

Case Report - Year 2023 - Volume 38 -
Diagnosis, evolution and treatment of a patient with pyomyositis
Diagnóstico, evolução e tratamento de paciente com piomiosite
ABSTRACT
Pyomyositis is a deep muscle infection of bacterial origin and subacute, which can evolve with multiple intramuscular abscesses. Despite being characterized as an affection of tropical zones, its incidence in temperate zones has been increasing due to immunosuppression factors, such as infection by the human immunodeficiency virus (HIV) and some types of immunosuppressive treatments. Even though it has been known for over a century, it is a rare and potentially serious condition that can lead to septic shock and death. This is a case report of a descriptive nature, which found the relevance of knowledge about this condition for an early diagnosis, enabling positive prognostic repercussions.
Keywords: Pyomyositis; Staphylococcal infections; COVID-19; Staphylococcus aureus Muscle, skeleton
RESUMO
A piomiosite é uma infecção muscular profunda, de origem bacteriana e caráter subagudo, que pode evoluir com abcessos intramusculares múltiplos. Apesar de ser caracterizada como uma afecção de zonas tropicais, sua incidência em zonas temperadas vem aumentando por fatores de imunossupressão, como a infecção pelo vírus da imunodeficiência humana (HIV) e alguns tipos de tratamentos imunossupressivos. Mesmo sendo conhecida há mais de um século, é uma condição rara e potencialmente grave, podendo levar ao choque séptico e óbito. Trata-se de um relato de caso de caráter descritivo, que constatou a relevância do conhecimento desta afecção para um diagnóstico precoce, possibilitando repercussões prognósticas positivas.
Palavras-chave: Piomiosite; Infecções estafilocócicas; COVID-19; Staphylococcus aureus; Músculo esquelético
INTRODUCTION
Pyomyositis is defined as a primary acute bacterial infection of the skeletal muscles, with Staphylococcus aureus as the main etiological agent. Its pathogenesis is believed to be related to a previous history of local trauma, with consequent transient bacteremia and dissemination to large muscle groups, predominantly in the lower limbs1.
In epidemiological terms, the disease has a higher prevalence in males, in the first two decades of life, with a ratio of 1.5 men for each woman2, and in tropical regions. However, there is a growing number of cases in temperate zones due to infection by the human immunodeficiency virus (HIV) or by immunosuppressive treatments3. Mortality ranges from 1 to 23%4.
Three stages are correlated in the clinical manifestation of pyomyositis: the first stage, which corresponds to bacterial invasion of the muscle, causing signs and symptoms such as low-grade fever, anorexia, localized pain, edema, contraction and limitation of muscle mobility; the second stage corresponds to the suppurative phase, in which there is the formation of abscesses with exacerbation of phlogistic signs and high fever. Without a diagnosis, the disease progresses to the septic phase (third stage), with systemic dissemination of the infection5.
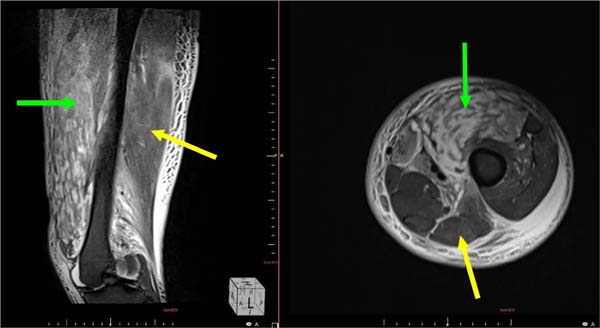
The diagnosis is basically established by imaging tests, with magnetic resonance imaging being the most sensitive method for analyzing muscle damage. In more limited methods, such as X-rays, there is evidence of soft tissue enlargement, and in ultrasonography, hyperechogenicity is observed, indicative of edema and muscle necrosis. Computed tomography shows muscle edema and fluid collections. For etiological diagnosis, blood cultures and/or cultures of drained or aspirated material are performed5. Clinically, the diagnosis is difficult and delayed due to its nonspecific signs, leading to potentially fatal consequences2.
Treatment consists of antibiotic therapy in the first stage or associated with a surgical approach in the following stages, usually lasting about 3 to 6 weeks. Oxacillin is a good option for S. aureus infection; however, the chosen antibiotics may vary according to the culture result.
