INTRODUCTION
High-energy trauma has increased significantly in recent decades, mainly due to motorcycle
and car accidents. Trauma victims may present varying severity and location injuries,
with the lower limbs being an important and common site affected. These can range
from simple skin continuity solutions to major tissue loss and exposure of noble structures1,2.
The decision for the technique to be used is essential for successful reconstruction,
and, based on the principle that the best repair is always the simplest3, the fundamentals of reconstructive surgery were created. Therefore, primary wound
closure is the first choice whenever possible.
However, in wounds with great loss of soft tissues, or when decompressive fasciotomy
of the limbs is performed with local skin retraction and muscle protrusion, there
is difficulty in performing such closure. Several alternatives are proposed for the
closure of the extremity wound, such as grafts, flaps, elastic sutures, adhesive tapes,
and plastic clamps, the former being able to be associated with the vacuum dressing.
Within this context, closure through intermittent traction with Kirschner wires and
steel wires becomes a viable, inexpensive, low-morbidity option, avoiding new scars
created by flap rotation that can result in retraction, ischemia, and tissue necrosis4,5, and being easy to reproduce for closing numerous limb wounds, as well as fasciotomies.
OBJECTIVE
The present study evaluates the closure of a post-trauma lower limb wound with local
fasciotomy, through continuous and intermittent traction with a Kirschner wire associated
with steel wires, as an alternative for highly complex injuries.
CASE REPORT
This is a retrospective, observational study of a patient who underwent fasciotomy
closure through dermatotraction with steel wire at the Hospital do Trabalhador, in
Curitiba-PR, in 2020. Study approved by the Research Ethics Committee, under CAAE
52788221.0.0000.5225.
Patient LFMP, male, 26 years old, previously healthy, comes to the emergency room
at the Hospital do Trabalhador in Curitiba with a history of a fall from the same
level into a maintenance hole, with consequent dislocation of the left knee joint.
He preserved the posterior tibial artery, popliteal artery pulses, and anterior tibial
artery pulse on admission. He was referred to the surgical center for dislocation
reduction by the Orthopedics team. In the immediate postoperative period of transarticular
external fixation, there was a slowdown in capillary refill time, the temperature
difference concerning the contralateral limb, and difficulty in palpating pulses.
An assessment by the Vascular Surgery team was then requested, which on physical examination
of the patient, found the absence of anterior tibial, posterior tibial, and popliteal
pulse, pain on palpation of the calf, and decreased movement of the toes. Angiotomography
was performed, which confirmed a lesion in the popliteal artery, and the patient was
taken back to the surgical center for revascularization of the limb, with interposition
of the popliteal artery with the reverse saphenous vein and medial and lateral fasciotomy.
During the postoperative period, the patient evolved with signs of reperfusion syndrome
and was referred to the Intensive Care Unit (ICU). After 4 days, he was discharged
from the ICU, maintaining decreased foot sensitivity and absent motricity in the toes
and forefoot. Anterior and posterior tibial pulses are present, without popliteal
pulse attributed to edema. Fluxes present on Doppler.
On the tenth postoperative day, the patient started with a fever, progressing to blisters
and hallux necrosis. Ultrasonography was performed, which identified the presence
of a collection in the distal third of the wound, which was drained with a large number
of clots and a purulent collection. Subsequently, he was submitted to successive debridements
of devitalized tissues due to muscle necrosis in the deep posterior compartment, interosseous
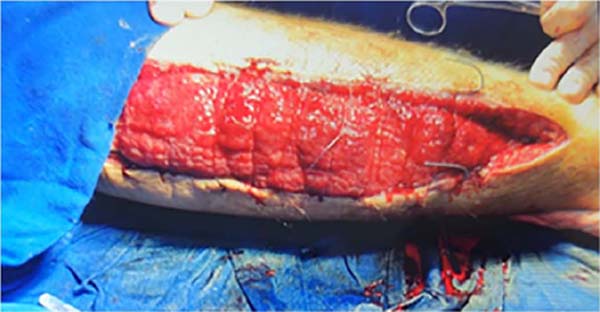
membrane, and anterior compartment (Figure 1).
Figure 1 - Patient in the postoperative period of fasciotomy (photo taken by the assistant team).
Figure 1 - Patient in the postoperative period of fasciotomy (photo taken by the assistant team).
An evaluation was requested after the patient’s first vacuum dressing to monitor the
condition, assessing the lesion (Figure 2) and indicating the approximation of the edges with 1.5 Kirschner wires in association
with the twisting of 0 steel wires (Figure 3) in association with the dressing vacuum for drainage of secretion and approximation
of borders. Four sessions were performed to approximate the edges by twisting the
steel wires (Figure 4), all in a surgical center under spinal anesthesia; the mean interval between procedures
was 3 days. Ultimately, the surgical wound was completely resolved with the proposed
treatment (Figure 5), without grafts, flaps, or other procedures, ending the procedure with a primary
suture of the lesion.
Figure 2 - Patient in the postoperative period of debridement of the lesion in association with
a vacuum dressing (photo taken by the assistant team).
Figure 2 - Patient in the postoperative period of debridement of the lesion in association with
a vacuum dressing (photo taken by the assistant team).
Figure 3 - Patient in the postoperative period of insertion of 1.5 Kirschner wires and 0 steel
wires.
Figure 3 - Patient in the postoperative period of insertion of 1.5 Kirschner wires and 0 steel
wires.
Figure 4 - Patient in the postoperative period of steel wire traction, photo in medial and lateral
views, respectively.
Figure 4 - Patient in the postoperative period of steel wire traction, photo in medial and lateral
views, respectively.
Figure 5 - Patient in the postoperative period of new steel wire traction, photo in medial and
lateral views, respectively.
Figure 5 - Patient in the postoperative period of new steel wire traction, photo in medial and
lateral views, respectively.
The time between the first intervention by the Plastic Surgery team and hospital discharge
was two weeks. Thus, the various surgical times for tissue traction and approximation
of the edges did not generate an extension of hospital stay.
The patient was followed up at the outpatient clinic for 12 months without suture
dehiscence, local aesthetic complaints, or other complications inherent to the proposed
treatment. He was satisfied with the final aesthetic result and was discharged from
the service.
DISCUSSION
Due to the significant increase in high-energy trauma in recent decades, mainly due
to motorcycle and car accidents, the number of complex fractures of extremities that
are difficult to close is increasing. Many of them require fasciotomy, which momentarily
becomes necessary, but can lead to difficulty in their primary suture, requiring flaps,
grafts, vacuum dressing, elastic sutures, or other means for closing the same.
The number of fasciotomies registered in the Public Health System (SUS) in the last
decade, 2009-2019, was 26,905 nationally, with 13,758 in the lower limbs6. Amid this, the plastic surgeon must have a range of alternatives to close fasciotomies.
Among them, we found intermittent traction with Kirschner and steel wires a cheap
method, easily reproducible by other surgeons, and of great value for this purpose.
This technique is a variation based on tissue expansion described by Neuman in 1956,
in which skin gain is obtained through slow and intermittent expansion7, by Bashir (1987)8 and Callanan & Macey (1997)9.
This expansion process can be explained by the phenomenon of mechanical drag, in which
the collagen fibers stretch parallel to the direction of the traction force, and the
fundamental substance, composed of mucopolysaccharides and tissue fluids, which, being
displaced, leads to a final result of increased of surface area10,11,12,13.
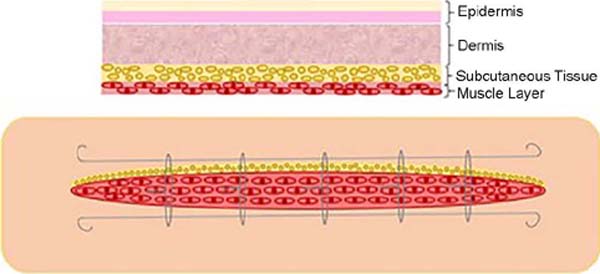
1-1.5mm Kirschner wires are passed through the healthy skin, being crossed parallel
to the edges of the wound in the dermal plane, approximately 5-7mm from the edge of
the wound, the remaining ends being cut and inverted, in order to support them and
not lose them between its ends. Then, grade 0 steel wires are introduced through both
Kirschner wires between the edges, and they are twisted and stretched to perform traction
to approximate the edges. The steel wires are inserted longitudinally and parallel
to the longest axis of the wound in the intradermal plane with a manually curved 18G
needle. The representative scheme of how the method is performed can be seen in Figure 6.
Figure 6 - Representative scheme of dermatotraction of the skin with Kirschner wires.
Figure 6 - Representative scheme of dermatotraction of the skin with Kirschner wires.
Subsequently, every 2 - 3 days, as well as weekly, depending on the patient’s clinical
status and tolerability, the steel wires are pulled again until the edges are ready
for primary closure; the procedure can be performed in the operating room under anesthesia
or intravenous sedation, or at the bedside with a locoregional blockade, depending
on the patient’s pain tolerance.
During the traction of the evaluated case, ischemic suffering of the skin or other
intercurrences were not evaluated, respecting the traction allowed according to the
elasticity of the skin presented at each procedure.
A meta-analysis conducted by Jauregui et al.14 compared the various types of fasciotomy closure described in the literature, including
conservative treatment (dressings only), partial skin grafts, elastic suture, gradual
approximation, dynamic dermatotraction (with specific devices) and negative pressure,
with the success rate defined as wound closure without the need for partial skin grafting.
Dynamic dermatotraction with specific devices (92.7%) and gradual approximation techniques
(92.4%) had the highest success rates. On the other hand, negative pressure dressings
obtained the worst results, with 78.1% of success14.
Elastic suture, another inexpensive and easily reproducible modality, can gradually
close complex wounds or fasciotomies. Raskin used it for the first time in 1993 to
approximate the borders of a post-compartment syndrome fasciotomy in an upper limb15.
The principle was based on the fixation with the tension of an interlaced elastic,
fixed to the edges of the skin, making a continuous tension of the skin, putting into
practice the concept of elasticity and skin compliance. The technique was revised
by Leite, in 1996, after observing the incidence of skin necrosis at the edges of
the wound when using the Raskin technique; he then proposed the fixation of the elastic
in the subcutaneous tissue and the superficial fascia, sparing the skin from the ischemic
event induced by the tensile force15.
Meanwhile, traction with steel wires can be controlled, performing traction as needed
so that vascularization, which is the limiting factor for skin traction in the various
methods, can be performed without compromising. Thickness, skin tension of the displaced
flap, skin pallor, and pain are the indicators to assess the ugly traction with the
steel wires.
Another point that should be considered is the procedure’s low cost. While steel wires
cost approximately R$5.00, other similar dermatotraction devices cost around US$500-1000,
and negative pressure dressings around US$96 a day10. Other techniques to achieve skin gain through intraoperative distension, described
by Hirshowitz et al.16, Stough et al.17, Lam et al.18, Bjarnesen et al.19 and others, require specialized equipment for their execution, being the former unavailable
in most hospitals and being more expensive7.
Unlike tissue grafting, dermatotraction requires a longer hospital stay, especially
in large wounds. In this case, dermatotraction was performed in a surgical center
under anesthetic blockade via spinal anesthesia in all procedures; however, depending
on the patient’s pain tolerance, it could be performed at the bedside.
We believe this method is valid mainly for patients needing to remain hospitalized
for reasons other than closing the fasciotomy, especially if we consider that vacuum
therapy cannot be performed at home in our country due to its unavailability in the
Public Health System (SUS). In cases where the early discharge of the patient is possible,
other methods, such as tissue grafting, should be considered.
CONCLUSION
The work demonstrates yet another highly valuable, safe, inexpensive, easily reproducible,
and low-morbid alternative to the arsenal of techniques available to surgeons for
closing fasciotomy and complex extremity injuries, often requiring prolonged hospitalization
and difficult therapeutic management.
1. Hospital de Clínicas de Curitiba, Cirurgia Plástica, Curitiba, Paraná, Brazil
2. Hospital do Trabalhador, Cirurgia Plástica, Curitiba, Paraná, Brazil
3. Universidade Federal do Paraná, Curso de Medicina, Curitiba, Paraná, Brazil
4. Universidade de Caxias do Sul, Curso de Medicina, Caxias do Sul, Rio Grande do
Sul, Brazil
Corresponding author: Antoninho José Tonatto Filho Rua Ubaldino do Amaral, 124/701, Bairro Alto da Gloria, Curitiba, PR, Brazil. Zip
code: 80060-190 E-mail: aj.tonatto@gmail.com