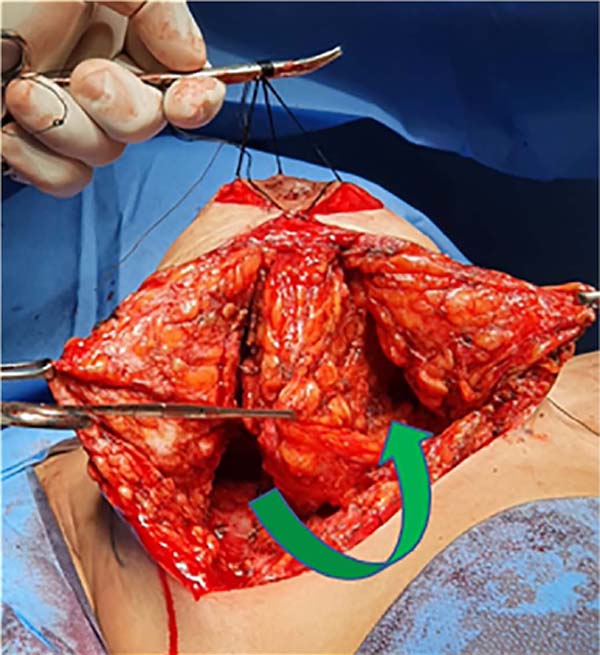
This block will then be divided longitudinally into three parts, three flaps, through
two incisions, resulting in a lateral, medial, and intermediate block (Figure 3). This retroareolar intermediate block should be close to the width of the areola
(between 3 and 5 cm). The two incisions that will divide this mammary block into three
must have the depth of the entire mammary gland, reaching the subcutaneous fat close
to the skin (approximately 2 cm). With this, the medial and lateral pillars are released,
subsequently involving the intermediate pillar.
Figure 3 - Breast divided into three pillars.
Figure 3 - Breast divided into three pillars.
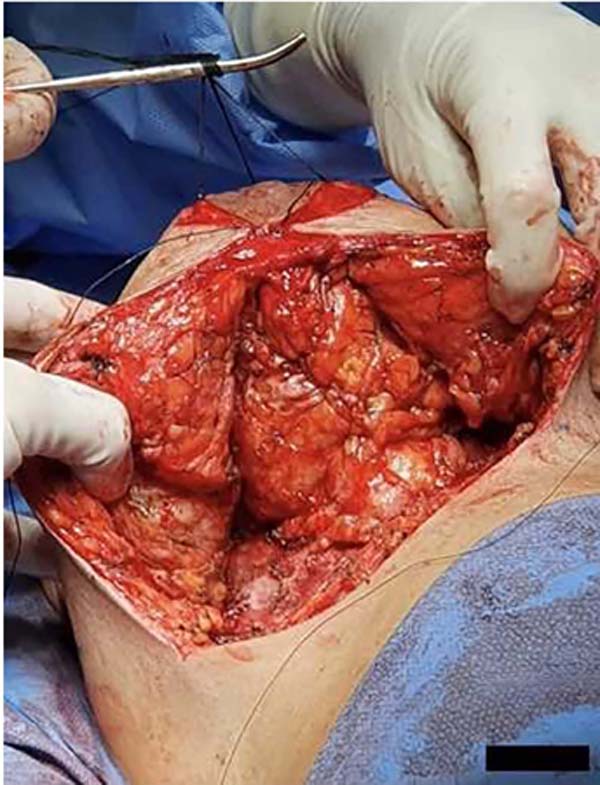
At that moment, the breast can be modeled by reducing or not the medial and lateral
pillars, defining the desired projection of the breast (Figure 4). The intermediate abutment must not be reduced or devascularized. Once the necessary
reduction has been made on the lateral and medial pillars, the intermediate pillar
is modeled and structured – which is pedicled on the perforating arteries of the thorax
up to the nipple- areola complex. Thus, in practical terms, the nipple- areolar complex
will be irrigated superiorly by the subdermal plexus and superior pedicle and inferiorly
by the inferior pedicle, therefore being bipedicled11.
Figure 4 - Three pillars after resection of excess tissue in the medial and lateral pillars.
Figure 4 - Three pillars after resection of excess tissue in the medial and lateral pillars.
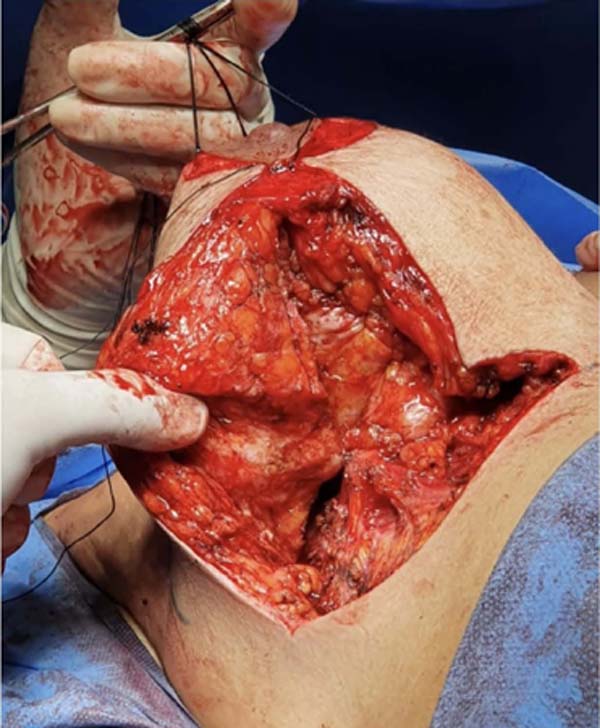
Starting from the nipple-areola complex and towards the pectoral muscle, we measured
the desired length of the intermediate pillar. In this location, the lateral border
of the intermediate pillar is fixed, through suture, to the pectoral muscle in the
most cranial part possible of the incision made for the division of the breast (Figure 5). Other points at the base of the intermediate pillar can be given for greater fixation
of the same to the muscle, tensioning and fixing it medially.
Figure 5 - Traction and fixation of the intermediate flap to the medial region of the breast.
Figure 5 - Traction and fixation of the intermediate flap to the medial region of the breast.
Until this moment, the three pillars are still not structured, and the breast has
not reached the desired shape and support. For this reason, some X-shaped sutures
will be made, joining the lateral and medial edges of the intermediate pillar, making
its tubular shape like a cigar (Figure 6). Thus, the successive tensioning sutures promote stiffening of the intermediate
pillar, ensuring the greatest breast projection obtained with this technique (Figures 7, 9, and 10).
Figure 6 - X points on the intermediate pillar.
Figure 6 - X points on the intermediate pillar.
Figure 7 - Breast projection obtained after successive tension sutures of the intermediate pillar
(above). Aspect of the breast before the X sutures (below).
Figure 7 - Breast projection obtained after successive tension sutures of the intermediate pillar
(above). Aspect of the breast before the X sutures (below).
Figure 9 - Structured left breast.
Figure 9 - Structured left breast.
The next and last step of the surgery will be to pull the medial and lateral pillars
towards the mammary sulcus, involving the pedicled and reinforced intermediate tubular
pillar. Then, the lateral and medial pillars are advancement flaps that will be pulled
toward the submammary crease. This traction must be fixed with Baroudi-type 12 adhesion
points throughout its base, avoiding lateral and medial dead space and dispensing
with drains13 (Figure 8).
Figure 8 - Advancement of the medial and lateral flaps involving the intermediate pillar.
Figure 8 - Advancement of the medial and lateral flaps involving the intermediate pillar.
The closure of the skin and the finishing of the areolas can be done as usual by the
surgeon.
RESULTS
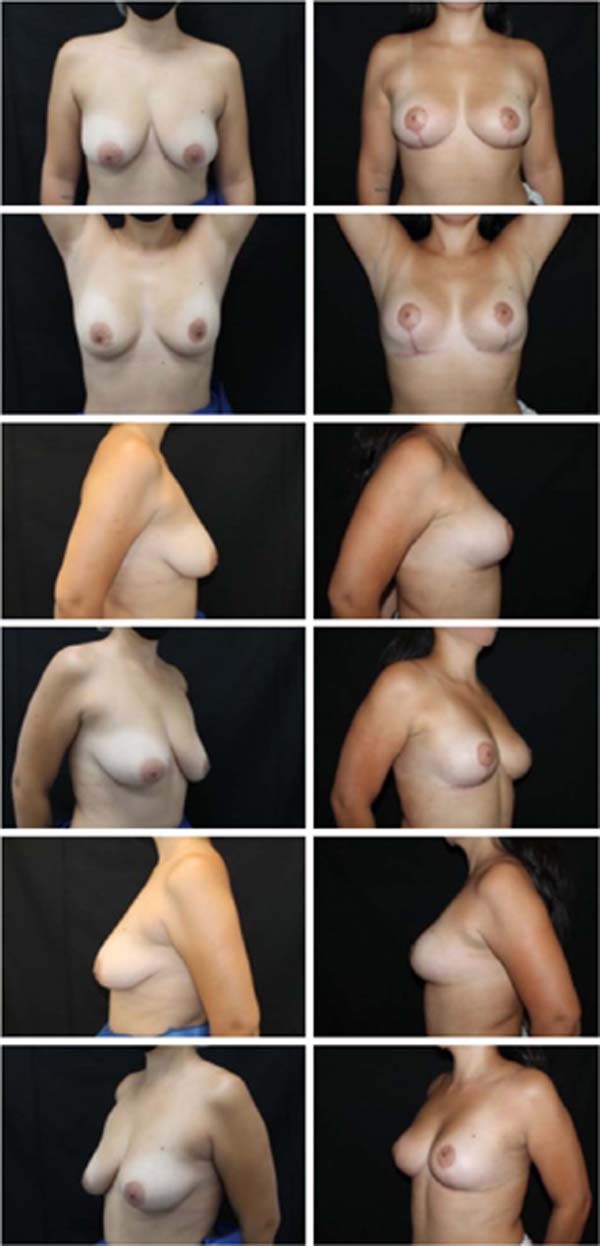
The authors examined results through in-office clinical evaluations and the analysis
of standardized preoperative and postoperative photographs at one, six, and twelve
months. From an aesthetic point of view, there was a clear improvement in the shape
and consistency of the breasts. Subjectively, the aesthetic result was maintained
throughout the follow-up period of these patients. The increase in patient satisfaction
with the techniques previously used by the authors was also clinically remarkable.
The complication rate was below the average described in the literature14. Of the
86 operated cases, 14 patients had some complication, with 4 suture dehiscence (4.6%)
and 9 occurrences of seroma (9.6%), all treated uneventfully conservatively or with
a single puncture in the office. There was no occurrence of hematomas that required
drainage, surgical or not.
There was also no necrosis of skin flaps, the nipple-areola complex, or ischemic suffering
requiring complementary therapy. There was no increase in the rate of other complications,
such as infections and sensitivity changes, compared with rates of already established
techniques2,14. These numbers allow us to state that this is an extremely safe technique compared
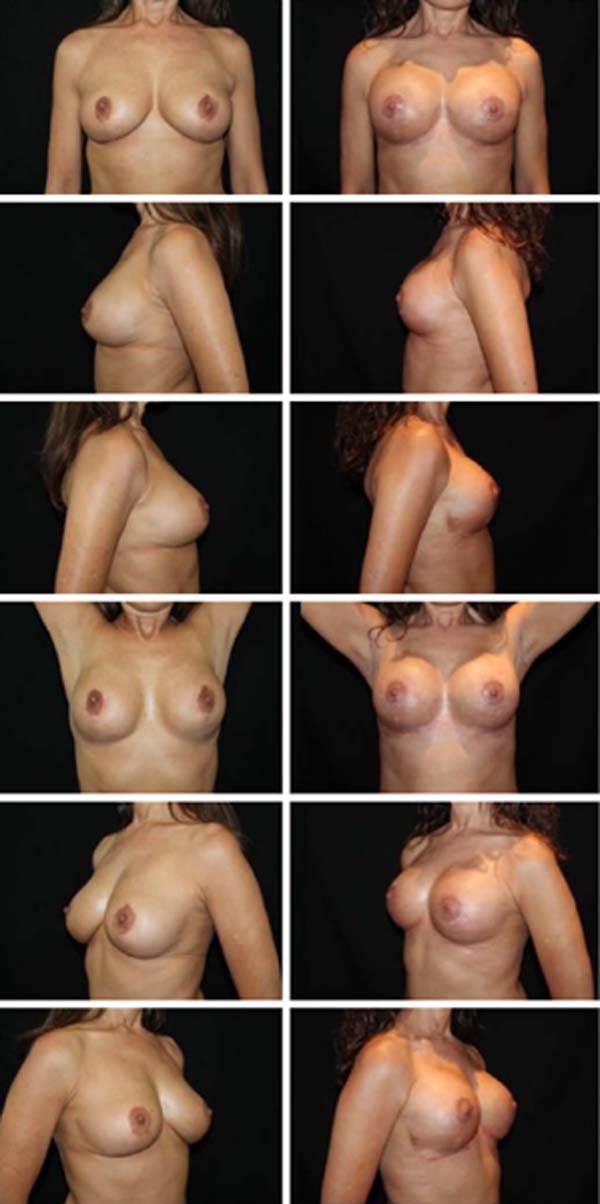
to already established mammoplasty techniques (Figures 11, 12, 13, 14, 15, 16, 17).
Figure 11 - Pre and postoperative 4 months.
Figure 11 - Pre and postoperative 4 months.
Figure 12 - Pre and postoperative 4 months.
Figure 12 - Pre and postoperative 4 months.
Figure 13 - Pre and postoperative 5 months.
Figure 13 - Pre and postoperative 5 months.
Figure 14 - Pre and postoperative 5 months.
Figure 14 - Pre and postoperative 5 months.
Figure 15 - Pre and postoperative 6 months.
Figure 15 - Pre and postoperative 6 months.
Figure 16 - Pre and postoperative 6 months.
Figure 16 - Pre and postoperative 6 months.
Figure 17 - Pre and postoperative 6 months.
Figure 17 - Pre and postoperative 6 months.
DISCUSSION
Numerous surgical techniques are described for treating the breasts, many of which
are highly acclaimed by Brazilian authors, such as the techniques by Pitanguy8 and Liacyr Ribeiro15.
Some authors already presented bipedicled techniques for mammoplasty, such as McKissock9, in 1972. However, we observed a scarcity of techniques based on double pedicles
in the literature.
A systematic review carried out by Wirthmann et al.16 in 2018 showed a rate of complications related to reduction mammoplasties of 33%,
and if minor complications that do not involve the need for any reintervention are
disregarded, the incidence drops to 9.5%. The most common ones observed were dehiscence
and delayed healing of surgical wounds, followed by hematomas. Necrosis of the nipple-areola
complex, feared mainly in large reductions and large fixations, had an incidence of
0.7%, all of which were partial16.
The risk of areola necrosis leads the surgeon to prioritize safety when choosing the
technique14. Therefore, the vascular pedicles of the chosen flaps will define which surgical
technique will be used. The greater the number and the better the quality of the pedicles,
the safer the technique will be11. Based on this principle, the authors believe that a bipedicled technique brings
greater safety than a single pedicle, whether superior or inferior.
The technique described here is based on a double pedicle, being a superior areolar
pedicle, with irrigation coming from the subdermal plexus preserved around the entire
areola, in addition to an inferior pedicle, based on the preservation of the main
perforators of the thoracic muscles, branches of the internal thoracic arteries and
external, from the first to fourth intercostal spaces11. The presence of multiple sources of irrigation for the nipple-areola complex ensures
superior safety concerning the vitality of breast tissues14,17,18,19,20,21.
Concerning the innervation of the nipple-areolar complex, the technique provides greater
neuronal supply through the superior, subdermal and periareolar pedicle and by preserving
the intercostal nerve in the intermediate pillar of the inferior pedicle11.
Another fact that contributes to the safety and prevention of complications is the
fact that the lateral and medial pillars are fixed to the thoracic muscles using Baroudi
stitches12, reducing dead space in such a way that it significantly reduces the risk of seromas
and hematomas, eliminating the need for the use of drains13.
In addition to the increased safety associated with the technique, the authors believe
that another important advantage is the possibility of greater breast structuring,
with results demonstrating increased consistency and improved shape and contour, with
the upper poles becoming more filled without silicone prostheses.
Moreover, it is an easily reproducible technique, with simplicity to perform, a small
learning curve, and reducing surgical time compared to other reduction mammoplasty
techniques22. It is a versatile technique that can be used both in large breast reductions and
in large fixations that do not require the removal of breast tissue.
CONCLUSION
The mammoplasty technique presented here is an innovative proposal that has been carried
out since 2015. During this period, 86 patients underwent surgery using the bipedicled
and structured mammoplasty technique, with a low rate of complications, most of which
were minor. The double pedicle provides great security for preserving the vascularization
and innervation of the nipple-areola complex, with no case of necrosis associated
with the technique to date. The aesthetic result was surprising, with long- lasting
projection and support. Moreover, it is a highly reproducible technique, easy to perform,
highly applicable, and versatile, in addition to extremely satisfactory aesthetic
and functional results for both surgeon and patient.
1. Hospital da Plástica Contorno, Belo Horizonte, MG, Brazil.
2. Hospital Felício Rocho, Belo Horizonte, MG, Brazil.
3. Núcleo de Cirurgia Plástica, Belo Horizonte, MG, Brazil.
4. Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil.
Corresponding author: Victor Izidro Alves de Almeida Avenida do Contorno, 6975, Santa Efigênia, Belo Horizonte, MG, Brazil. Zip code:
30110-076 E-mail: izidrodealmeida1@gmail.com