This article aims to conduct a clinical analysis of the surgical approach adopted in a case of pyomyositis in a 21-year-old patient admitted with pain and edema in the lower limbs in a tertiary hospital in the interior of Minas Gerais.
CASE REPORT
FJJE, 21 years old male, previously healthy, denied the use of drugs or injectable medication, admitted in February 2021 to the emergency room of the Hospital de Clínicas of the Federal University of Triângulo Mineiro, in Uberaba, with a clinical picture of moderate, intermittent pain, in both lower limbs, associated with swelling and fever for 3 days. Patient with a history of strenuous physical activity and trauma to the lower limbs during a soccer match a week ago. He previously sought medical attention, was treated with symptomatic drugs, and was released to his home.
On physical examination, he presented a decline in general condition, fever, difficulty walking, and significant edema in the lower limbs, mainly on the left side. There was local heat and stiffness on palpation.
Doppler ultrasonography and magnetic resonance imaging showed multiple abscesses in the thigh’s anterior and posterior muscle groups and the gastrocnemius muscle’s topography. No signs of deep venous thrombosis were observed (Figure 1).
The patient was admitted to the care of the Internal Medicine and Orthopedics teams. He required four debridements in the operating room and used culture-guided intravenous antibiotic therapy that showed the growth of methicillin-resistant Staphylococcus aureus (MRSA) (Figure 2).
During the 15th day of hospitalization, the patient underwent a rapid test for the COVID-19 virus, with a positive result. Fortunately, he evolved with only mild respiratory symptoms. He remained in respiratory isolation for 15 days and used symptomatic drugs.
After releasing the respiratory isolation, the lesions looked good, granulated, superficial, and without infectious characteristics. Thus, the patient was referred for definitive treatment by the Plastic Surgery team (Figure 3).
It was decided to perform a partial skin graft removed with an electric dermatome, using intact areas in the lower limbs as donors and performing a non-adherent occlusive dressing.
The patient had excellent graft integration and was discharged one week after surgery, with outpatient follow-up by the Plastic Surgery and Physiotherapy teams. Late postoperative follow-up showed complete motor rehabilitation (Figure 4).
DISCUSSION
Epidemiological issues, such as origin, age and sex, and the manifestation of reported signs and symptoms corroborate the data shown in the literature; however, the patient in question did not present immunosuppression factors prior to the event or known history of drug use or injectable medication, unlike the observed series6,7,8,9.
The main impasses of pyomyositis include its rarity and clinical diagnostic difficulty, which result in late and often ineffective treatments.
The differential diagnosis includes costochondritis, osteomyelitis, thrombophlebitis, and deep vein thrombosis4. The gold standard imaging test is magnetic resonance imaging, which allows the detection of fluid collections and muscle edema more accurately.
The treatment and the need for a surgical approach are analyzed according to the culture results and the stage of the disease. In this case, multiple purulent collections and extensive lesions made serial surgical intervention and subsequent reconstruction with a partial skin graft imperative.
CONCLUSION
Concerning the diagnosis of uncommon diseases, in the clinical practice of plastic surgeons, diagnostic suspicion is only possible when there is prior knowledge of the condition. That said, the importance of familiarizing the professional with pyomyositis should be emphasized, since early diagnosis and correct treatment, used promptly, greatly alter the patient’s prognosis. Furthermore, on the other hand, the delay in diagnosis can lead to disastrous consequences, with injuries of high morbidity to the patient, which may even culminate in the death of the patient whose diagnosis was inadvertently neglected.
Therefore, specific imaging tests must be promptly requested because of the suspicion of this disease. A multidisciplinary team, acting coordinated, must manage the case so that the correct diagnosis allows for early treatment and a favorable evolution.
1. Universidade Federal do Triângulo Mineiro, Hospital de Clínicas, Cirurgia Plástica,
Uberaba, Minas Gerais, Brazil
2. Universidade Federal do Triângulo Mineiro, Medicina, Uberaba, Minas Gerais, Brazil
Corresponding author: Larissa Figueiredo Vieira Rua Vigário Silva, 695/804, Bairro Bom Retiro, Uberaba, MG, Brazil. Zip code: 38022-190 E-mail: larissafvieira31@hotmail.com










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter